J Korean Neurosurg Soc.
2023 Jan;66(1):44-52. 10.3340/jkns.2022.0174.
Clinical Effect of Transverse Process Hook with K-Means Clustering-Based Stratification of Computed Tomography Hounsfield Unit at Upper Instrumented Vertebra Level in Adult Spinal Deformity Patients
- Affiliations
-
- 1Department of Neurosurgery, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Neurosurgery, National Health Insurance Service Hospital, Goyang, Korea
- 3Department of Neurosurgery, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2537847
- DOI: http://doi.org/10.3340/jkns.2022.0174
Abstract
Objective
: This study aimed to investigate the efficacy of transverse process (TP) hook system at the upper instrumented vertebra (UIV) for preventing screw pullout in adult spinal deformity surgery using the pedicle Hounsfield unit (HU) stratification based on K-means clustering.
Methods
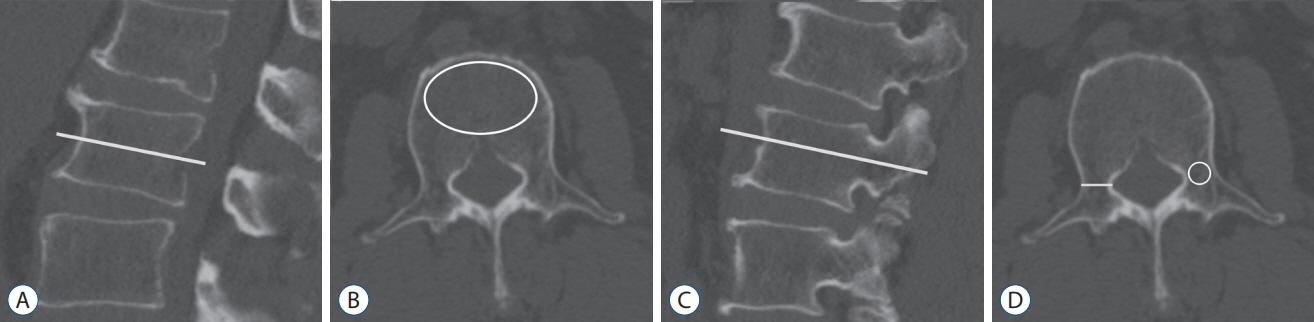
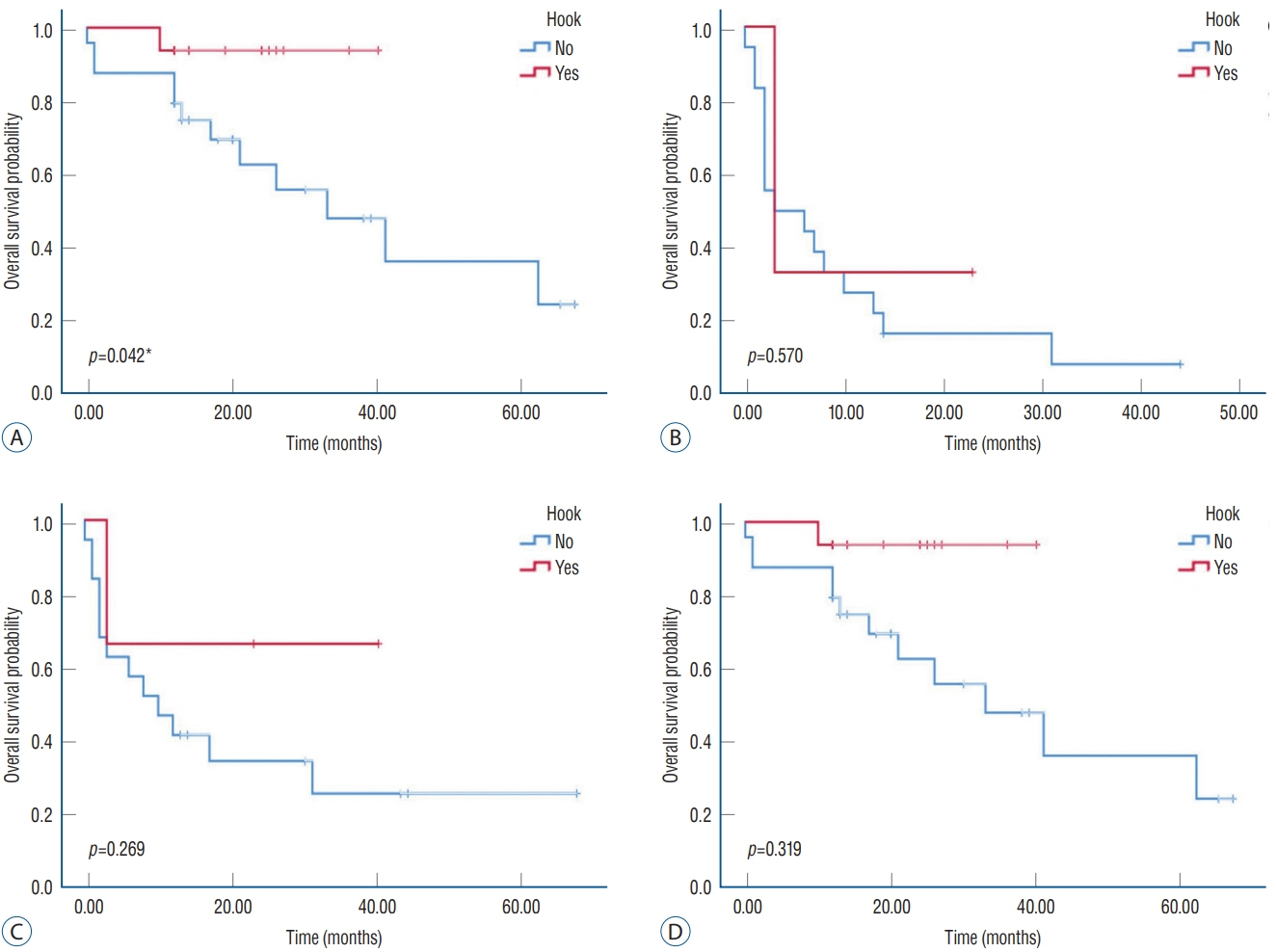
: We retrospectively reviewed 74 patients who underwent deformity correction surgery between 2011 and 2020 and were followed up for >12 months. Pre- and post-operative data were used to determine the incidence of screw pullout, UIV TP hook implementation, vertebral body HU, pedicle HU, and patient outcomes. Data was then statistically analyzed for assessment of efficacy and risk prediction using stratified HU at UIV level alongside the effect of the TP hook system.
Results
: The screw pullout rate was 36.4% (27/74). Perioperative radiographic parameters were not significantly different between the pullout and non-pullout groups. The vertebral body HU and pedicle HU were significantly lower in the pullout group. K-means clustering stratified the vertebral body HU ≥205.3, <137.2, and pedicle HU ≥243.43, <156.03. The pullout rate significantly decreases in patients receiving the hook system when the pedicle HU was from ≥156.03 to < 243.43 (p<0.05), but the difference was not statistically significant in the vertebra HU stratified groups and when pedicle HU was ≥243.43 or <156.03. The postoperative clinical outcomes improved significantly with the implementation of the hook system.
Conclusion
: The UIV hook provides better clinical outcomes and can be considered a preventative strategy for screw-pullout in the certain pedicle HU range.
Keyword
Figure
Reference
-
References
1. Bess RS, Lenke LG, Bridwell KH, Cheh G, Mandel S, Sides B. Comparison of thoracic pedicle screw to hook instrumentation for the treatment of adult spinal deformity. Spine (Phila Pa 1976). 32:555–561. 2007.2. Bredow J, Boese CK, Werner CM, Siewe J, Löhrer L, Zarghooni K, et al. Predictive validity of preoperative CT scans and the risk of pedicle screw loosening in spinal surgery. Arch Orthop Trauma Surg. 136:1063–1067. 2016.3. Buckens CF, Dijkhuis G, de Keizer B, Verhaar HJ, de Jong PA. Opportunistic screening for osteoporosis on routine computed tomography? An external validation study. Eur Radiol. 25:2074–2079. 