J Stroke.
2023 Jan;25(1):81-91. 10.5853/jos.2022.03755.
Endovascular versus Medical Management of Acute Basilar Artery Occlusion: A Systematic Review and Meta-Analysis of the Randomized Controlled Trials
- Affiliations
-
- 1Departments of Radiology and Neurology, Boston Medical Center, Boston University Chobanian & Avedisian School of Medicine, Boston, MA, USA
- 2Department of Radiology, Aristotle University of Thessaloniki, Thessaloniki, Greece
- 3Stroke Center and Department of Neurology, Xuanwu Hospital of Capital Medical University, Beijing, China
- 4Department of Neurology and Stroke Center, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
- 5Department of Neurosurgery, Xuanwu Hospital of Capital Medical University, Beijing, China
- 6Interventional Neuroradiology, Beijing Tiantan Hospital, Beijing, China
- 7Medicine and Neurology, Melbourne Brain Centre at the Royal Melbourne Hospital, University of Melbourne, Parkville, VC, Australia
- 8Department of Neurology, The 903rd Hospital of The Chinese People’s Liberation Army, Hangzhou, China
- 9Neurology, Helsinki University Hospital, University of Helsinki, Helsinki, Finland
- 10Neurology, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 11Dresden Neurovascular Center, University Hospital Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
- 12Cooper Neurological Institute, Cooper University Hospital, Camden, NJ, USA
- 13Rhode Island Hospital, Brown University, Providence, RI, USA
