J Stroke.
2023 Jan;25(1):2-15. 10.5853/jos.2022.03468.
Stroke in Women: A Review Focused on Epidemiology, Risk Factors, and Outcomes
- Affiliations
-
- 1Department of Neurology, Inha University School of Medicine, Incheon, Korea
- 2Department of Neurology, Wake Forest University School of Medicine, Winston Salem, NC, USA
- KMID: 2539054
- DOI: http://doi.org/10.5853/jos.2022.03468
Abstract
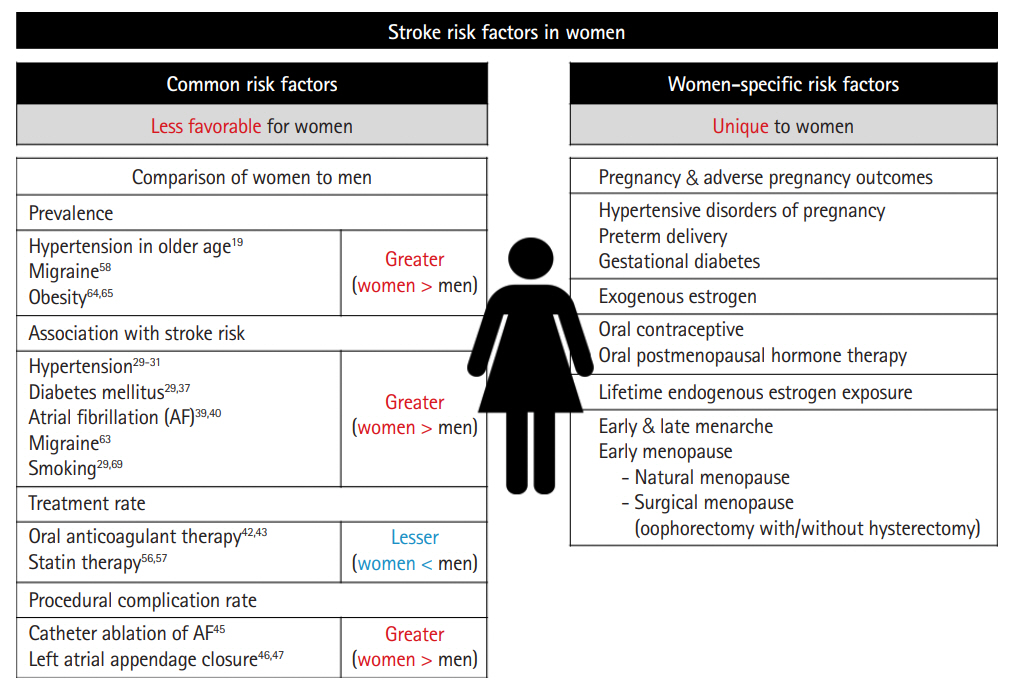
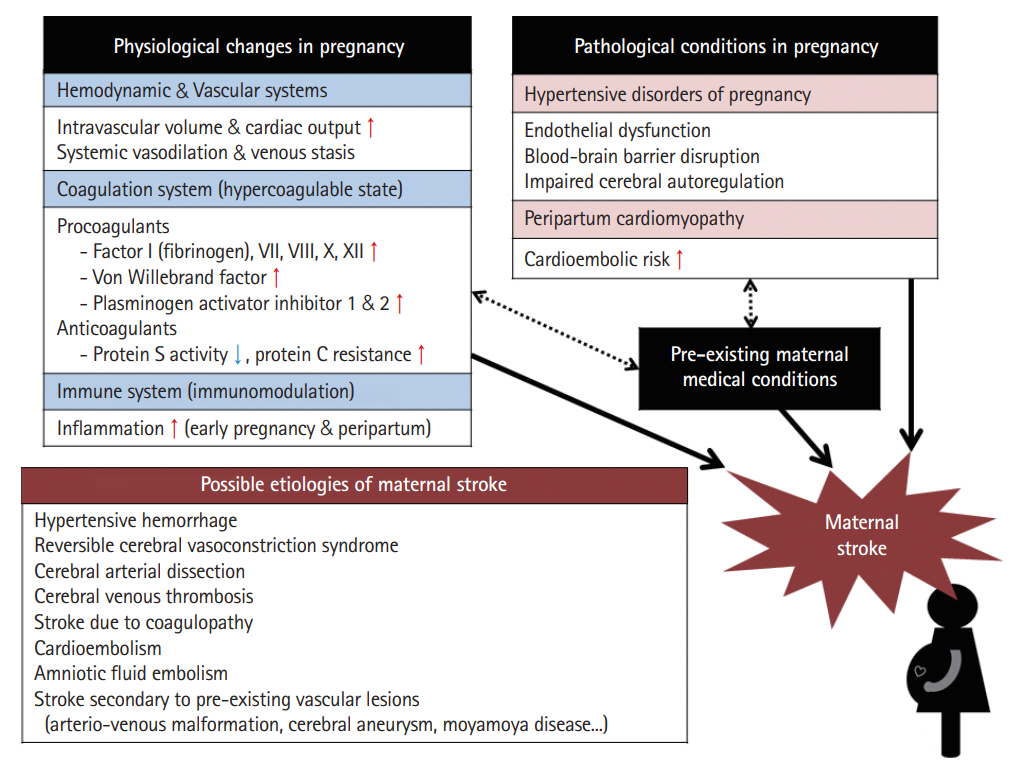
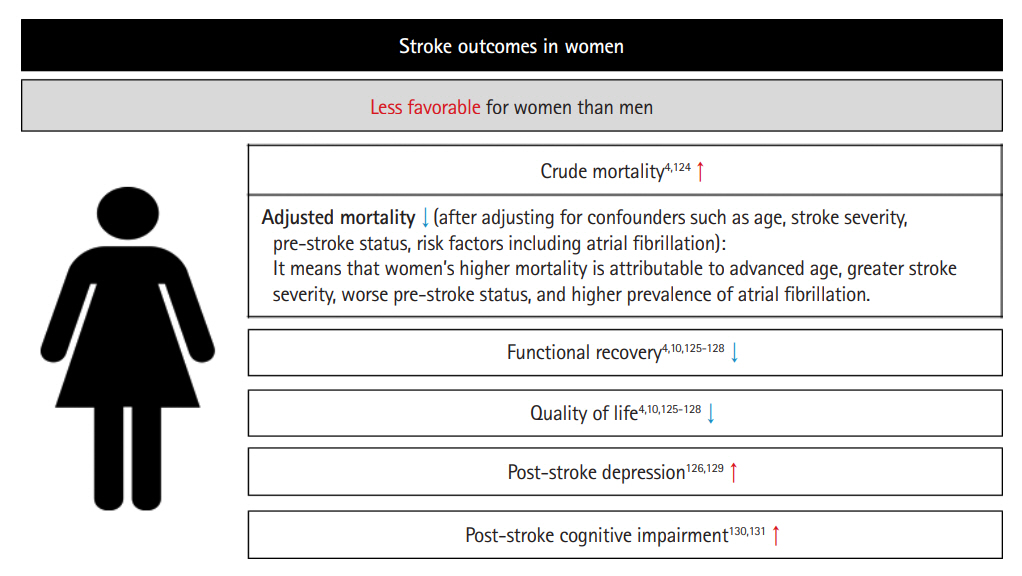
- Stroke is a particularly important issue for women. Women account for over half of all persons who experienced a stroke. The lifetime risk of stroke is higher in women than in men. In addition, women have worse stroke outcomes than men. Several risk factors have a higher association with stroke in women than in men, and women-specific risk factors that men do not have should be considered. This focused review highlights recent findings in stroke epidemiology, risk factors, and outcomes in women.
