J Stroke.
2023 Jan;25(1):119-125. 10.5853/jos.2022.02334.
Mechanical Thrombectomy for Acute Ischemic Stroke in Metastatic Cancer Patients: A Nationwide Cross-Sectional Analysis
- Affiliations
-
- 1Department of Neurology, Emory University School of Medicine, Atlanta, GA, USA
- 2Department of Neurology, Henry Ford Hospital, Detroit, MI, USA
- 3Department of Internal Medicine, CHI St. Alexius Health, Bismark, ND, USA
- 4Department of Internal Medicine, Lincoln Medical and Mental Health Center, New York, NY, USA
- 5Cardiovascular Medicine Department, University of Toledo, Toledo, OH, USA
- 6Department of Internal Medicine, Carle Foundation Hospital, Urbana, IL, USA
- 7Departments of Neurology and Neurosurgery, New York Medical College, Valhalla, NY, USA
- KMID: 2539064
- DOI: http://doi.org/10.5853/jos.2022.02334
Abstract
- Background and Purpose
Mechanical thrombectomy (MT) is the standard treatment for large vessel occlusion (LVO) acute ischemic stroke. Patients with active malignancy have an increased risk of stroke but were excluded from MT trials.
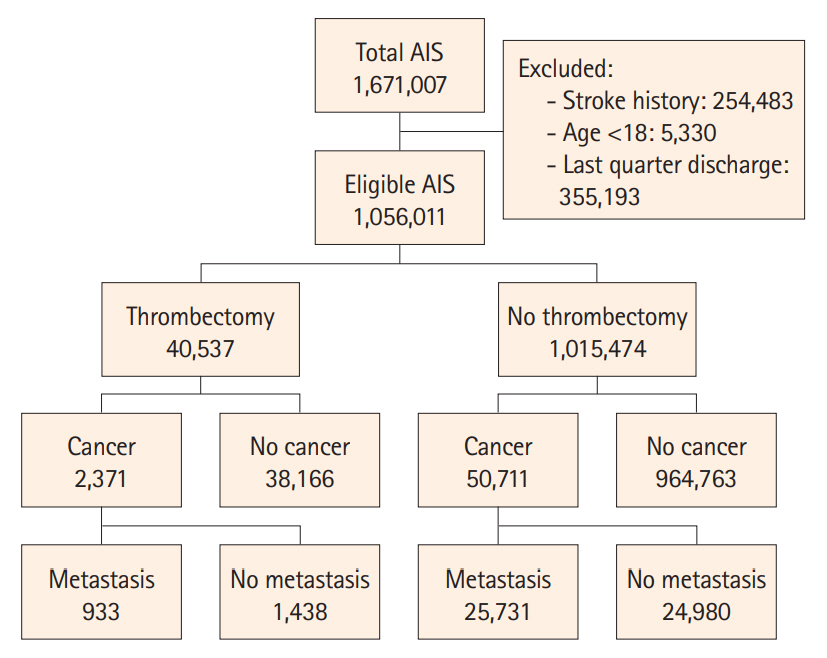
Methods
We searched the National Readmission Database for LVO patients treated with MT between 2016–2018 and compared the characteristics and outcomes of cancer-free patients to those with metastatic cancer (MC). Primary outcomes were all-cause in-hospital mortality and favorable outcome, defined as a routine discharge to home (regardless of whether home services were provided or not). Multivariate regression was used to adjust for confounders.
Results
Of 40,537 LVO patients treated with MT, 933 (2.3%) had MC diagnosis. Compared to cancer-free patients, MC patients were similar in age and stroke severity but had greater overall disease severity. Hospital complications that occurred more frequently in MC included pneumonia, sepsis, acute coronary syndrome, deep vein thrombosis, and pulmonary embolism (P<0.001). Patients with MC had similar rates of intracerebral hemorrhage (20% vs. 21%) but were less likely to receive tissue plasminogen activator (13% vs. 23%, P<0.001). In unadjusted analysis, MC patients as compared to cancer-free patients had a higher in-hospital mortality rate and were less likely to be discharged to home (36% vs. 42%, P=0.014). On multivariate regression adjusting for confounders, mortality was the only outcome that was significantly higher in the MC group than in the cancerfree group (P<0.001).
Conclusion
LVO patients with MC have higher mortality and more infectious and thrombotic complications than cancer-free patients. MT nonetheless can result in survival with good outcome in slightly over one-third of patients.
Keyword
Figure
Cited by 1 articles
-
Cancer-Associated Stroke: Thrombosis Mechanism, Diagnosis, Outcome, and Therapeutic Strategies
Ji Hoe Heo, Jaeseob Yun, Kwang Hyun Kim, Jae Wook Jung, Joonsang Yoo, Young Dae Kim, Hyo Suk Nam
J Stroke. 2024;26(2):164-178. doi: 10.5853/jos.2023.03279.