2015.4. Cazzulino A, Gandhi R, Woodard T, Ackshota N, Janjua MB, Arlet V, et al. Soft Landing technique as a possible prevention strategy for proximal junctional failure following adult spinal deformity surgery. J Spine Surg. 7:26–36. 2021.5. Hassanzadeh H, Gupta S, Jain A, El Dafrawy MH, Skolasky RL, Kebaish KM. Type of anchor at the proximal fusion level has a significant effect on the incidence of proximal junctional kyphosis and outcome in adults after long posterior spinal fusion. Spine Deform. 1:299–305. 2013.6. Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976). 35:E465–E470. 2010.7. Hongo M, Gay RE, Zhao KD, Ilharreborde B, Huddleston PM, Berglund LJ, et al. Junction kinematics between proximal mobile and distal fused lumbar segments: biomechanical analysis of pedicle and hook constructs. Spine J. 9:846–853. 2009.8. Jain RK, Vokes T. Dual-energy X-ray absorptiometry. J Clin Densitom. 20:291–303. 2017.9. Line BG, Bess S, Lafage R, Lafage V, Schwab F, Ames C, et al. Effective prevention of proximal junctional failure in adult spinal deformity surgery requires a combination of surgical implant prophylaxis and avoidance of sagittal alignment overcorrection. Spine (Phila Pa 1976). 45:258–267. 2020.10. Mac-Thiong JM, Levasseur A, Parent S, Petit Y. The influence of proximal anchors on the risk of proximal junctional fracture in the osteoporotic spine: biomechanical comparison between pedicle screws and transverse process hooks. J Spinal Disord Tech. 27:E49–E54. 2014.11. Maruo K, Ha Y, Inoue S, Samuel S, Okada E, Hu SS, et al. Predictive factors for proximal junctional kyphosis in long fusions to the sacrum in adult spinal deformity. Spine (Phila Pa 1976). 38:E1469–E1476. 2013.12. Matsumura A, Namikawa T, Kato M, Oyama S, Hori Y, Yabu A, et al. Effect of different types of upper instrumented vertebrae instruments on proximal junctional kyphosis following adult spinal deformity surgery: pedicle screw versus transverse process hook. Asian Spine J. 12:622–631. 2018.13. Mi J, Li K, Zhao X, Zhao CQ, Li H, Zhao J. Vertebral body hounsfield units are associated with cage subsidence after transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Clin Spine Surg. 30:E1130–E1136. 2017.14. Nguyen HS, Shabani S, Patel M, Maiman D. Posterolateral lumbar fusion: relationship between computed tomography hounsfield units and symptomatic pseudoarthrosis. Surg Neurol Int. 6(Suppl 24):S611–S614. 2015.15. Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N. Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 158:588–595. 2013.16. Rosinski A, Odeh K, Ungurean V Jr, Leasure J, Kondrashov D. Nonpedicular fixation techniques for the treatment of spinal deformity: a systematic review. JBJS Rev. 8:e0150. 2020.17. Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 93:1057–1063. 2011.18. Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 34:1828–1833. 2009.19. Schwaiger BJ, Gersing AS, Baum T, Noël PB, Zimmer C, Bauer JS. Bone mineral density values derived from routine lumbar spine multidetector row CT predict osteoporotic vertebral fractures and screw loosening. AJNR Am J Neuroradiol. 35:1628–1633. 