J Korean Assoc Oral Maxillofac Surg.
2022 Dec;48(6):371-381. 10.5125/jkaoms.2022.48.6.371.
Does platelet-rich fibrin increase bone regeneration in mandibular third molar extraction sockets?
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Obafemi Awolowo University Teaching Hospitals Complex, Ile-Ife, Nigeria
- 2Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Obafemi Awolowo University, Ile-Ife, Nigeria
- 3Institute of Public Health, Obafemi Awolowo University, Ile-Ife, Nigeria
- 4Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Lagos State University College of Medicine, Ikeja, Nigeria
- KMID: 2537563
- DOI: http://doi.org/10.5125/jkaoms.2022.48.6.371
Abstract
Objectives
This study determined the effect of platelet-rich fibrin (PRF) on extraction socket bone regeneration and assessed the patterns and determinants of bone regeneration after the surgical extraction of impacted mandibular third molars.
Materials and Methods
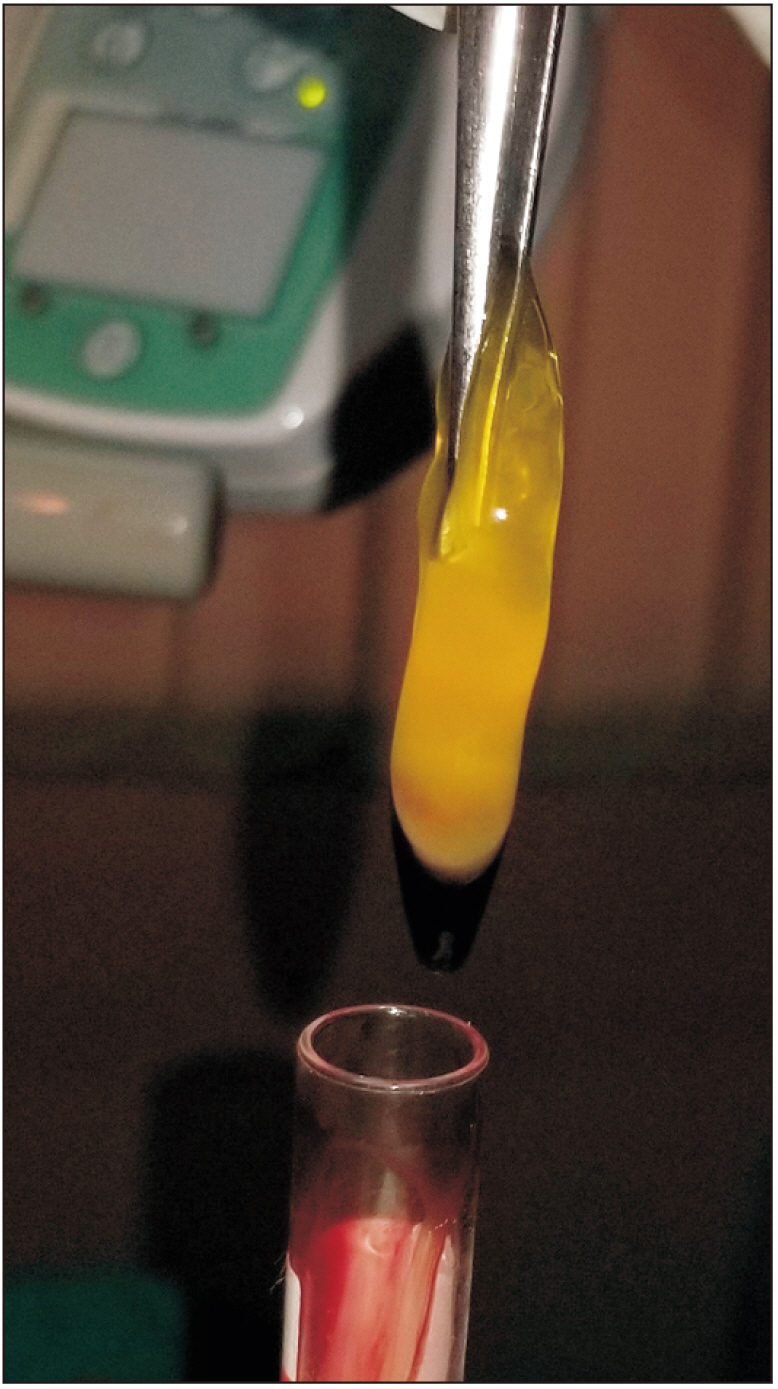
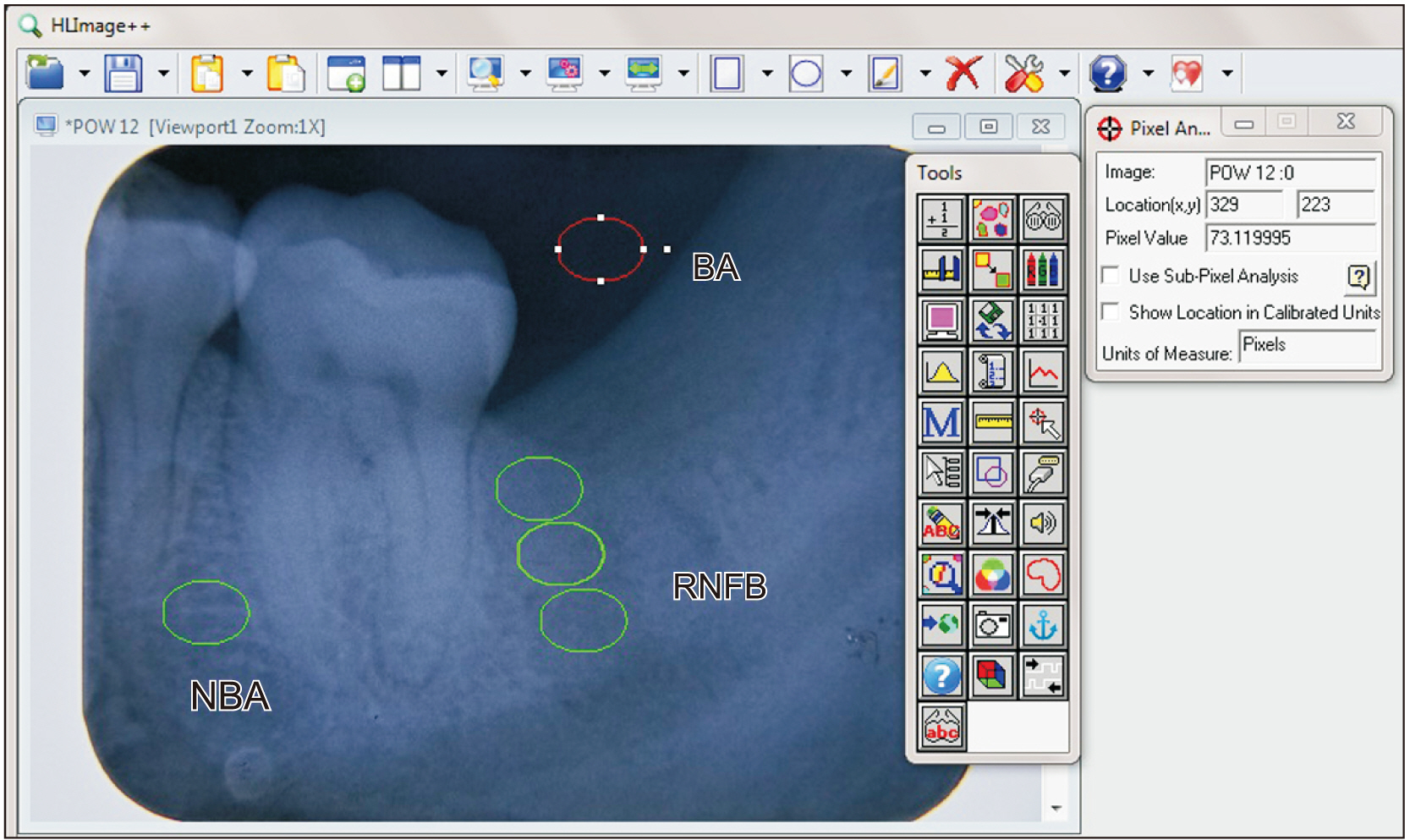
This prospective study randomly allocated 90 patients into two treatment groups: A PRF group (intervention group) and a non-PRF group (control group). After surgical extractions, the PRF group had PRF placed in the extraction socket and the socket was sutured, while the socket was only sutured in the non-PRF group. At postoperative weeks 1, 4, 8, and 12, periapical radiographs were obtained and HLImage software was used to determine the region of newly formed bone (RNFB) and the pattern of bone formation. The determinants of bone regeneration were assessed. Statistical significance was set at P<0.05.
