Ann Hepatobiliary Pancreat Surg.
2023 Feb;27(1):6-19. 10.14701/ahbps.22-045.
Procedural outcomes of laparoscopic caudate lobe resection: A systematic review and meta-analysis
- Affiliations
-
- 1Cardiff Liver Unit, University Hospital of Wales, Cardiff and Vale NHS Trust, Cardiff, United Kingdom
- 2Department of General Surgery, Glan Clwyd Hospital, Rhyl, United Kingdom
- 3Department of General Surgery, Royal Glamorgan Hospital, Cwm Taf University Health Board, Pontyclun, United Kingdom
- 4Undergraduate Department, School of Medicine, Cardiff University, Cardiff, United Kingdom
- 5Hepatobiliary and Pancreatic Surgery and Liver Transplant Unit, Queen Elizabeth Hospital, Birmingham, United Kingdom
- 6Department of Hepatobiliary and Pancreatic Surgery, Manchester Royal Infirmary Hospital, Manchester, United Kingdom
- KMID: 2539509
- DOI: http://doi.org/10.14701/ahbps.22-045
Abstract
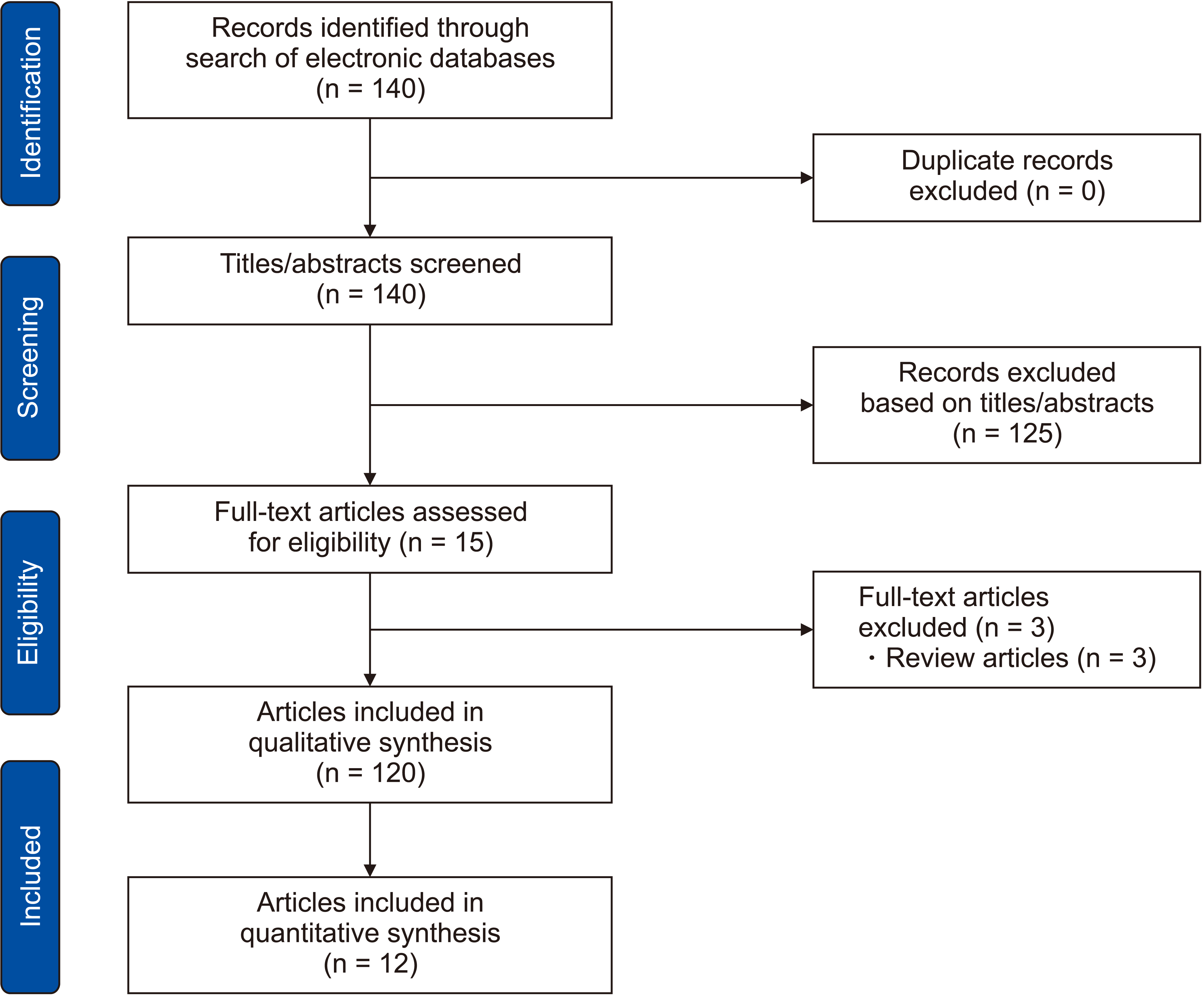
- A systematic review was conducted in compliance with PRISMA statement standards to identify all studies reporting outcomes of laparoscopic resection of benign or malignant lesions located in caudate lobe of liver. Pooled outcome data were calculated using random-effects models. A total of 196 patients from 12 studies were included. Mean operative time, volume of intraoperative blood loss, and length of hospital stay were 225 minutes (95% confidence interval [CI], 181–269 minutes), 134 mL (95% CI, 85–184 mL), and 7 days (95% CI, 5–9 days), respectively. The pooled risk of need for intraoperative transfusion was 2% (95% CI, 0%–5%). It was 3% (95% CI, 1%–6%) for conversion to open surgery, 6% (95% CI, 0%–19%) for need for intra-abdominal drain, 1% (95% CI, 0%–3%) for postoperative mortality, 2% (95% CI, 0%–4%) for biliary leakage, 2% (95% CI, 0%–4%) for intra-abdominal abscess, 1% (95% CI, 0%–4%) for biliary stenosis, 1% (95% CI, 0%–3%) for postoperative bleeding, 1% (95% CI, 0%–4%) for pancreatic fistula, 2% (95% CI, 1%–5%) for pulmonary complications, 1% (95% CI, 0%–4%) for paralytic ileus, and 1% (95% CI, 0%–4%) for need for reoperation. Although the available evidence is limited, the findings of the current study might be utilized for hypothesis synthesis in future studies. They can be used to inform surgeons and patients about estimated risks of perioperative complications until a higher level of evidence is available.
Keyword
Figure
Cited by 2 articles
-
Low versus standard central venous pressure during laparoscopic liver resection: A systematic review, meta-analysis and trial sequential analysis
Mina Stephanos, Christopher M. B. Stewart, Ameen Mahmood, Christopher Brown, Shahin Hajibandeh, Shahab Hajibandeh, Thomas Satyadas