Figure
Reference
-
References
1. Feigin VL, Stark BA, Johnson CO, Roth GA, Bisignano C, Abady GG, et al. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021; 20:795–820.2. Feigin VL, Brainin M, Norrving B, Martins S, Sacco RL, Hacke W, et al. World Stroke Organization (WSO): global stroke fact sheet 2022. Int J Stroke. 2022; 17:18–29.3. Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB, et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke. 2006; 37:345–350.4. Xu M, Amarilla Vallejo A, Cantalapiedra Calvete C, Rudd A, Wolfe C, O’Connell MDL, et al. Stroke outcomes in women: a population-based cohort study. Stroke. 2022; 53:3072–3081.5. Appelros P, Stegmayr B, Terént A. Sex differences in stroke epidemiology: a systematic review. Stroke. 2009; 40:1082–1090.6. Madsen TE, Khoury JC, Leppert M, Alwell K, Moomaw CJ, Sucharew H, et al. Temporal trends in stroke incidence over time by sex and age in the GCNKSS. Stroke. 2020; 51:1070–1076.7. Vyas MV, Silver FL, Austin PC, Yu AYX, Pequeno P, Fang J, et al. Stroke incidence by sex across the lifespan. Stroke. 2021; 52:447–451.8. Leppert MH, Ho PM, Burke J, Madsen TE, Kleindorfer D, Sillau S, et al. Young women had more strokes than young men in a large, United States claims sample. Stroke. 2020; 51:3352–3355.9. Ekker MS, Verhoeven JI, Vaartjes I, van Nieuwenhuizen KM, Klijn CJM, de Leeuw FE. Stroke incidence in young adults according to age, subtype, sex, and time trends. Neurology. 2019; 92:e2444–e2454.10. Petrea RE, Beiser AS, Seshadri S, Kelly-Hayes M, Kase CS, Wolf PA. Gender differences in stroke incidence and poststroke disability in the Framingham Heart Study. Stroke. 2009; 40:1032–1037.11. Gardener H, Sacco RL, Rundek T, Battistella V, Cheung YK, Elkind MSV. Race and ethnic disparities in stroke incidence in the Northern Manhattan Study. Stroke. 2020; 51:1064–1069.12. Arnao V, Acciarresi M, Cittadini E, Caso V. Stroke incidence, prevalence and mortality in women worldwide. Int J Stroke. 2016; 11:287–301.13. Koton S, Sang Y, Schneider ALC, Rosamond WD, Gottesman RF, Coresh J. Trends in stroke incidence rates in older US adults: an update from the Atherosclerosis Risk in Communities (ARIC) cohort study. JAMA Neurol. 2020; 77:109–113.14. GBD 2016 Lifetime Risk of Stroke Collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018; 379:2429–2437.15. Cras TY, Bos D, Ikram MA, Vergouwen MDI, Dippel DWJ, Voortman T, et al. Determinants of the presence and size of intracranial aneurysms in the general population: the Rotterdam study. Stroke. 2020; 51:2103–2110.16. Fuentes AM, Stone McGuire L, Amin-Hanjani S. Sex differences in cerebral aneurysms and subarachnoid hemorrhage. Stroke. 2022; 53:624–633.17. Rehman S, Sahle BW, Chandra RV, Dwyer M, Thrift AG, Callisaya M, et al. Sex differences in risk factors for aneurysmal subarachnoid haemorrhage: systematic review and meta-analysis. J Neurol Sci. 2019; 406:116446.18. Zhou B, Carrillo-Larco RM, Danaei G, Riley LM, Paciorek CJ, Stevens GA, et al. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021; 398:957–980.19. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016; 134:441–450.20. Beaney T, Burrell LM, Castillo RR, Charchar FJ, Cro S, Damasceno A, et al. May Measurement Month 2018: a pragmatic global screening campaign to raise awareness of blood pressure by the International Society of Hypertension. Eur Heart J. 2019; 40:2006–2017.21. Redfern A, Peters SAE, Luo R, Cheng Y, Li C, Wang J, et al. Sex differences in the awareness, treatment, and control of hypertension in China: a systematic review with meta-analyses. Hypertens Res. 2019; 42:273–283.22. Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017; 289:1–8.23. Zhang Y, Moran AE. Trends in the prevalence, awareness, treatment, and control of hypertension among young adults in the United States, 1999 to 2014. Hypertension. 