Results
The percentage RNFB (RNFB%) was not significantly higher in the PRF group when compared with the non-PRF group at postoperative weeks 1, 4, 8, and 12 (P=0.188, 0.155, 0.132, and 0.219, respectively). Within the non-PRF group, the middle third consistently exhibited the highest bone formation while the least amount of bone formation was consistently observed in the cervical third. In the PRF group, the middle third had the highest bone formation, while bone formation at the apical third was smaller compared to the cervical third at the 8th week with this difference widening at the 12th week. The sex of the patient, type of impaction, and duration of surgery was significantly associated with percentage bone formation (P=0.041, 0.043, and 0.018, respectively).
Conclusion
Placement of PRF in extraction sockets increased socket bone regeneration. However, this finding was not statistically significant. The patient’s sex, type of impaction, and duration of surgery significantly influenced the percentage of bone formation.
Keyword
Figure
Cited by 1 articles
-
Effects of ascorbic acid augmented albumin platelet-rich fibrin on the wound healing activity of human gingival fibroblasts: an
in vitro trial
Manjiri Kulkarni, Sowmya NK, Gayathri GV, Triveni MG
J Korean Assoc Oral Maxillofac Surg. 2024;50(4):206-215. doi: 10.5125/jkaoms.2024.50.4.206.
Reference
-
References
1. Srinivas B, Das P, Rana MM, Qureshi AQ, Vaidya KC, Ahmed Raziuddin SJ. 2018; Wound healing and bone regeneration in postextraction sockets with and without platelet-rich fibrin. Ann Maxillofac Surg. 8:28–34. https://doi.org/10.4103/ams.ams_153_17. DOI: 10.4103/ams.ams_153_17. PMID: 29963421. PMCID: PMC6018297.2. Devlin H, Sloan P. 2002; Early bone healing events in the human extraction socket. Int J Oral Maxillofac Surg. 31:641–5. https://doi.org/10.1054/ijom.2002.0292. DOI: 10.1054/ijom.2002.0292. PMID: 12521322.3. Santosh P. 2015; Impacted mandibular third molars: review of literature and a proposal of a combined clinical and radiological classification. Ann Med Health Sci Res. 5:229–34. https://doi.org/10.4103/2141-9248.160177. DOI: 10.4103/2141-9248.160177. PMID: 26229709. PMCID: PMC4512113.4. Peterson LJ. Peterson LJ, editor. 1998. Principles of management of impacted teeth. Contemporary oral and maxillofacial surgery. 3rd ed. Mosby;St. Louis (MO): p. 143–7. DOI: 10.1016/b978-0-323-09177-0.00009-8.5. Hashemipour MA, Tahmasbi-Arashlow M, Fahimi-Hanzaei F. 2013; Incidence of impacted mandibular and maxillary third molars: a radiographic study in a Southeast Iran population. Med Oral Patol Oral Cir Bucal. 18:e140–5. https://doi.org/10.4317/medoral.18028. DOI: 10.4317/medoral.18028. PMID: 23229243. PMCID: PMC3548634.6. Leung YY, Yeung AWK, Ismail IN, Wong NSM. 2020; Bone regeneration at the distal aspect of the adjacent second molar after lower third molar coronectomy: a long-term analysis. Int J Oral Maxillofac Surg. 49:1360–6. https://doi.org/10.1016/j.ijom.2020.03.016. DOI: 10.1016/j.ijom.2020.03.016. PMID: 32340909.7. Choukroun J, Adda F, Schoeffler C, Vervelle A. 2001; Une opportunité en paro-implantologie: le PRF. Implantodontie. 42:55–62. French.8. Naik B, Karunakar P, Jayadev M, Marshal VR. 2013; Role of platelet rich fibrin in wound healing: a critical review. J Conserv Dent. 16:284–93. https://doi.org/10.4103/0972-0707.114344. DOI: 10.4103/0972-0707.114344. PMID: 23956527. PMCID: PMC3740636.9. Lind M. 1998; Growth factor stimulation of bone healing. Effects on osteoblasts, osteomies, and implants fixation. Acta Orthop Scand Suppl. 