Reference
-
References
1. Graus F, Rogers LR, Posner JB. Cerebrovascular complications in patients with cancer. Medicine (Baltimore). 1985; 64:16–35.2. Casado-Naranjo I, Calle ML, Falcón A, Serrano A, Portilla JC, Ramírez-Moreno JM. Intravenous thrombolysis for acute stroke in patients with cancer. J Neurol Neurosurg Psychiatry. 2011; 82:1404–1405.3. Verschoof MA, Groot AE, de Bruijn SFTM, Roozenbeek B, van der Worp HB, Dippel DWJ, et al. Clinical outcome after endovascular treatment in patients with active cancer and ischemic stroke: a MR CLEAN registry substudy. Neurology. 2022; 98:e993. e1001.4. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.5. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.6. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.7. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.8. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.9. Lee D, Lee DH, Suh DC, Kwon HS, Jeong DE, Kim JG, et al. Intra-arterial thrombectomy for acute ischaemic stroke patients with active cancer. J Neurol. 2019; 266:2286–2293.10. Jung S, Jung C, Kim JH, Choi BS, Bae YJ, Sunwoo L, et al. Procedural and clinical outcomes of endovascular recanalization therapy in patients with cancer-related stroke. Interv Neuroradiol. 2018; 24:520–528.11. Cho BH, Yoon W, Kim JT, Choi KH, Kang KW, Lee JH, et al. Outcomes of endovascular treatment in acute ischemic stroke patients with current malignancy. Neurol Sci. 2020; 41:379–385.12. Sallustio F, Mascolo AP, Marrama F, Koch G, Alemseged F, Davoli A, et al. Safety and efficacy of reperfusion therapies for acute ischemic stroke patients with active malignancy. J Stroke Cerebrovasc Dis. 2019; 28:2287–2291.13. Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) [Internet]. Rockville, MD: Agency for Healthcare Research and Quality;2022. [cited 2022 October 10]. Available from: https://www.hcup-us.ahrq.gov/.14. Henderson T, Shepheard J, Sundararajan V. Quality of diagnosis and procedure coding in ICD-10 administrative data. Med Care. 2006; 44:1011–1019.15. Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Steinbeck BA, et al. All Patient Refined Diagnosis Related Groups (APR-DRGs): version 20.0. Methodology overview [Internet]. Wallingford, CT: 3M Health Information Systems;2003. [cited 2022 October 10]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf.16. Dicpinigaitis AJ, Sursal T, Morse CA, Briskin C, Dakay K, Kurian C, et al. Endovascular thrombectomy for treatment of acute ischemic stroke during pregnancy and the early postpartum period. Stroke. 2021; 52:3796–3804.17. Motataianu A, Maier S, Andone S, Barcutean L, Serban G, Bajko Z, et al. Ischemic stroke in patients with cancer: a retrospective cross-sectional study. J Crit Care Med (Targu Mures). 2021; 7:54–61.18. Navi BB, Iadecola C. Ischemic stroke in cancer patients: a review of an underappreciated pathology. Ann Neurol. 2018; 83:873–883.19. Grisold W, Oberndorfer S, Struhal W. Stroke and cancer: a review. Acta Neurol Scand. 2009; 119:1–16.20. Rickles FR, Edwards RL. Activation of blood coagulation in cancer: Trousseau’s syndrome revisited. Blood. 1983; 62:14–31.21. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.22. Kim SG, Hong JM, Kim HY, Lee J, Chung PW, Park KY, et al. Ischemic stroke in cancer patients with and without conventional mechanisms: a multicenter study in Korea. Stroke. 2010; 41:798–801.23. Murthy SB, Karanth S, Shah S, Shastri A, Rao CP, Bershad EM, et al. Thrombolysis for acute ischemic stroke in patients with cancer: a population study. Stroke. 2013; 44:3573–3576.24. Khorana AA, Francis CW, Culakova E, Fisher RI, Kuderer NM, Lyman GH. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol. 2006; 24:484–490.25. Selvik HA, Naess H, Kvistad CE. Intravenous thrombolysis in ischemic stroke patients with active cancer. Front Neurol. 2018; 9:811.26. Lee EJ, Bae J, Jeong HB, Lee EJ, Jeong HY, Yoon BW. Effectiveness of mechanical thrombectomy in cancer-related stroke and associated factors with unfavorable outcome. BMC Neurol. 2021; 21:57.27. Yoo J, Kim YD, Park H, Kim BM, Bang OY, Kim HC, et al. Immediate and long-term outcomes of reperfusion therapy in patients with cancer. Stroke. 2021; 52:2026–2034.28. Ciolli L, Bigliardi G, Ferraro D, Maffei S, Vandelli L, Dell’Acqua ML, et al. Efficacy of mechanical thrombectomy in patients with ischemic stroke and cancer. J Clin Neurosci. 2021; 91:20–22.29. Joshi KC, Grewal P, Beer-Furlan A, Vargas A, Osteraas N, Dafer R, et al. Endovascular thrombectomy for acute ischemic stroke in patients with cancer: a propensity-matched analysis. J Neurointerv Surg. 2022; 14:1161–1165.30. Oki S, Kawabori M, Echizenya S, Shimoda Y, Shimbo D, Osanai T, et al. Long-term clinical outcome and prognosis after thrombectomy in patients with concomitant malignancy. Front Neurol. 2020; 11:572589.31. Ren C, Xu G, Liu Y, Liu G, Wang J, Gao J. Effect of conscious sedation vs. general anesthesia on outcomes in patients undergoing mechanical thrombectomy for acute ischemic stroke: a prospective randomized clinical trial. Front Neurol. 2020; 11:170.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Endovascular Treatment of Acute Ischemic Stroke
- Paradigm Shift in Intra-Arterial Mechanical Thrombectomy for Acute Ischemic Stroke : A Review of Randomized Controlled Trials after 2015
- Differences in mechanical thrombectomy for acute ischemic stroke on weekdays versus nights/ weekends in a Japanese primary stroke core center
- Cell free DNA: A Novel Predictor of Neurological Outcome after Intravenous Thrombolysis and/or Mechanical Thrombectomy in Acute Ischemic Stroke Patients