2017; 70:736–742.24. Sarganas G, Neuhauser HK. The persisting gender gap in hypertension management and control in Germany: 1998 and 2008-2011. Hypertens Res. 2016; 39:457–466.25. Choi HM, Kim HC, Kang DR. Sex differences in hypertension prevalence and control: analysis of the 2010-2014 Korea National Health and Nutrition Examination Survey. PLoS One. 2017; 12:e0178334.26. Zhou B, Danaei G, Stevens GA, Bixby H, Taddei C, CarrilloLarco RM, et al. Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet. 2019; 394:639–651.27. O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016; 388:761–775.28. Peters SA, Huxley RR, Woodward M. Comparison of the sex-specific associations between systolic blood pressure and the risk of cardiovascular disease: a systematic review and meta-analysis of 124 cohort studies, including 1.2 million individuals. Stroke. 2013; 44:2394–2401.29. Peters SAE, Carcel C, Millett ERC, Woodward M. Sex differences in the association between major risk factors and the risk of stroke in the UK Biobank cohort study. Neurology. 2020; 95:e2715–e2726.30. Madsen TE, Howard G, Kleindorfer DO, Furie KL, Oparil S, Manson JE, et al. Sex differences in hypertension and stroke risk in the REGARDS study: a longitudinal cohort study. Hypertension. 2019; 74:749–755.31. Ji H, Niiranen TJ, Rader F, Henglin M, Kim A, Ebinger JE, et al. Sex differences in blood pressure associations with cardiovascular outcomes. Circulation. 2021; 143:761–763.32. Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019; 157:107843.33. Peters SAE, Muntner P, Woodward M. Sex differences in the prevalence of, and trends in, cardiovascular risk factors, treatment, and control in the United States, 2001 to 2016. Circulation. 2019; 139:1025–1035.34. Franzini L, Ardigò D, Cavalot F, Miccoli R, Rivellese AA, Trovati M, et al. Women show worse control of type 2 diabetes and cardiovascular disease risk factors than men: results from the MIND.IT Study Group of the Italian Society of Diabetology. Nutr Metab Cardiovasc Dis. 2013; 23:235–241.35. Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010; 375:2215–2222.36. Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH Jr, Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2006; 37:2493–2498.37. Peters SA, Huxley RR, Woodward M. Diabetes as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 64 cohorts, including 775,385 individuals and 12,539 strokes. Lancet. 2014; 383:1973–1980.38. Gnatiuc L, Herrington WG, Halsey J, Tuomilehto J, Fang X, Kim HC, et al. Sex-specific relevance of diabetes to occlusive vascular and other mortality: a collaborative meta-analysis of individual data from 980 793 adults from 68 prospective studies. Lancet Diabetes Endocrinol. 2018; 6:538–546.39. Ko D, Rahman F, Schnabel RB, Yin X, Benjamin EJ, Christophersen IE. Atrial fibrillation in women: epidemiology, pathophysiology, presentation, and prognosis. Nat Rev Cardiol. 2016; 13:321–332.40. Emdin CA, Wong CX, Hsiao AJ, Altman DG, Peters SA, Woodward M, et al. Atrial fibrillation as risk factor for cardiovascular disease and death in women compared with men: systematic review and meta-analysis of cohort studies. BMJ. 2016; 352:h7013.41. Nielsen PB, Skjøth F, Overvad TF, Larsen TB, Lip GYH. Female sex is a risk modifier rather than a risk factor for stroke in atrial fibrillation: should we use a CHA2DS2-VA score rather than CHA2DS2-VASc? Circulation. 2018; 137:832–840.42. Thompson LE, Maddox TM, Lei L, Grunwald GK, Bradley SM, Peterson PN, et al. Sex differences in the use of oral anticoagulants for atrial fibrillation: a report from the national cardiovascular data registry (NCDR®) PINNACLE registry. J Am Heart Assoc. 