- 14Amita Health and University of Illinois-Chicago, Chicago, IL, USA
- 15Department of Neurology, General Hospital of Northern Theatre Command, Shenyang, China
- 16Neurology, Heidelberg University Hospital, Heidelberg, Germany
- 17Neurology, Klinikum Ludwigshafen, Ludwigshafen, Germany
- 18Department of Neurology, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece
- 19Department of Neurology, Neurosurgery, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
- 20Department of Neurology, St. Antonius Hospital, Nieuwegein, the Netherlands
- KMID: 2539060
- DOI: http://doi.org/10.5853/jos.2022.03755
Abstract
- Background and Purpose
The optimal management of patients with acute basilar artery occlusion (BAO) is uncertain. We aimed to evaluate the safety and efficacy of endovascular thrombectomy (EVT) compared to medical management (MM) for acute BAO through a meta-analysis of randomized controlled trials (RCTs).
Methods
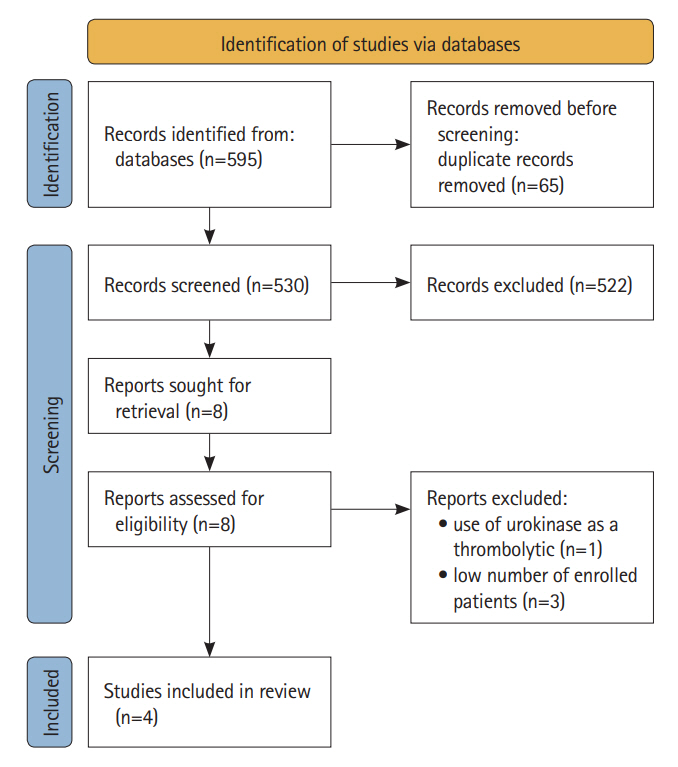
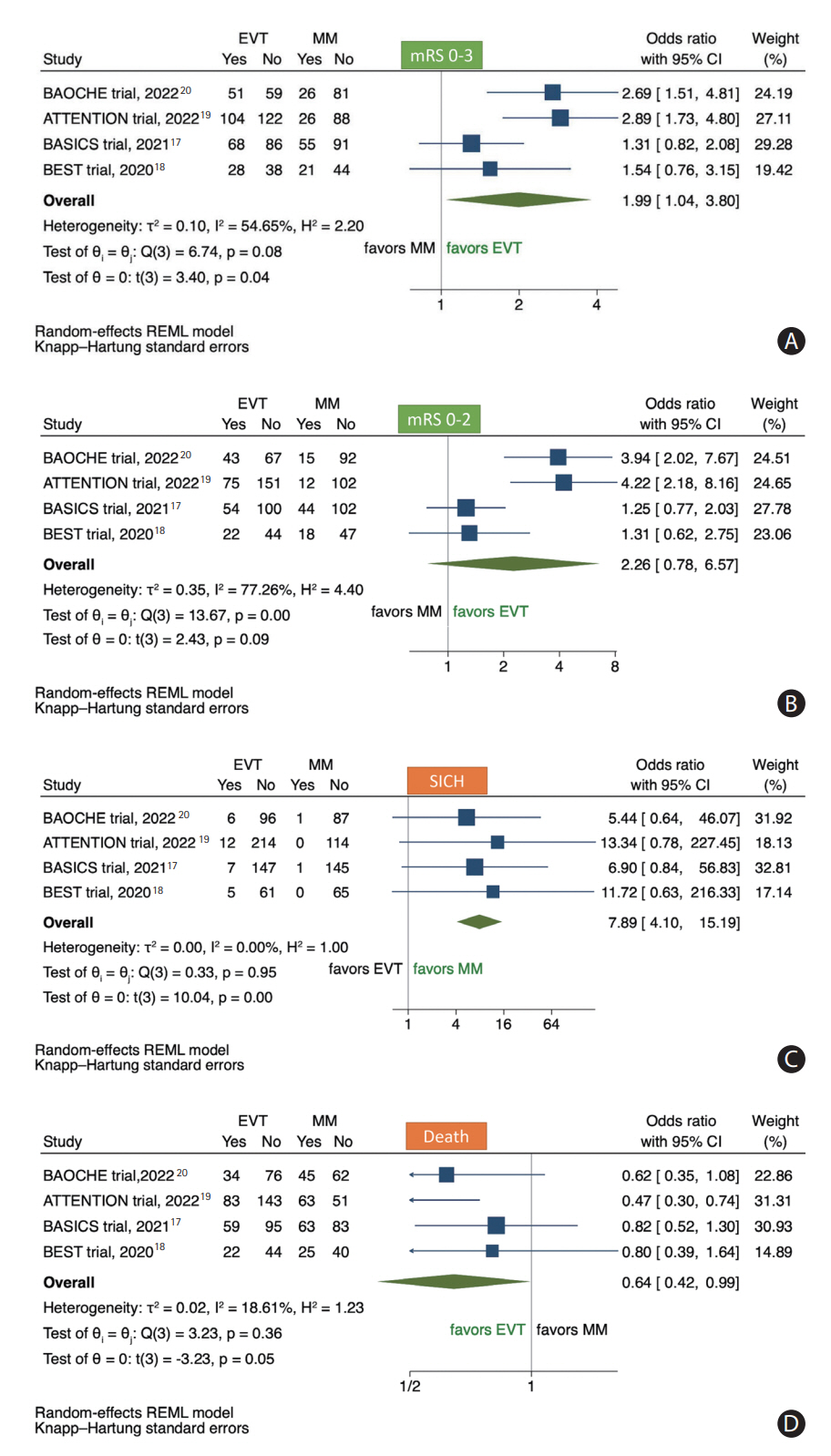
We performed a systematic review and meta-analysis of RCTs of patients with acute BAO. We analyzed the pooled effect of EVT compared to MM on the primary outcome (modified Rankin Scale [mRS] of 0–3 at 3 months), secondary outcome (mRS 0–2 at 3 months), symptomatic intracranial hemorrhage (sICH), and 3-month mortality rates. For each study, effect sizes were computed as odds ratios (ORs) with random effects and Mantel-Haenszel weighting.
