J Korean Assoc Oral Maxillofac Surg.
2022 Dec;48(6):363-370. 10.5125/jkaoms.2022.48.6.363.
Efficacy of submucosal injection of hyaluronidase after mandibular third molar surgery: a randomized controlled trial
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Yonsei University College of Dentistry, Seoul, Korea
- 2Department of Oral and Maxillofacial Surgery, Private Clinic, Seoul, Korea
- KMID: 2537562
- DOI: http://doi.org/10.5125/jkaoms.2022.48.6.363
Abstract
Objectives
This study aimed to investigate the efficacy of postoperative submucosal injection of hyaluronidase (HUD) for reducing sequelae and quality of life (QOL) after mandibular third molar (M3M) surgery.
Materials and Methods
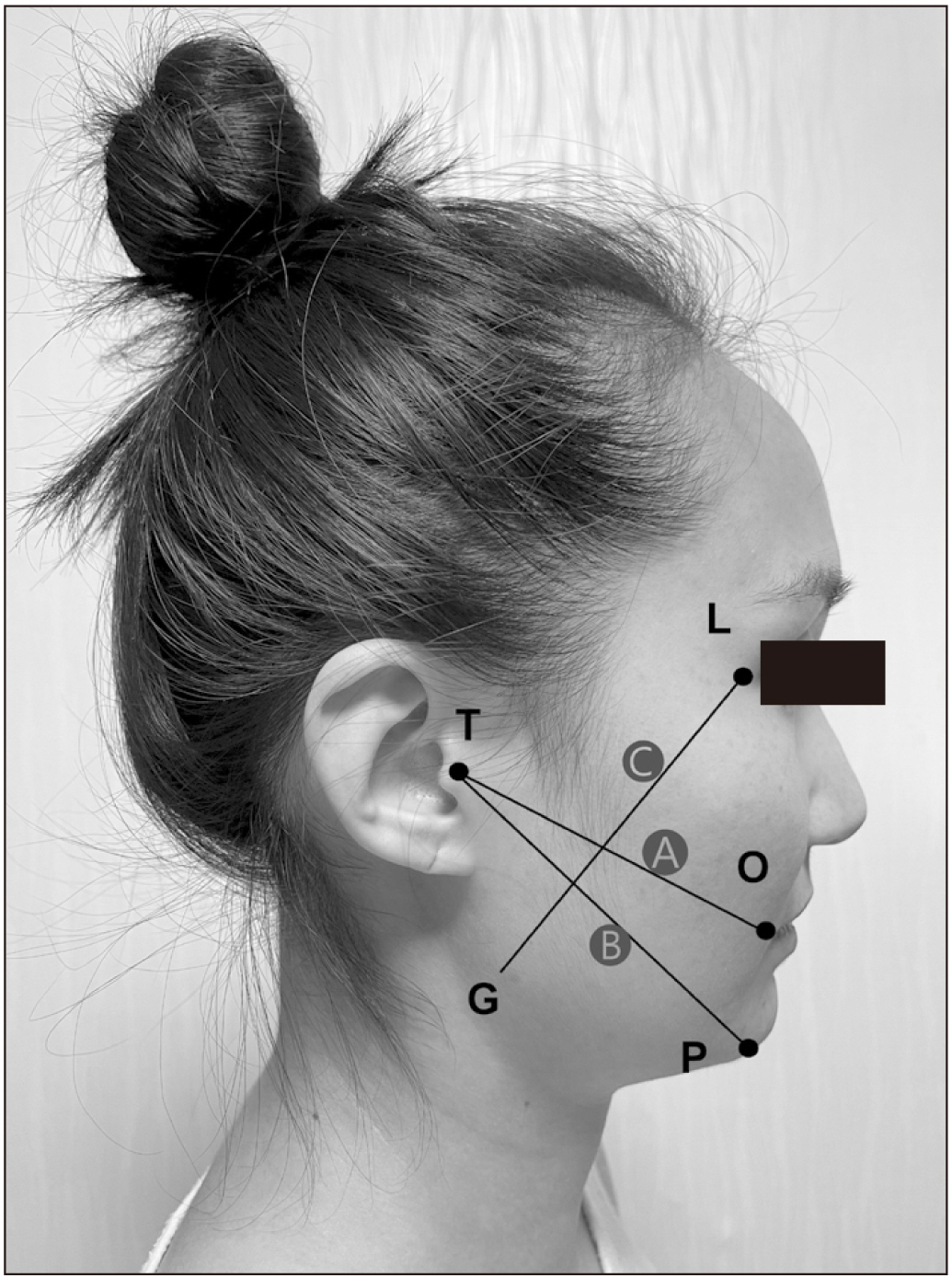
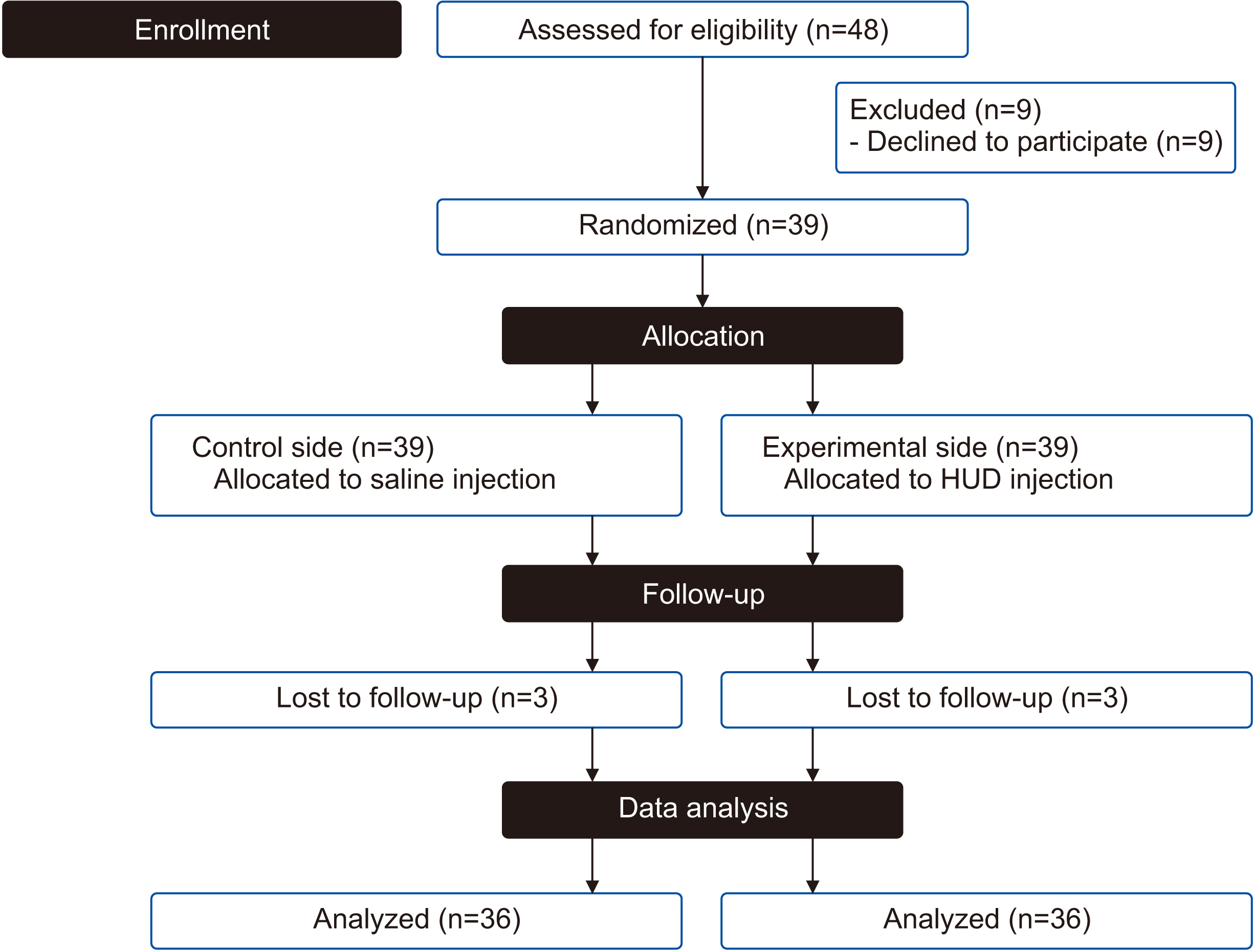
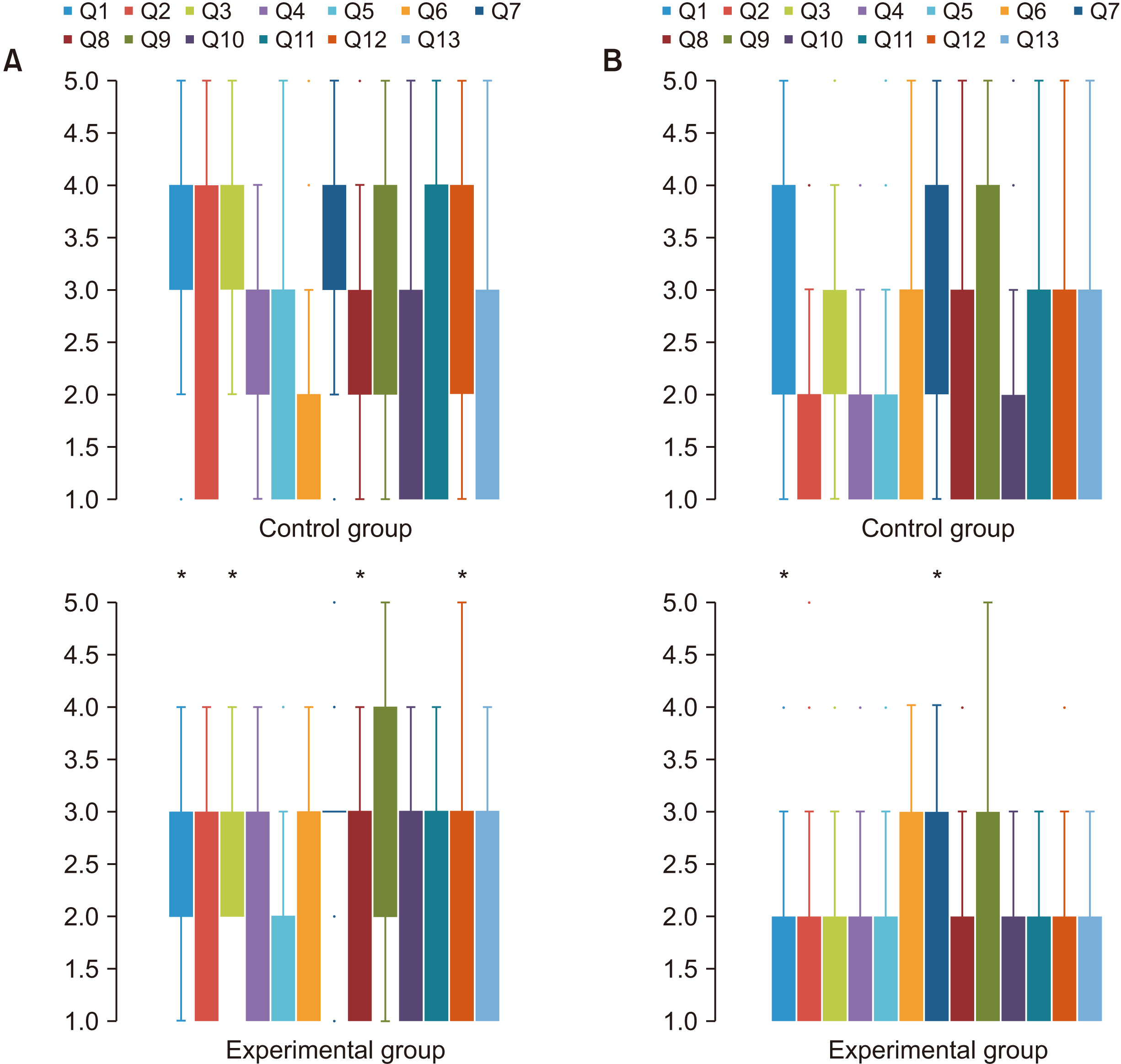
Participants with bilateral impacted M3M underwent surgical extraction with a split-mouth randomized controlled study design. M3M were removed by the same surgeon in 2 sessions, one a control and the other experimental. Submucosal injection of HUD was performed in the experimental session and submucosal injection of saline in the control session. Mouth opening, facial swelling, and pain intensity were measured before surgery, and then 2 and 7 days after surgery. The QOL of participants following surgery was evaluated by means of a patient-centered outcome questionnaire (PCOQ).
Results
A total of 36 patients was included in the final data analysis. There was a significant reduction in the maximal mouth opening and postoperative pain in the experimental side at the 2 and 7 days after surgery (P<0.05), and a remarkable difference in facial swelling was reported on the experimental side 7 days after surgery (P<0.05). The PCOQ demonstrated that participants reported less pain and swelling on the experimental side.
Conclusion
The present study provides clinical evidence that submucosal administration of HUD immediately after M3M surgery reduced postop-erative discomfort and improved patients’ QOL.