2014.20. Sensale M, Vendeuvre T, Schilling C, Grupp T, Rochette M, Dall’Ara E. Patient-specific finite element models of posterior pedicle screw fixation: effect of screw’s size and geometry. Front Bioeng Biotechnol. 9:643154. 2021.21. Shin HK, Koo HW, Kim KH, Yoon SW, Sohn MJ, Lee BJ. The usefulness of trabecular CT attenuation measurement at L4 level to predict screw loosening after degenerative lumbar fusion surgery: consider number of fused levels and postoperative sagittal balance. Spine (Phila Pa 1976). 47:745–753. 2022.22. Sumiya S, Fukushima K, Kurosa Y, Hirai T, Inose H, Yoshii T, et al. Comparative analysis of clinical factors associated with pedicle screw pull-out during or immediately after surgery between intraoperative conebeam computed tomography and postoperative computed tomography. BMC Musculoskelet Disord. 22:55. 2021.23. Thawrani DP, Glos DL, Coombs MT, Bylski-Austrow DI, Sturm PF. Transverse process hooks at upper instrumented vertebra provide more gradual motion transition than pedicle screws. Spine (Phila Pa 1976). 39:E826–E832. 2014.24. Wichmann JL, Booz C, Wesarg S, Bauer RW, Kerl JM, Fischer S, et al. Quantitative dual-energy CT for phantomless evaluation of cancellous bone mineral density of the vertebral pedicle: correlation with pedicle screw pull-out strength. Eur Radiol. 25:1714–1720. 2015.25. Xu F, Zou D, Li W, Sun Z, Jiang S, Zhou S, et al. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg Focus. 49:E10. 2020.26. Xu M, Yang J, Lieberman IH, Haddas R. Finite element method-based study of pedicle screw-bone connection in pullout test and physiological spinal loads. Med Eng Phys. 67:11–21. 2019.27. Yuan L, Zhang X, Zeng Y, Chen Z, Li W. Incidence, risk, and outcome of pedicle screw loosening in degenerative lumbar scoliosis patients undergoing long-segment fusion. Global Spine J. 2021; [Epub ahead of print].28. Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of hounsfield unit values for assessment of bone quality prior to spinal instrumentation: a review of current literature. Spine (Phila Pa 1976). 44:E239–E244. 2019.29. Zou D, Muheremu A, Sun Z, Zhong W, Jiang S, Li W. Computed tomography Hounsfield unit-based prediction of pedicle screw loosening after surgery for degenerative lumbar spine disease. J Neurosurg Spine. 32:716–721. 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiographic and Clinical Outcomes of Transverse Process Hook Placement at the Proximal Thoracic Upper Instrumented Vertebra in Adult Spinal Deformity Surgery
- Sagittal Section Hounsfield Units of the Upper Instrumented Vertebrae as a Predictor of Proximal Junctional Vertebral Fractures Following Adult Spinal Deformity Surgery
- Effect of Different Types of Upper Instrumented Vertebrae Instruments on Proximal Junctional Kyphosis Following Adult Spinal Deformity Surgery: Pedicle Screw versus Transverse Process Hook
- Study for hounsfield units in computed tomogram with jaw lesion
- Hounsfield units and vertebral bone quality score for predicting mechanical complications after adult spinal deformity surgery: a systematic review and meta-analysis