2017; 6:e005801.43. Yong CM, Tremmel JA, Lansberg MG, Fan J, Askari M, Turakhia MP. Sex differences in oral anticoagulation and outcomes of stroke and intracranial bleeding in newly diagnosed atrial fibrillation. J Am Heart Assoc. 2020; 9:e015689.44. Avgil Tsadok M, Gagnon J, Joza J, Behlouli H, Verma A, Essebag V, et al. Temporal trends and sex differences in pulmonary vein isolation for patients with atrial fibrillation. Heart Rhythm. 2015; 12:1979–1986.45. Cheng X, Hu Q, Gao L, Liu J, Qin S, Zhang D. Sex-related differences in catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Europace. 2019; 21:1509–1518.46. Darden D, Duong T, Du C, Munir MB, Han FT, Reeves R, et al. Sex differences in procedural outcomes among patients undergoing left atrial appendage occlusion: insights from the NCDR LAAO registry. JAMA Cardiol. 2021; 6:1275–1284.47. Abusnina W, Latif A, Al-Abdouh A, Mostafa MR, Radaideh Q, Alshebani Y, et al. Sex differences in the clinical outcomes after left atrial appendage closure: a systematic review and meta-analysis. Cardiovasc Revasc Med. 2022; 41:29–34.48. Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. 2014; 12:28.49. Tirschwell DL, Smith NL, Heckbert SR, Lemaitre RN, Longstreth WT Jr, Psaty BM. Association of cholesterol with stroke risk varies in stroke subtypes and patient subgroups. Neurology. 2004; 63:1868–1875.50. Yaghi S, Elkind MS. Lipids and cerebrovascular disease: research and practice. Stroke. 2015; 46:3322–3328.51. Gu X, Li Y, Chen S, Yang X, Liu F, Li Y, et al. Association of lipids with ischemic and hemorrhagic stroke: a prospective cohort study among 267 500 Chinese. Stroke. 2019; 50:3376–3384.52. Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology. 2007; 68:556–562.53. Peters SA, Singhateh Y, Mackay D, Huxley RR, Woodward M. Total cholesterol as a risk factor for coronary heart disease and stroke in women compared with men: a systematic review and meta-analysis. Atherosclerosis. 2016; 248:123–131.54. Hong KS, Lee JS. Statins in acute ischemic stroke: a systematic review. J Stroke. 2015; 17:282–301.55. Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015; 385:1397–1405.56. Zhao M, Woodward M, Vaartjes I, Millett ERC, Klipstein-Grobusch K, Hyun K, et al. Sex differences in cardiovascular medication prescription in primary care: a systematic review and meta-analysis. J Am Heart Assoc. 2020; 9:e014742.57. Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, et al. Sex differences in the use of statins in community practice: patient and provider assessment of lipid management registry. Circ Cardiovasc Qual Outcomes. 2019; 12:e005562.58. Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, AlRaddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018; 17:954–976.59. Lee MJ, Lee C, Chung CS. The migraine–stroke connection. J Stroke. 2016; 18:146–156.60. Mahmoud AN, Mentias A, Elgendy AY, Qazi A, Barakat AF, Saad M, et al. Migraine and the risk of cardiovascular and cerebrovascular events: a meta-analysis of 16 cohort studies including 1 152 407 subjects. BMJ Open. 2018; 8:e020498.61. Sacco S, Ornello R, Ripa P, Pistoia F, Carolei A. Migraine and hemorrhagic stroke: a meta-analysis. Stroke. 2013; 44:3032–3038.62. Gaist D, González-Pérez A, Ashina M, Rodríguez LA. Migraine and risk of hemorrhagic stroke: a study based on data from general practice. J Headache Pain. 2014; 15:74.63. Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009; 339:b3914.64. Garawi F, Devries K, Thorogood N, Uauy R. Global differences between women and men in the prevalence of obesity: is there an association with gender inequality? Eur J Clin Nutr. 2014; 68:1101–1106.65. Fryar CD, Carroll MD, Afful J. Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018. Hyattsville, MD: NCHS Health E-Stats;2020. p. 1–7.66. Yatsuya H, Folsom AR, Yamagishi K, North KE, Brancati FL, Stevens J. Race- and sex-specific associations of obesity measures with ischemic stroke incidence in the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2010; 41:417–425.67. Kroll ME, Green J, Beral V, Sudlow CL, Brown A, Kirichek O, et al. Adiposity and ischemic and hemorrhagic stroke: prospective study in women and meta-analysis. Neurology. 2016; 87:1473–1481.68. Ng M, Freeman MK, Fleming TD, Robinson M, Dwyer-Lindgren L, Thomson B, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980-2012. JAMA. 2014; 311:183–192.69. Pan B, Jin X, Jun L, Qiu S, Zheng Q, Pan M. The relationship between smoking and stroke: a meta-analysis. Medicine (Baltimore). 2019; 98:e14872.70. Peters SA, Huxley RR, Woodward M. Smoking as a risk factor for stroke in women compared with men: a systematic review and meta-analysis of 81 cohorts, including 3,980,359 individuals and 42,401 strokes. Stroke. 2013; 44:2821–2828.71. Swartz RH, Cayley ML, Foley N, Ladhani NNN, Leffert L, Bushnell C, et al. The incidence of pregnancy-related stroke: a systematic review and meta-analysis. Int J Stroke. 2017; 12:687–697.72. Elgendy IY, Gad MM, Mahmoud AN, Keeley EC, Pepine CJ. Acute stroke during pregnancy and puerperium. J Am Coll Cardiol. 2020; 75:180–190.73. Karjalainen L, Tikkanen M, Rantanen K, Aarnio K, Korhonen A, Saaros A, et al. Stroke in pregnancy and puerperium: validated incidence trends with risk factor analysis in Finland 1987-2016. Neurology. 2021; 96:e2564–e2575.74. Ban L, Sprigg N, Abdul Sultan A, Nelson-Piercy C, Bath PM, Ludvigsson JF, et al. Incidence of first stroke in pregnant and nonpregnant women of childbearing age: a population-based cohort study from England. J Am Heart Assoc. 2017; 6:e004601.75. Silvis SM, Lindgren E, Hiltunen S, Devasagayam S, Scheres LJ, Jood K, et al. Postpartum period is a risk factor for cerebral venous thrombosis. Stroke. 2019; 50:501–503.76. Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014; 130:1003–1008.77. Stergiopoulos K, Shiang E, Bench T. Pregnancy in patients with pre-existing cardiomyopathies. J Am Coll Cardiol. 2011; 58:337–350.78. Porras JL, Yang W, Philadelphia E, Law J, Garzon-Muvdi T, Caplan JM, et al. Hemorrhage risk of brain arteriovenous malformations during pregnancy and puerperium in a North American cohort. Stroke. 2017; 48:1507–1513.79. Beighley A, Glynn R, Scullen T, Mathkour M, Werner C, Berry JF, et al. Aneurysmal subarachnoid hemorrhage during pregnancy: a comprehensive and systematic review of the literature. Neurosurg Rev. 2021; 44:2511–2522.80. Salehi Omran S, Parikh NS, Poisson S, Armstrong J, Merkler AE, Prabhu M, et al. Association between pregnancy and cervical artery dissection. Ann Neurol. 2020; 88:596–602.81. Brenner B. Haemostatic changes in pregnancy. Thromb Res. 2004; 114:409–414.82. Thornton P, Douglas J. Coagulation in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2010; 24:339–352.83. James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005; 106:509–516.84. Mor G, Cardenas I, Abrahams V, Guller S. Inflammation and pregnancy: the role of the immune system at the implantation site. Ann N Y Acad Sci. 2011; 1221:80–87.85. Boeldt DS, Bird IM. Vascular adaptation in pregnancy and endothelial dysfunction in preeclampsia. J Endocrinol. 2017; 232:R27–R44.86. Romero R, Gotsch F, Pineles B, Kusanovic JP. Inflammation in pregnancy: its roles in reproductive physiology, obstetrical complications, and fetal injury. Nutr Rev. 2007; 65(12 Pt 2):S194–S202.87. Kelly PJ, Lemmens R, Tsivgoulis G. Inflammation and stroke risk: a new target for prevention. Stroke. 2021; 52:2697–2706.88. Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, Saito S, et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension. 