Keyword
Figure
Reference
-
References
1. Duarte-Rodrigues L, Miranda EFP, Souza TO, de Paiva HN, Falci SGM, Galvão EL. 2018; Third molar removal and its impact on quality of life: systematic review and meta-analysis. Qual Life Res. 27:2477–89. https://doi.org/10.1007/s11136-018-1889-1. DOI: 10.1007/s11136-018-1889-1. PMID: 29797177.2. Majid OW, Al-Mashhadani BA. 2014; Perioperative bromelain reduces pain and swelling and improves quality of life measures after mandibular third molar surgery: a randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg. 72:1043–8. https://doi.org/10.1016/j.joms.2013.12.035. DOI: 10.1016/j.joms.2013.12.035. PMID: 24589242.3. Al-Dajani M. 2017; Can preoperative intramuscular single-dose dexamethasone improve patient-centered outcomes following third molar surgery? J Oral Maxillofac Surg. 75:1616–26. https://doi.org/10.1016/j.joms.2017.03.037. DOI: 10.1016/j.joms.2017.03.037. PMID: 28438596.4. Xie L, Sang L, Li Z. 2021; Does low dose of etoricoxib play pre-emptive analgesic effect in third molar surgery? A randomized clinical trial. BMC Oral Health. 21:462. https://doi.org/10.1186/s12903-021-01837-0. DOI: 10.1186/s12903-021-01837-0. PMID: 34556118. PMCID: PMC8459478.5. Lim D, Ngeow WC. 2017; A comparative study on the efficacy of submucosal injection of dexamethasone versus methylprednisolone in reducing postoperative sequelae after third molar surgery. J Oral Maxillofac Surg. 75:2278–86. https://doi.org/10.1016/j.joms.2017.05.033. DOI: 10.1016/j.joms.2017.05.033. PMID: 28666096.6. Sugragan C, Sirintawat N, Kiattavornchareon S, Khoo LK, Kc K, Wongsirichat N. 2020; Do corticosteroids reduce postoperative pain following third molar intervention? J Dent Anesth Pain Med. 20:281–91. https://doi.org/10.17245/jdapm.2020.20.5.281. DOI: 10.17245/jdapm.2020.20.5.281. PMID: 33195806. PMCID: PMC7644360.7. Buhren BA, Schrumpf H, Hoff NP, Bölke E, Hilton S, Gerber PA. 2016; Hyaluronidase: from clinical applications to molecular and cellular mechanisms. Eur J Med Res. 21:5. https://doi.org/10.1186/s40001-016-0201-5. DOI: 10.1186/s40001-016-0201-5. PMID: 26873038. PMCID: PMC4752759.8. Fronza M, Muhr C, da Silveira DS, Sorgi CA, Rodrigues SF, Farsky SH, et al. 2016; Hyaluronidase decreases neutrophils infiltration to the inflammatory site. Inflamm Res. 65:533–42. https://doi.org/10.1007/s00011-016-0935-0. DOI: 10.1007/s00011-016-0935-0. PMID: 26943648.9. Satish SV, Shetty KP, Kilaru K, Bhargavi P, Reddy ES, Bellutgi A. 2013; Comparative evaluation of the efficacy of 2% lidocaine containing 1:200,000 epinephrine with and without hyaluronidase (75 IU) in patients with irreversible pulpitis. J Endod. 39:1116–8. https://doi.org/10.1016/j.joen.2012.11.049. DOI: 10.1016/j.joen.2012.11.049. PMID: 23953282.10. Fronza M, Caetano GF, Leite MN, Bitencourt CS, Paula-Silva FW, Andrade TA, et al. 2014; Hyaluronidase modulates inflammatory response and accelerates the cutaneous wound healing. PLoS One. 9:e112297. https://doi.org/10.1371/journal.pone.0112297. DOI: 10.1371/journal.pone.0112297. PMID: 25393024. PMCID: PMC4230982.11. Wu L, Liu X, Jian X, Wu X, Xu N, Dou X, et al. 2018; Delayed allergic hypersensitivity to hyaluronidase during the treatment of granulomatous hyaluronic acid reactions. J Cosmet Dermatol. 17:991–5. https://doi.org/10.1111/jocd.12461. DOI: 10.1111/jocd.12461. PMID: 29159865.12. Venkatesh KH, Rao GS. 2007; Treatment of supraglottic airway edema by local hyaluronidase. Anesthesiology. 106:1254–5. https://doi.org/10.1097/01.anes.0000265425.52996.fc. DOI: 10.1097/01.anes.0000265425.52996.fc. PMID: 17525618.13. Henkel GH. 1956; The role and applicability of hyaluronidase in clinical dentistry. Oral Surg Oral Med Oral Pathol. 