Ann Hepatobiliary Pancreat Surg. 2024;28(2):115-124. doi: 10.14701/ahbps.23-137.Feasibility and safety of robotic radical resection for hilar cholangiocarcinoma in highly selected patients: A systematic review and meta-analysis with meta-regression
Shahab Hajibandeh, Shahin Hajibandeh, Thomas Satyadas
Ann Hepatobiliary Pancreat Surg. 2025;29(2):99-112. doi: 10.14701/ahbps.24-236.
Reference
-
1. Wang ZY, Chen QL, Sun LL, He SP, Luo XF, Huang LS, et al. 2019; Laparoscopic versus open major liver resection for hepatocellular carcinoma: systematic review and meta-analysis of comparative cohort studies. BMC Cancer. 19:1047. DOI: 10.1186/s12885-019-6240-x. PMID: 31694596. PMCID: PMC6833163.
Article2. Zhang XL, Liu RF, Zhang D, Zhang YS, Wang T. 2017; Laparoscopic versus open liver resection for colorectal liver metastases: a systematic review and meta-analysis of studies with propensity score-based analysis. Int J Surg. 44:191–203. DOI: 10.1016/j.ijsu.2017.05.073. PMID: 28583897.
Article3. Hajibandeh S, Hajibandeh S, Dave M, Tarazi M, Satyadas T. 2020; Laparoscopic versus open liver resection for tumors in the posterosuperior segments: a systematic review and meta-analysis. Surg Laparosc Endosc Percutan Tech. 30:93–105. DOI: 10.1097/SLE.0000000000000746. PMID: 31929396.
Article4. Kazaryan AM, Røsok BI, Marangos IP, Rosseland AR, Edwin B. 2011; Comparative evaluation of laparoscopic liver resection for posterosuperior and anterolateral segments. Surg Endosc. 25:3881–3889. DOI: 10.1007/s00464-011-1815-x. PMID: 21735326. PMCID: PMC3213339.
Article5. Koh YX, Lee SY, Chiow AKH, Kam JH, Goh BKP, Chan CY. 2017; Laparoscopic caudate lobe resection: navigating the technical challenge. Ann Laparosc Endosc Surg. 2:39. DOI: 10.21037/ales.2017.03.04.
Article6. Oh D, Kwon CH, Na BG, Lee KW, Cho WT, Lee SH, et al. 2016; Surgical techniques for totally laparoscopic caudate lobectomy. J Laparoendosc Adv Surg Tech A. 26:689–692. DOI: 10.1089/lap.2016.0161. PMID: 27599012.
Article7. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. 2009; The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 339:b2700. DOI: 10.1136/bmj.b2700. PMID: 19622552. PMCID: PMC2714672.
Article8. The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews. 2017. Checklist for Case Series [Internet]. Available from: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Case_Series2017_0.pdf. cited 2021 Sep 1. Adelaide: Joanna Briggs Institute.9. Petrie A, Bulman JS, Osborn JF. 2003; Further statistics in dentistry Part 8: systematic reviews and meta-analyses. Br Dent J. 194:73–78. DOI: 10.1038/sj.bdj.4809877. PMID: 12577072.