2018; 72:24–43.89. Ying W, Catov JM, Ouyang P. Hypertensive disorders of pregnancy and future maternal cardiovascular risk. J Am Heart Assoc. 2018; 7:e009382.90. Leffert LR, Clancy CR, Bateman BT, Bryant AS, Kuklina EV. Hypertensive disorders and pregnancy-related stroke: frequency, trends, risk factors, and outcomes. Obstet Gynecol. 2015; 125:124–131.91. Hung SK, Lee MS, Lin HY, Chen LC, Chuang CJ, Chew CH, et al. Impact of hypertensive disorders of pregnancy on the risk of stroke stratified by subtypes and follow-up time. Stroke. 2022; 53:338–344.92. Roberts JM, Hubel CA. The two stage model of preeclampsia: variations on the theme. Placenta. 2009; 30(Suppl A):S32–S37.93. Young BC, Levine RJ, Karumanchi SA. Pathogenesis of preeclampsia. Annu Rev Pathol. 2010; 5:173–192.94. McDermott M, Miller EC, Rundek T, Hurn PD, Bushnell CD. Preeclampsia: association with posterior reversible encephalopathy syndrome and stroke. Stroke. 2018; 49:524–530.95. Bello N, Rendon ISH, Arany Z. The relationship between preeclampsia and peripartum cardiomyopathy: a systematic review and meta-analysis. J Am Coll Cardiol. 2013; 62:1715–1723.96. Hoes MF, Arany Z, Bauersachs J, Hilfiker-Kleiner D, Petrie MC, Sliwa K, et al. Pathophysiology and risk factors of peripartum cardiomyopathy. Nat Rev Cardiol. 2022; 19:555–565.97. Arany Z, Elkayam U. Peripartum cardiomyopathy. Circulation. 2016; 133:1397–1409.98. Sliwa K, Petrie MC, van der Meer P, Mebazaa A, Hilfiker-Kleiner D, Jackson AM, et al. Clinical presentation, management, and 6-month outcomes in women with peripartum cardiomyopathy: an ESC EORP registry. Eur Heart J. 2020; 41:3787–3797.99. Liu S, Chan WS, Ray JG, Kramer MS, Joseph KS; Canadian Perinatal Surveillance System (Public Health Agency of Canada). Stroke and cerebrovascular disease in pregnancy: incidence, temporal trends, and risk factors. Stroke. 2019; 50:13–20.100. Meeks JR, Bambhroliya AB, Alex KM, Sheth SA, Savitz SI, Miller EC, et al. Association of primary intracerebral hemorrhage with pregnancy and the postpartum period. JAMA Netw Open. 2020; 3:e202769.101. Miller EC, Yaghi S, Boehme AK, Willey JZ, Elkind MS, Marshall RS. Mechanisms and outcomes of stroke during pregnancy and the postpartum period: a cross-sectional study. Neurol Clin Pract. 2016; 6:29–39.102. Maragkos GA, Ascanio LC, Chida K, Boone MD, Ogilvy CS, Thomas AJ, et al. Moyamoya disease in pregnancy: a systematic review. Acta Neurochir (Wien). 2018; 160:1711–1719.103. Uebing A, Steer PJ, Yentis SM, Gatzoulis MA. Pregnancy and congenital heart disease. BMJ. 2006; 332:401–406.104. Connolly C, O’Donoghue K, Doran H, McCarthy FP. Infective endocarditis in pregnancy: case report and review of the literature. Obstet Med. 2015; 8:102–104.105. Woo YS, Hong SC, Park SM, Cho KH. Ischemic stroke related to an amniotic fluid embolism during labor. J Clin Neurosci. 2015; 22:767–768.106. Greer IA. Pregnancy complicated by venous thrombosis. N Engl J Med. 2015; 373:540–547.107. de Havenon A, Delic A, Stulberg E, Sheibani N, Stoddard G, Hanson H, et al. Association of preeclampsia with incident stroke in later life among women in the Framingham Heart Study. JAMA Netw Open. 2021; 4:e215077.108. Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017; 10:e003497.109. Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ. 2020; 371:m3502.110. Crump C, Sundquist J, Sundquist K. Preterm delivery and long-term risk of stroke in women: a national cohort and cosibling study. Circulation. 2021; 143:2032–2044.111. Xu Z, Li Y, Tang S, Huang X, Chen T. Current use of oral contraceptives and the risk of first-ever ischemic stroke: a meta-analysis of observational studies. Thromb Res. 2015; 136:52–60.112. Xu Z, Yue Y, Bai J, Shen C, Yang J, Huang X, et al. Association between oral contraceptives and risk of hemorrhagic stroke: a meta-analysis of observational studies. Arch Gynecol Obstet. 