Results
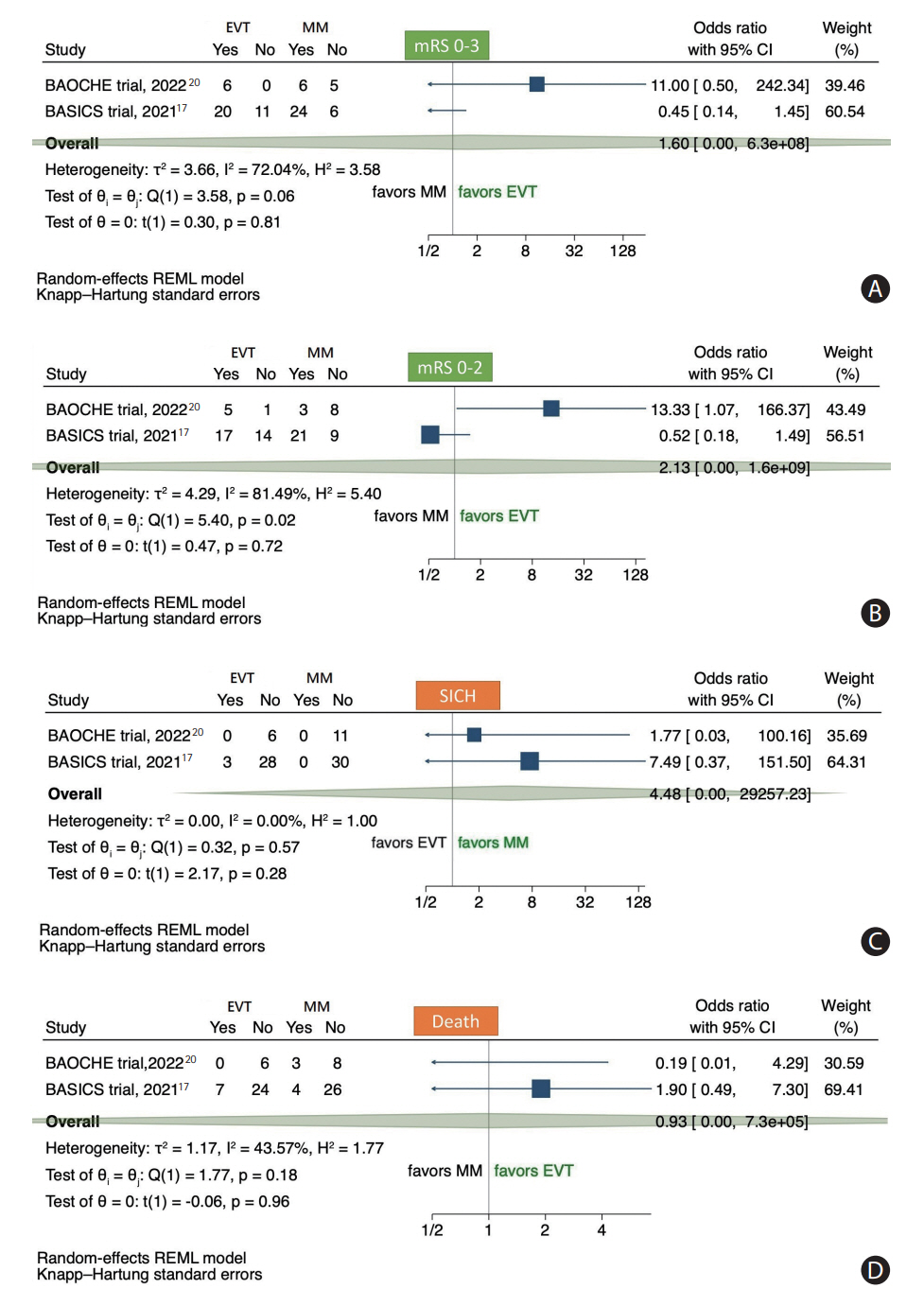
Four RCTs met inclusion criteria including 988 patients. There were higher odds of mRS of 0-3 at 90 days in the EVT versus MM group (45.1% vs. 29.1%, OR 1.99, 95% confidence interval [CI] 1.04–3.80; P=0.04). Patients receiving EVT had a higher sICH compared to MM (5.4% vs. 0.8%, OR 7.89, 95% CI 4.10–15.19; P<0.01). Mortality was lower in the EVT group (35.5% vs. 45.1%, OR 0.64, 95% CI 0.42–0.99; P=0.05). In an analysis of two trials with BAO patients and National Institutes of Health Stroke Scale (NIHSS) <10, there was no difference in 90-day outcomes between EVT versus MM.