283:2–37. DOI: 10.1080/17453674.1998.11744808. PMID: 9856074.10. Lundquist R, Dziegiel MH, Agren MS. 2008; Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen. 16:356–63. https://doi.org/10.1111/j.1524-475X.2007.00344.x. DOI: 10.1111/j.1524-475X.2007.00344.x. PMID: 18282265.11. Gassling VL, Açil Y, Springer IN, Hubert N, Wiltfang J. 2009; Platelet-rich plasma and platelet-rich fibrin in human cell culture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 108:48–55. https://doi.org/10.1016/j.tripleo.2009.02.007. DOI: 10.1016/j.tripleo.2009.02.007. PMID: 19451011.12. Blatt S, Thiem DGE, Pabst A, Al-Nawas B, Kämmerer PW. 2021; Does platelet-rich fibrin enhance the early angiogenetic potential of different bone substitute materials? An in vitro and in vivo analysis. Biomedicines. 9:61. https://doi.org/10.3390/biomedicines9010061. DOI: 10.3390/biomedicines9010061. PMID: 33435244. PMCID: PMC7827266.13. Chakravarthi S. 2017; Platelet rich fibrin in the management of established dry socket. J Korean Assoc Oral Maxillofac Surg. 43:160–5. https://doi.org/10.5125/jkaoms.2017.43.3.160. DOI: 10.5125/jkaoms.2017.43.3.160. PMID: 28770156. PMCID: PMC5529189.14. Baslarli O, Tumer C, Ugur O, Vatankulu B. 2015; Evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. Med Oral Patol Oral Cir Bucal. 20:e111–6. https://doi.org/10.4317/medoral.19999. DOI: 10.4317/medoral.19999. PMID: 25475771. PMCID: PMC4320413.15. Kumar N, Prasad K, Ramanujam L, Ranganath K, Dexith J, Chauhan A. 2015; Evaluation of treatment outcome after impacted mandibular third molar surgery with the use of autologous platelet-rich fibrin: a randomized controlled clinical study. J Oral Maxillofac Surg. 73:1042–9. https://doi.org/10.1016/j.joms.2014.11.013. DOI: 10.1016/j.joms.2014.11.013. PMID: 25659357.16. Ruga E, Gallesio C, Boffano P. 2011; Platelet-rich fibrin and piezoelectric surgery: a safe technique for the prevention of periodontal complications in third molar surgery. J Craniofac Surg. 22:1951–5. https://doi.org/10.1097/SCS.0b013e31822ea76b. DOI: 10.1097/SCS.0b013e31822ea76b. PMID: 21959479.17. Gürbüzer B, Pikdöken L, Tunali M, Urhan M, Küçükodaci Z, Ercan F. 2010; Scintigraphic evaluation of osteoblastic activity in extraction sockets treated with platelet-rich fibrin. J Oral Maxillofac Surg. 68:980–9. https://doi.org/10.1016/j.joms.2009.09.092. DOI: 10.1016/j.joms.2009.09.092. PMID: 20144497.18. Varghese MP, Manuel S, Kumar LKS. 2017; Potential for osseous regeneration of platelet-rich fibrin-a comparative study in mandibular third molar impaction sockets. J Oral Maxillofac Surg. 75:1322–9. https://doi.org/10.1016/j.joms.2017.01.035. DOI: 10.1016/j.joms.2017.01.035. PMID: 28249808.19. Alzahrani AA, Murriky A, Shafik S. 2017; Influence of platelet rich fibrin on post-extraction socket healing: a clinical and radiographic study. Saudi Dent J. 29:149–55. https://doi.org/10.1016/j.sdentj.2017.07.003. DOI: 10.1016/j.sdentj.2017.07.003. PMID: 29033524. PMCID: PMC5634795.20. dos Santos Canellas JV, da Costa RC, Breves RC, de Oliveira GP, da Silva Figueredo CM, Fischer RG, et al. 2020; Tomographic and histomorphometric evaluation of socket healing after tooth extraction using leukocyte- and platelet-rich fibrin: a randomized, single-blind, controlled clinical trial. J Craniomaxillofac Surg. 48:24–32. https://doi.org/10.1016/j.jcms.2019.11.006. DOI: 10.1016/j.jcms.2019.11.006. PMID: 31810848.21. Amler MH. 1977; The age factor in human extraction wound healing. J Oral Surg. 35:193–7. PMID: 264520.22. Amler MH. 1993; Age factor in human alveolar bone repair. J Oral Implantol. 19:138–42. PMID: 8246300.23. Haffner-Luntzer M, Fischer V, Ignatius A. 2021; Differences in fracture healing between female and male C57BL/6J mice. Front Physiol. 