Diabetes Metab J.
2023 Jan;47(1):140-146. 10.4093/dmj.2021.0322.
Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
- Affiliations
-
- 1Diabetes Center Bad Lauterberg, Bad Lauterberg, Germany
- 2Diabetes, Endocrinology and Metabolism Section, Department of Medicine I, St. Josef-Hospital, Katholisches Klinikum Bochum gGmbH, Ruhr University of Bochum, Bochum, Germany
- 3Department of Internal Medicine, Augusta-Hospital, Bochum, Germany
- KMID: 2538938
- DOI: http://doi.org/10.4093/dmj.2021.0322
Abstract
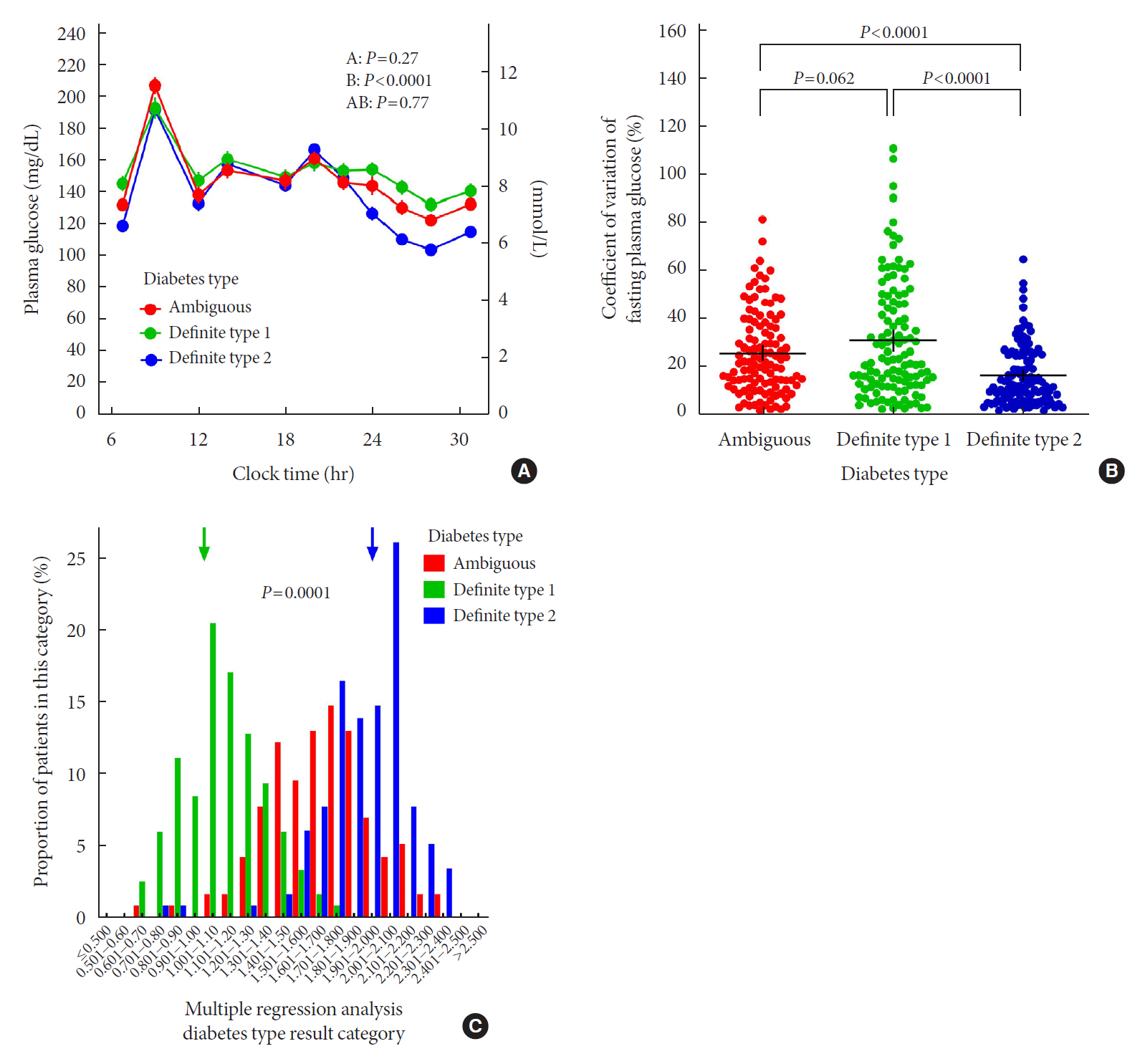
- In clinical practice, the distinction between type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) can be challenging, leaving patients with “ambiguous” diabetes type. Insulin-treated patients (n=115) previously diagnosed with T2DM had to be re-classified based on clinical phenotype and laboratory results, and were operationally defined as having an ambiguous diabetes type. They were compared against patients with definite T1DM and T2DM regarding 12 clinical and laboratory features typically different between diabetes types. Characteristics of patients with ambiguous diabetes type, representing approximately 6% of all patients with T1DM or T2DM seen at our specialized clinic, fell in between those of patients with definite T1DM and T2DM, both regarding individual features and with respect to a novel classification based on multi-variable regression analysis (P<0.0001). In conclusion, a substantial proportion of diabetes patients in a tertiary care centre presented with an “ambiguous” diabetes type. Their clinical characteristics fall in between those of definite T1DM or T2DM patients.