Article10. Chen KH, Jeng KS, Huang SH, Chu SH. 2013; Laparoscopic caudate hepatectomy for cancer--an innovative approach to the no-man's land. J Gastrointest Surg. 17:522–526. DOI: 10.1007/s11605-012-2115-z. PMID: 23297026.
Article11. Salloum C, Lahat E, Lim C, Doussot A, Osseis M, Compagnon P, et al. 2016; Laparoscopic isolated resection of caudate lobe (Segment 1): a safe and versatile technique. J Am Coll Surg. 222:e61–e66. DOI: 10.1016/j.jamcollsurg.2016.01.047. PMID: 27113524.
Article12. Araki K, Fuks D, Nomi T, Ogiso S, Lozano RR, Kuwano H, et al. 2016; Feasibility of laparoscopic liver resection for caudate lobe: technical strategy and comparative analysis with anteroinferior and posterosuperior segments. Surg Endosc. 30:4300–4306. DOI: 10.1007/s00464-016-4747-7. PMID: 26823056.
Article13. Chai S, Zhao J, Zhang Y, Xiang S, Zhang W. 2018; Arantius ligament suspension: a novel technique for retraction of the left lateral lobe liver during laparoscopic isolated caudate lobectomy. J Laparoendosc Adv Surg Tech A. 28:740–744. DOI: 10.1089/lap.2017.0572. PMID: 29232529.
Article14. Jin B, Jiang Z, Hu S, Du G, Shi B, Kong D, et al. 2018; Surgical technique and clinical analysis of twelve cases of isolated laparoscopic resection of the hepatic caudate lobe. Biomed Res Int. 2018:5848309. DOI: 10.1155/2018/5848309. PMID: 29568758. PMCID: PMC5820552.
Article15. Hayami S, Ueno M, Kawai M, Miyamoto A, Suzaki N, Hirono S, et al. 2019; Standardization of surgical procedures for laparoscopic Spiegel lobectomy: a single-institutional experience. Asian J Endosc Surg. 12:232–236. DOI: 10.1111/ases.12609. PMID: 30549230.
Article16. Cappelle M, Aghayan DL, van der Poel MJ, Besselink MG, Sergeant G, Edwin B, et al. 2020; A multicenter cohort analysis of laparoscopic hepatic caudate lobe resection. Langenbecks Arch Surg. 405:181–189. DOI: 10.1007/s00423-020-01867-2. PMID: 32239290.
Article17. Ding Z, Huang Y, Liu L, Xu B, Xiong H, Luo D, et al. 2020; Comparative analysis of the safety and feasibility of laparoscopic versus open caudate lobe resection. Langenbecks Arch Surg. 405:737–744. DOI: 10.1007/s00423-020-01928-6. PMID: 32648035.
Article18. Xu G, Tong J, Ji J, Wang H, Wu X, Jin B, et al. 2021; Laparoscopic caudate lobectomy: a multicenter, propensity score-matched report of safety, feasibility, and early outcomes. Surg Endosc. 35:1138–1147. DOI: 10.1007/s00464-020-07478-8. PMID: 32130488.
Article19. Peng Y, Liu F, Xu H, Guo S, Wei Y, Li B. 2021; Propensity score matching analysis for outcomes of laparoscopic versus open caudate lobectomy. ANZ J Surg. 91:E168–E173. DOI: 10.1111/ans.16512.
Article20. Ruzzenente A, Ciangherotti A, Aldrighetti L, Ettorre GM, De Carlis L, Ferrero A, et al. 2022; Technical feasibility and short-term outcomes of laparoscopic isolated caudate lobe resection: an IgoMILS (Italian Group of Minimally Invasive Liver Surgery) registry-based study. Surg Endosc. 36:1490–1499. DOI: 10.1007/s00464-021-08434-w. PMID: 33788031. PMCID: PMC8758628.
Article21. Ding Z, Liu L, Xu B, Huang Y, Xiong H, Luo D, et al. 2021; Safety and feasibility for laparoscopic versus open caudate lobe resection: a meta-analysis. Langenbecks Arch Surg. 406:1307–1316. DOI: 10.1007/s00423-020-02055-y. PMID: 33404881.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Total Laparoscopic Liver Resection for a Metastatic Lesion Located in the Caudate Lobe
- An Introduction of the Systematic Review and Meta-Analysis
- Short-term and Long-term Clinical Outcomes of Combined Caudate Lobectomy for Intrahepatic Cholangiocarcinoma Involving the Hepatic Hilus: A Propensity Score Analysis
- Comment on “Comparison of efficacy and safety between palonosetron and ondansetron to prevent postoperative nausea and vomiting in patients undergoing laparoscopic surgery: a systematic review and meta-analysis”
- Systematic Review and Meta-analysis in Digestive Cancer Research