Conclusion
In this systematic review and meta-analysis, EVT was associated with favorable outcome and decreased mortality in patients with BAO up to 24 hours from stroke symptoms compared to MM. The treatment effect in BAO patients with NIHSS <10 was less certain. Further studies are of interest to evaluate the efficacy of EVT in basilar occlusion patients with milder symptoms.
Figure
Cited by 1 articles
-
Cancer-Associated Stroke: Thrombosis Mechanism, Diagnosis, Outcome, and Therapeutic Strategies
Ji Hoe Heo, Jaeseob Yun, Kwang Hyun Kim, Jae Wook Jung, Joonsang Yoo, Young Dae Kim, Hyo Suk Nam
J Stroke. 2024;26(2):164-178. doi: 10.5853/jos.2023.03279.
Reference
-
References
1. Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; 372:11–20.2. Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; 372:1009–1018.3. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.4. Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–2306.5. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; 372:2285–2295.6. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.7. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.8. Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016; 15:1138–1147.9. Khoury NN, Darsaut TE, Ghostine J, Deschaintre Y, Daneault N, Durocher A, et al. Endovascular thrombectomy and medical therapy versus medical therapy alone in acute stroke: a randomized care trial. J Neuroradiol. 2017; 44:198–202.10. Drumm B, Banerjee S, Qureshi MM, Schonewille WJ, Klein P, Huo X, et al. Current opinions on optimal management of basilar artery occlusion: After the BEST of BASICS survey. Stroke Vasc Interv Neurol. 2022; 2:e000538.11. Huo X, Klein P, Drumm B, Chen Y, Qureshi MM, et al. Perceptions on basilar artery occlusion management in China versus other countries: analysis of the After the BEST of BASICS (ABBA) survey. J Stroke Cerebrovasc Dis. 2022; 31:106804.12. Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the basilar artery international cooperation study (BASICS): a prospective registry study. Lancet Neurol. 2009; 8:724–730.13. Dias FA, Alessio-Alves FF, Castro-Afonso LH, Cougo PT, Barreira CMA, Camilo MR, et al. Clinical outcomes of patients with acute basilar artery occlusion in Brazil: an observational study. J Stroke Cerebrovasc Dis. 2017; 26:2191–2198.14. Tao C, Qureshi AI, Yin Y, Li J, Li R, Xu P, et al. Endovascular treatment versus best medical management in acute basilar artery occlusion strokes: results from the ATTENTION multi-center registry. Circulation. 2022; 146:6–17.15. Writing Group for the BASILAR Group, Zi W, Qiu Z, Wu D, Li F, Liu H, Liu W, et al. Assessment of endovascular treatment for acute basilar artery occlusion via a nationwide prospective registry. JAMA Neurol. 2020; 77:561–573.16. Yu W, Higashida RT. Endovascular thrombectomy for acute basilar artery occlusion: latest findings and critical thinking on future study design. Transl Stroke Res. 2022; 13:913–922.17. Langezaal LCM, van der Hoeven EJRJ, Mont’Alverne FJA, de Carvalho JJF, Lima FO, Dippel DWJ, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. 2021; 384:1910–1920.18. Liu X, Dai Q, Ye R, Zi W, Liu Y, Wang H, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. 2020; 19:115–122.19. Tao C, Nogueira RG, Zhu Y, Sun J, Han H, Yuan G, et al. Trial of endovascular treatment of acute basilar-artery occlusion. N Engl J Med. 2022; 387:1361–1372.20. Jovin TG, Li C, Wu L, Wu C, Chen J, Jiang C, et al. Trial of thrombectomy 6 to 24 hours after stroke due to basilar-artery occlusion. N Engl J Med. 2022; 387:1373–1384.21. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009; 151:264–269.22. IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-SidikJonkman method for random effects meta-analysis is straight-forward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014; 14:25.23. Macleod MR, Davis SM, Mitchell PJ, Gerraty RP, Fitt G, Hankey GJ, et al. Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovasc Dis. 2005; 20:12–17.24. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 368:893–903.25. Nguyen TN, Strbian D. Endovascular therapy for stroke due to basilar artery occlusion: a BASIC challenge at BEST. Stroke. 2021; 52:3410–3413.26. Strbian D, Sairanen T, Silvennoinen H, Salonen O, Lindsberg PJ. Intravenous thrombolysis of basilar artery occlusion: thrombus length versus recanalization success. Stroke. 2014; 45:1733–1738.27. Puetz V, Lutsep HL, Nguyen TN. Endovascular therapy for basilar artery occlusion: among the first to conceptualize, last to prove. Stroke. 2023; Jan. 20. [Epub]. https://www.ahajournals.org/doi/10.1161/STROKEAHA.122.041645.28. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.29. Jovin TG, Nogueira RG, Lansberg MG, Demchuk AM, Martins SO, Mocco J, et al. Thrombectomy for anterior circulation stroke beyond 6 h from time last known well (AURORA): a systematic review and individual patient data meta-analysis. Lancet. 2022; 399:249–258.30. Alemseged F, Nguyen TN, Mont’Alverne F, Schonewille F, Nogueira RG. Endovascular therapy for basilar artery occlusion. Stroke. 2023; 54:(in Press).31. Strbian D, Sairanen T, Silvennoinen H, Salonen O, Kaste M, Lindsberg PJ. Thrombolysis of basilar artery occlusion: impact of baseline ischemia and time. Ann Neurol. 2013; 73:688–694.32. Kaesmacher J, Abdullayev N, Maamari B, Dobrocky T, Vynckier J, Piechowiak EI, et al. Safety and angiographic efficacy of intra-arterial fibrinolytics as adjunct to mechanical thrombectomy: results from the infinity registry. J Stroke. 2021; 23:91–102.33. Mitchell PJ, Gerraty RP, Donnan GA, Fitt G, Tress BM, Thomson KR, et al. Thrombolysis in the vertebrobasilar circulation: the Australian urokinase stroke trial. Cerebrovasc Dis. 1997; 7:94–99.34. Abdalkader M, Hu W. Endovascular therapy for stroke due to basilar artery occlusion: challenges and opportunities. J Neuroradiol. 2022; Dec. 14. [Epub]. https://doi.org/10.1016/j.neurad.2022.12.004.35. Alemseged F, Rocco A, Arba F, Schwabova JP, Wu T, Cavicchia L, et al. Posterior National Institutes of Health Stroke Scale improves prognostic accuracy in posterior circulation stroke. Stroke. 2022; 53:1247–1255.36. Nagel S, Bouslama M, Krause LU, Küpper C, Messer M, Petersen M, et al. Mechanical thrombectomy in patients with milder strokes and large vessel occlusions: a multicenter matched analysis. Stroke. 2018; 49:2391–2397.37. Guenego A, Dargazanli C, Weisenburger-Lile D, Gory B, Richard S, Ducroux C, et al. Thrombectomy for basilar artery occlusion with mild symptoms. World Neurosurg. 2021; 149:e400–e414.38. Katsanos AH, Safouris A, Nikolakopoulos S, Mavridis D, Goyal N, Psychogios MN, et al. Endovascular treatment for basilar artery occlusion: a systematic review and meta-analysis. Eur J Neurol. 2021; 28:2106–2110.39. Sun X, Tong X, Gao F, Lao H, Miao Z. Endovascular treatment for acute basilar artery occlusion: a single center retrospective observational study. BMC Neurol. 2019; 19:315.40. Turan TN, Zaidat OO, Gronseth GS, Chimowitz MI, Culebras A, Furlan AJ, et al. Stroke prevention in symptomatic large artery intracranial atherosclerosis practice advisory: report of the AAN guideline subcommittee. Neurology. 2022; 98:486–498.41. Klein P, Herning A, Drumm B, Raymond J, Abdalkader M, Siegler J, et al. Basilar artery occlusion thrombectomy technique: an international survey of practice patterns. Stroke Vasc Interv Neurol. 2022; Nov. 18. [Epub]. https://doi.org/10.1161/SVIN.122.000642.42. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Causes and Solutions of Endovascular Treatment Failure
- Introduction to systematic review and meta-analysis
- Intravenous Versus Intra-arterial Thrombolysis for Acute Ischemic Stroke Secondary to Basilar Artery Occlusion
- Endovascular Thrombectomy for Large Ischemic Strokes: A Living Systematic Review and Meta-Analysis of Randomized Trials
- Standard Versus Intensive Blood Pressure Control in Acute Ischemic Stroke Patients Successfully Treated With Endovascular Thrombectomy: A Systemic Review and Meta-Analysis of Randomized Controlled Trials