Keyword
Figure
Reference
-
1. Eisenbarth GS. Type I diabetes mellitus. A chronic autoimmune disease. N Engl J Med. 1986; 314:1360–8.2. Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009; 58:773–95.3. Becker B, Vogtmeier S, Terhoeven L, Vardarli I, Nauck MA. Characterization of glycaemic control with intensified insulin therapy in patients with T1DM and T2DM (abstract P 202). Diabetol Stoffwechs. 2011; 6:202.4. Rodbard D. Hypo- and hyperglycemia in relation to the mean, standard deviation, coefficient of variation, and nature of the glucose distribution. Diabetes Technol Ther. 2012; 14:868–76.
Article5. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care. 2017; 40(Suppl 1):S11–24.6. Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994; 17:961–9.
Article7. Becht FS, Walther K, Martin E, Nauck MA. Fasting C-peptide and related parameters characterizing insulin secretory capacity for correctly classifying diabetes type and for predicting insulin requirement in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes. 2016; 124:148–56.
Article8. Isermann B, Ritzel R, Zorn M, Schilling T, Nawroth PP. Autoantibodies in diabetes mellitus: current utility and perspectives. Exp Clin Endocrinol Diabetes. 2007; 115:483–90.
Article9. Tsirogianni A, Pipi E, Soufleros K. Specificity of islet cell autoantibodies and coexistence with other organ specific autoantibodies in type 1 diabetes mellitus. Autoimmun Rev. 2009; 8:687–91.
Article10. DeFronzo RA, Simonson D, Ferrannini E. Hepatic and peripheral insulin resistance: a common feature of type 2 (non-insulin-dependent) and type 1 (insulin-dependent) diabetes mellitus. Diabetologia. 1982; 23:313–9.
Article11. Corbin KD, Driscoll KA, Pratley RE, Smith SR, Maahs DM, Mayer-Davis EJ, et al. Obesity in type 1 diabetes: pathophysiology, clinical impact, and mechanisms. Endocr Rev. 2018; 39:629–63.
Article12. Cleland SJ, Fisher BM, Colhoun HM, Sattar N, Petrie JR. Insulin resistance in type 1 diabetes: what is ‘double diabetes’ and what are the risks? Diabetologia. 2013; 56:1462–70.
Article13. Park Y, Wintergerst KA, Zhou Z. Clinical heterogeneity of type 1 diabetes (T1D) found in Asia. Diabetes Metab Res Rev. 2017; 33:e2907.
Article14. Lee YB, Han K, Kim B, Jin SM, Lee SE, Jun JE, et al. High proportion of adult cases and prevalence of metabolic syndrome in type 1 diabetes mellitus population in Korea: a nationwide study. Diabetes Metab J. 2019; 43:76–89.
Article15. Zimmet PZ, Tuomi T, Mackay IR, Rowley MJ, Knowles W, Cohen M, et al. Latent autoimmune diabetes mellitus in adults (LADA): the role of antibodies to glutamic acid decarboxylase in diagnosis and prediction of insulin dependency. Diabet Med. 1994; 11:299–303.
Article16. Suzuki T, Takahashi K, Miyamoto S, Ueno H, Takekawa S, Yoshida A, et al. “Type 1 on type 2” diabetes mellitus: autoimmune type 1 diabetes superimposed on established type 2 diabetes. Intern Med. 2007; 46:1957–62.
Article17. Donath MY, Boni-Schnetzler M, Ellingsgaard H, Ehses JA. Islet inflammation impairs the pancreatic beta-cell in type 2 diabetes. Physiology (Bethesda). 2009; 24:325–31.18. Ahlqvist E, Storm P, Karajamaki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol. 2018; 6:361–9.
Article19. Leslie RD, Palmer J, Schloot NC, Lernmark A. Diabetes at the crossroads: relevance of disease classification to pathophysiology and treatment. Diabetologia. 2016; 59:13–20.
Article20. Skyler JS, Bakris GL, Bonifacio E, Darsow T, Eckel RH, Groop L, et al. Differentiation of diabetes by pathophysiology, natural history, and prognosis. Diabetes. 2017; 66:241–55.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pharmacothearpy of Adolescents with Diabetes
- Letter: Effects of Aerobic Exercise Intensity on Insulin Resistance in Patients with Type 2 Diabetes Mellitus (Korean Diabetes J 33(5):401-411, 2009)
- Summary of Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
- Genetic Diseases Associated with Diabetes Mellitus
- Response: Effects of Aerobic Exercise Intensity on Insulin Resistance in Patients with Type 2 Diabetes Mellitus (Korean Diabetes J 33:(5)401-411, 2009)