J Stroke.
2023 May;25(2):214-222. 10.5853/jos.2023.00752.
Endovascular Thrombectomy for Large Ischemic Strokes: A Living Systematic Review and Meta-Analysis of Randomized Trials
- Affiliations
-
- 1Department of Neurology, University of Chicago, Chicago, IL, USA
- 2Department of Neurological Sciences, University of Nebraska Medical Center, Omaha, NE, USA
- 3Faculty of Medicine, Al-Azhar University, Cairo, Egypt
- 4Department of Neurology, University of Connecticut, Farmington, CT, USA
- 5Department of Neurosurgery, Westchester Medical Center, Valhalla, NY, USA
- KMID: 2542472
- DOI: http://doi.org/10.5853/jos.2023.00752
Abstract
- Background and Purpose
New studies have shown that endovascular thrombectomy (EVT) is safe and effective for acute ischemic stroke (AIS) patients with large ischemic areas. The aim of our study is to conduct a living systematic review and meta-analysis of randomized trials comparing EVT versus medical management only.
Methods
We searched MEDLINE, Embase, and the Cochrane Library to identify randomized controlled trials (RCTs) comparing EVT versus medical management alone in AIS patients with large ischemic regions. We conducted our meta-analysis using fixed-effect models to compare functional independence, mortality, and symptomatic intracranial hemorrhage (sICH) between EVT and standard medical management only. We assessed the risk of bias using the Cochrane risk-of-bias tool and the certainty of evidence for each outcome using the Grading of Recommendations, Assessment, Development, and Evaluations approach.
Results
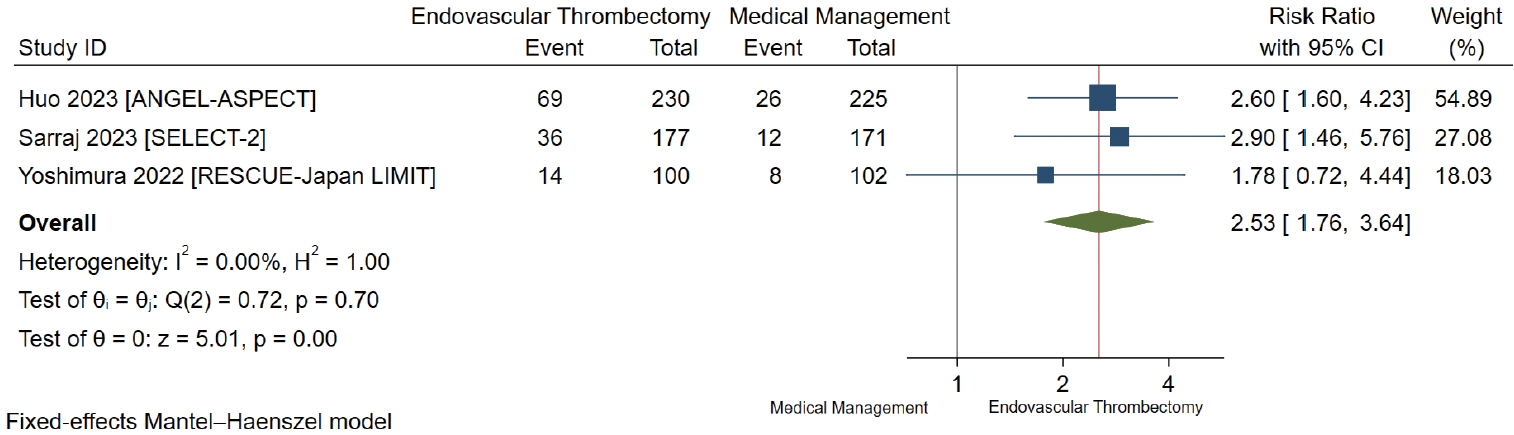
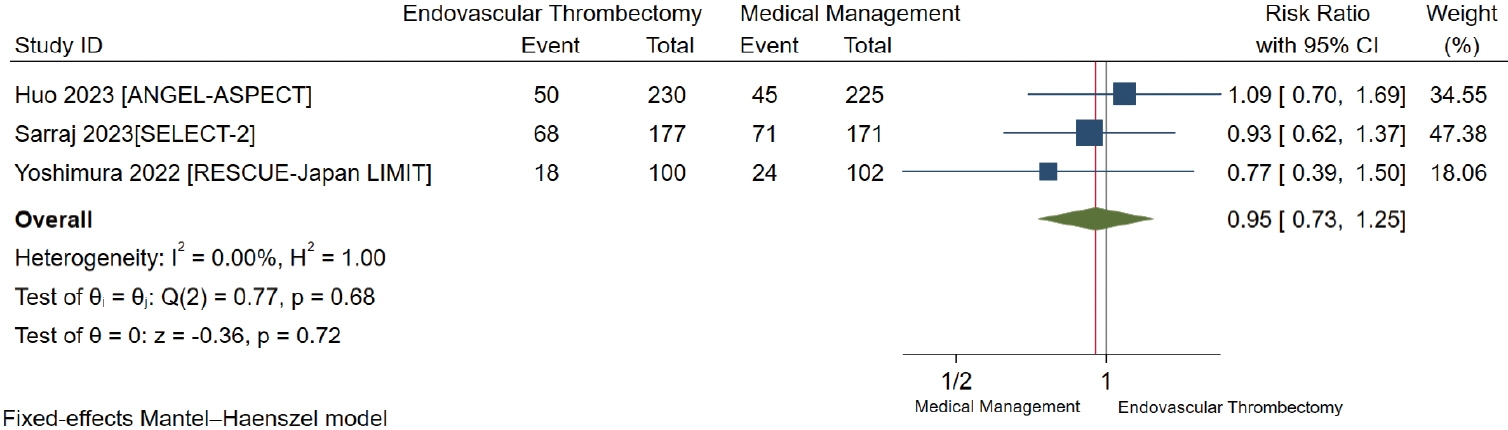