2018; 297:1181–1191.113. Li F, Zhu L, Zhang J, He H, Qin Y, Cheng Y, et al. Oral contraceptive use and increased risk of stroke: a dose–response meta-analysis of observational studies. Front Neurol. 2019; 10:993.114. Chakhtoura Z, Canonico M, Gompel A, Thalabard JC, Scarabin PY, Plu-Bureau G. Progestogen-only contraceptives and the risk of stroke: a meta-analysis. Stroke. 2009; 40:1059–1062.115. Johansson T, Fowler P, Ek WE, Skalkidou A, Karlsson T, Johansson Å. Oral contraceptives, hormone replacement therapy, and stroke risk. Stroke. 2022; 53:3107–3115.116. Grodstein F, Manson JE, Stampfer MJ, Rexrode K. Postmenopausal hormone therapy and stroke: role of time since menopause and age at initiation of hormone therapy. Arch Intern Med. 2008; 168:861–866.117. Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women’s Health Initiative randomized trials. JAMA. 2013; 310:1353–1368.118. Nudy M, Chinchilli VM, Foy AJ. A systematic review and meta-regression analysis to examine the ‘timing hypothesis’ of hormone replacement therapy on mortality, coronary heart disease, and stroke. Int J Cardiol Heart Vasc. 2019; 22:123–131.119. Pinkerton JV. Hormone therapy for postmenopausal women. N Engl J Med. 2020; 382:446–455.120. Renoux C, Dell’aniello S, Garbe E, Suissa S. Transdermal and oral hormone replacement therapy and the risk of stroke: a nested case-control study. BMJ. 2010; 340:c2519.121. Mishra SR, Chung HF, Waller M, Dobson AJ, Greenwood DC, Cade JE, et al. Association between reproductive life span and incident nonfatal cardiovascular disease: a pooled analysis of individual patient data from 12 studies. JAMA Cardiol. 2020; 5:1410–1418.122. Poorthuis MH, Algra AM, Algra A, Kappelle LJ, Klijn CJ. Female-and male-specific risk factors for stroke: a systematic review and meta-analysis. JAMA Neurol. 2017; 74:75–81.123. Poorthuis MHF, Yao P, Chen Y, Guo Y, Shi L, Li L, et al. Risks of stroke and heart disease following hysterectomy and oophorectomy in Chinese premenopausal women. Stroke. 2022; 53:3064–3071.124. Phan HT, Blizzard CL, Reeves MJ, Thrift AG, Cadilhac D, Sturm J, et al. Sex differences in long-term mortality after stroke in the INSTRUCT (INternational STRoke oUtComes sTudy): a meta-analysis of individual participant data. Circ Cardiovasc Qual Outcomes. 2017; 10:e003436.125. Carcel C, Wang X, Sandset EC, Delcourt C, Arima H, Lindley R, et al. Sex differences in treatment and outcome after stroke: pooled analysis including 19,000 participants. Neurology. 2019; 93:e2170–e2180.126. Gall S, Phan H, Madsen TE, Reeves M, Rist P, Jimenez M, et al. Focused update of sex differences in patient reported outcome measures after stroke. Stroke. 2018; 49:531–535.127. Phan HT, Blizzard CL, Reeves MJ, Thrift AG, Cadilhac DA, Sturm J, et al. Sex differences in long-term quality of life among survivors after stroke in the INSTRUCT. Stroke. 2019; 50:2299–2306.128. Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008; 7:915–926.129. Poynter B, Shuman M, Diaz-Granados N, Kapral M, Grace SL, Stewart DE. Sex differences in the prevalence of post-stroke depression: a systematic review. Psychosomatics. 2009; 50:563–569.130. Dong L, Briceno E, Morgenstern LB, Lisabeth LD. Poststroke cognitive outcomes: sex differences and contributing factors. J Am Heart Assoc. 2020; 9:e016683.131. Bako AT, Potter T, Tannous J, Pan AP, Johnson C, Baig E, et al. Sex differences in post-stroke cognitive decline: a population-based longitudinal study of nationally representative data. PLoS One. 2022; 17:e0268249.132. Strong B, Pudar J, Thrift AG, Howard VJ, Hussain M, Carcel C, et al. Sex disparities in enrollment in recent randomized clinical trials of acute stroke: a meta-analysis. JAMA Neurol. 2021; 78:666–677.