12:712494. https://doi.org/10.3389/fphys.2021.712494. DOI: 10.3389/fphys.2021.712494. PMID: 34434120. PMCID: PMC8381649.24. Bello SA, Adeyemo WL, Bamgbose BO, Obi EV, Adeyinka AA. 2011; Effect of age, impaction types and operative time on inflammatory tissue reactions following lower third molar surgery. Head Face Med. 7:8. https://doi.org/10.1186/1746-160X-7-8. DOI: 10.1186/1746-160X-7-8. PMID: 21527036. PMCID: PMC3114767.25. Osunde OD, Saheeb BD. 2015; Effect of age, sex and level of surgical difficulty on inflammatory complications after third molar surgery. J Maxillofac Oral Surg. 14:7–12. https://doi.org/10.1007/s12663-013-0586-4. DOI: 10.1007/s12663-013-0586-4. PMID: 25729220. PMCID: PMC4339341.26. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. 2006; Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 101:e37–44. https://doi.org/10.1016/j.tripleo.2005.07.008. DOI: 10.1016/j.tripleo.2005.07.008. PMID: 16504849.27. Célio-Mariano R, de Melo WM, Carneiro-Avelino C. 2012; Comparative radiographic evaluation of alveolar bone healing associated with autologous platelet-rich plasma after impacted mandibular third molar surgery. J Oral Maxillofac Surg. 70:19–24. https://doi.org/10.1016/j.joms.2011.03.028. DOI: 10.1016/j.joms.2011.03.028. PMID: 21778014.28. Haghighat A, Hekmatian E, Abdinian M, Sadeghkhani E. 2011; Radiographic evaluation of bone formation and density changes after mandibular third molar extraction: a 6 month follow up. Dent Res J (Isfahan). 8:1–5. PMID: 22132008. PMCID: PMC3177375.29. Singh A, Kohli M, Gupta N. 2012; Platelet rich fibrin: a novel approach for osseous regeneration. J Maxillofac Oral Surg. 11:430–4. https://doi.org/10.1007/s12663-012-0351-0. DOI: 10.1007/s12663-012-0351-0. PMID: 24293936. PMCID: PMC3485469.30. Dohan Ehrenfest DM, Doglioli P, de Peppo GM, Del Corso M, Charrier JB. 2010; Choukroun's platelet-rich fibrin (PRF) stimulates in vitro proliferation and differentiation of human oral bone mesenchymal stem cell in a dose-dependent way. Arch Oral Biol. 55:185–94. https://doi.org/10.1016/j.archoralbio.2010.01.004. DOI: 10.1016/j.archoralbio.2010.01.004. PMID: 20176344.31. Areewong K, Chantaramungkorn M, Khongkhunthian P. 2019; Platelet-rich fibrin to preserve alveolar bone sockets following tooth extraction: a randomized controlled trial. Clin Implant Dent Relat Res. 21:1156–63. https://doi.org/10.1111/cid.12846. DOI: 10.1111/cid.12846. PMID: 31647177.32. Sağlam AA. 2003; Effects of tube drain with primary closure technique on postoperative trismus and swelling after removal of fully impacted mandibular third molars. Quintessence Int. 34:143–7. PMID: 12666865.33. Rakprasitkul S, Pairuchvej V. 1997; Mandibular third molar surgery with primary closure and tube drain. Int J Oral Maxillofac Surg. 26:187–90. https://doi.org/10.1016/s0901-5027(97)80817-x. DOI: 10.1016/S0901-5027(97)80817-X. PMID: 9180228.34. Cheng H, Clymer JW, Po-Han Chen B, Sadeghirad B, Ferko NC, Cameron CG, et al. 2018; Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 229:134–44. https://doi.org/10.1016/j.jss.2018.03.022. DOI: 10.1016/j.jss.2018.03.022. PMID: 29936980.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reduction in post extraction waiting period for dental implant patients using plasma rich in growth factors: an in vivo study using cone-beam computed tomography
- Use of Platelet-Rich Fibrin in Oral and Maxillofacial Surgery
- Leukocyte platelet-rich fibrin in endodontic microsurgery: a report of 2 cases
- Use of platelet-rich fibrin and natural bone regeneration in regenerative surgery
- Clinical and Histopathological Study Using Platelet Rich Plasma and Bone Grafts in Extraction Sockets