Of 14,513 citations, we included 3 RCTs with a total of 1,010 participants. We found low-certainty evidence of possibly a large increase in the proportion of patients with functional independence (risk difference [RD] 30.3%, 95% CI 15.0% to 52.3%), low-certainty evidence of possibly a small non-significant decrease in mortality (RD -0.7%, 95% CI -3.8% to 3.5%), and low-certainty evidence of possibly a small non-significant increase in sICH (RD 3.1%, 95% CI -0.3% to 9.8%) for AIS patients with large infarcts who underwent EVT compared to medical management only.
Conclusion
Low-certainty evidence shows that there is possibly a large increase in functional independence, a small non-significant decrease in mortality, and a small non-significant increase in sICH amongst AIS patients with large infarcts undergoing EVT compared to medical management only.
Keyword
Figure
Cited by 1 articles
-
Cancer-Associated Stroke: Thrombosis Mechanism, Diagnosis, Outcome, and Therapeutic Strategies
Ji Hoe Heo, Jaeseob Yun, Kwang Hyun Kim, Jae Wook Jung, Joonsang Yoo, Young Dae Kim, Hyo Suk Nam
J Stroke. 2024;26(2):164-178. doi: 10.5853/jos.2023.03279.
Reference
-
References
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.
Article2. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019; 11:535–538.
Article3. Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016; 15:1138–1147.
Article4. Cucchiara B, Kasner SE, Tanne D, Levine SR, Demchuk A, Messe SR, et al. Factors associated with intracerebral hemorrhage after thrombolytic therapy for ischemic stroke: pooled analysis of placebo data from the Stroke-Acute Ischemic NXY Treatment (SAINT) I and SAINT II trials. Stroke. 2009; 40:3067–3072.
Article5. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after largevessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article6. Sarraj A, Hassan AE, Savitz S, Sitton C, Grotta J, Chen P, et al. Outcomes of endovascular thrombectomy vs medical management alone in patients with large ischemic cores: a secondary analysis of the optimizing patient’s selection for endovascular treatment in acute ischemic stroke (SELECT) study. JAMA Neurol. 2019; 76:1147–1156.
Article7. Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med. 2023; 388:1272–1283.
Article8. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023; 388:1259–1271.
Article9. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med. 2022; 386:1303–1313.
Article10. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Hoboken, NJ: John Wiley & Sons;2019.11. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021; 134:178–189.12. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg Bleeding Classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.13. Sterne JAC, Savovic´ J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898.
Article14. Minozzi S, Dwan K, Borrelli F, Filippini G. Reliability of the revised Cochrane risk-of-bias tool for randomised trials (RoB2) improved with the use of implementation instruction. J Clin Epidemiol. 2022; 141:99–105.
Article15. Kakita H, Yoshimura S, Uchida K, Sakai N, Yamagami H, Morimoto T; RESCUE-Japan Registry 2 Investigators. Impact of endovascular therapy in patients with large ischemic core: subanalysis of recovery by endovascular salvage for cerebral ultra-acute embolism Japan registry 2. Stroke. 2019; 50:901–908.16. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014; 14:135.
Article17. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64:383–394.
Article18. Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. BMJ. 2015; 350:h870.
Article19. Wang X, Ye Z, Busse JW, Hill MD, Smith EE, Guyatt GH, et al. Endovascular thrombectomy with or without intravenous alteplase for acute ischemic stroke due to large vessel occlusion: a systematic review and meta-analysis of randomized trials. Stroke Vasc Neurol. 2022; 7:510–517.
Article20. Phan K, Saleh S, Dmytriw AA, Maingard J, Barras C, Hirsch JA, et al. Influence of ASPECTS and endovascular thrombectomy in acute ischemic stroke: a meta-analysis. J Neurointerv Surg. 2019; 11:664–669.
Article21. Safouris A, Palaiodimou L, Szikora I, Kargiotis O, Magoufis G, Psychogios K, et al. Endovascular treatment for anterior circulation large-vessel occlusion ischemic stroke with low ASPECTS: a systematic review and meta-analysis. Ther Adv Neurol Disord. 2022; 15:17562864221139632.
Article22. Kerleroux B, Janot K, Hak JF, Kaesmacher J, Hassen WB, Benzakoun J, et al. Mechanical thrombectomy in patients with a large ischemic volume at presentation: systematic review and meta-analysis. J Stroke. 2021; 23:358–366.
Article23. Yudkin JS, Lipska KJ, Montori VM. The idolatry of the surrogate. BMJ. 2011; 343:d7995.
Article24. Ganesh A, Luengo-Fernandez R, Wharton RM, Rothwell PM; Oxford Vascular Study. Ordinal vs dichotomous analyses of modified Rankin scale, 5-year outcome, and cost of stroke. Neurology. 2018; 91:e1951–e1960.
Article25. Schwamm LH. In stroke, when is a good outcome good enough? N Engl J Med. 2022; 386:1359–1363.
Article26. Ren Z, Huo X, Kumar J, Jadhav AP, Costalat V, Fiehler J, et al. Review of current large core volume stroke thrombectomy clinical trials: controversies and progress. Stroke Vasc Interv Neurol. 2022; 2:e000330.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy in Strokes with Large-Vessel Occlusion Beyond 6 Hours: A Pooled Analysis of Randomized Trials
- Intravenous Thrombolysis and Endovascular Thrombectomy in Acute Ischemic Stroke with Minor Symptom
- Endovascular Treatment of Acute Ischemic Stroke
- Introduction to systematic review and meta-analysis
- Standard Versus Intensive Blood Pressure Control in Acute Ischemic Stroke Patients Successfully Treated With Endovascular Thrombectomy: A Systemic Review and Meta-Analysis of Randomized Controlled Trials