9:463–92. https://doi.org/10.1016/0030-4220(56)90125-6. DOI: 10.1016/0030-4220(56)90125-6. PMID: 13309976.14. Winter GB. 1926. Principles of exodontia as applied to the impacted mandibular third molar: a complete treatise on the operative technic with clinical diagnoses and radiographic interpretations. American medical Book Company;Louis (MO): DOI: 10.1016/0030-4220(56)90125-6.15. Pell GJ, Gregory GT. 1942; Report on a ten-year study of a tooth division technique for the removal of impacted teeth. Am J Orthod Oral Surg. 28:B660–6. https://doi.org/10.1016/S0096-6347(42)90021-8. DOI: 10.1016/S0096-6347(42)90021-8.16. Pederson GW. 1988. Oral surgery. WB Saunders;Philadelphia (PA): DOI: 10.1016/s0096-6347(42)90021-8.17. Slade GD, Spencer AJ. 1994; Development and evaluation of the oral health impact profile. Community Dent Health. 11:3–11. PMID: 8193981.18. Koçer G, Yuce E, Tuzuner Oncul A, Dereci O, Koskan O. 2014; Effect of the route of administration of methylprednisolone on oedema and trismus in impacted lower third molar surgery. Int J Oral Maxillofac Surg. 43:639–43. https://doi.org/10.1016/j.ijom.2013.11.005. DOI: 10.1016/j.ijom.2013.11.005. PMID: 24332587.19. Warraich R, Faisal M, Rana M, Shaheen A, Gellrich NC, Rana M. 2013; Evaluation of postoperative discomfort following third molar surgery using submucosal dexamethasone - a randomized observer blind prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 116:16–22. https://doi.org/10.1016/j.oooo.2012.12.007. DOI: 10.1016/j.oooo.2012.12.007. PMID: 23453611.20. Bilginaylar K, Uyanik LO. 2016; Evaluation of the effects of platelet-rich fibrin and piezosurgery on outcomes after removal of ımpacted mandibular third molars. Br J Oral Maxillofac Surg. 54:629–33. https://doi.org/10.1016/j.bjoms.2016.03.016. DOI: 10.1016/j.bjoms.2016.03.016. PMID: 27044941.21. Starzyńska A, Kaczoruk-Wieremczuk M, Lopez MA, Passarelli PC, Adamska P. 2021; The growth factors in advanced platelet-rich fibrin (A-PRF) reduce postoperative complications after mandibular third molar odontectomy. Int J Environ Res Public Health. 18:13343. https://doi.org/10.3390/ijerph182413343. DOI: 10.3390/ijerph182413343. PMID: 34948953. PMCID: PMC8702191.22. Eshghpour M, Ahrari F, Takallu M. 2016; Is low-level laser therapy effective in the management of pain and swelling after mandibular third molar surgery? J Oral Maxillofac Surg. 74:1322.e1–8. https://doi.org/10.1016/j.joms.2016.02.030. DOI: 10.1016/j.joms.2016.02.030. PMID: 27055228.23. Kwoen MJ, Choi YH, Kim KS, Chang NH, Kim YK, Lee HJ. 2021; Efficacy of local hyaluronidase administration in guided bone regeneration surgery: a randomized controlled trial. J Korean Assoc Oral Maxillofac Surg. 47:91–8. https://doi.org/10.5125/jkaoms.2021.47.2.91. DOI: 10.5125/jkaoms.2021.47.2.91. PMID: 33911041. PMCID: PMC8084749.24. Kim JH, Yang H, Oh SH, Song SH, Kyung H. 2019; The efficacy of hyaluronidase in early surgery of nasal bone fracture. J Craniofac Surg. 30:e617–9. https://doi.org/10.1097/SCS.0000000000005646. DOI: 10.1097/SCS.0000000000005646. PMID: 31261329.25. Smaïl-Faugeron V, Fron-Chabouis H, Courson F, Durieux P. 2014; Comparison of intervention effects in split-mouth and parallel-arm randomized controlled trials: a meta-epidemiological study. BMC Med Res Methodol. 14:64. https://doi.org/10.1186/1471-2288-14-64. DOI: 10.1186/1471-2288-14-64. PMID: 24886043. PMCID: PMC4023173.26. Koç O, Er N. 2018; Can hyaluronidase be an alternative postoperative anti-edema agent to dexamethasone? Preliminary results of an animal study. J Oral Maxillofac Surg. 76:1653–9. https://doi.org/10.1016/j.joms.2018.03.010. DOI: 10.1016/j.joms.2018.03.010. PMID: 29654778.27. Nekoroski T, Paladini RD, Sauder DN, Frost GI, Keller GA. 2014; A recombinant human hyaluronidase sustained release gel for the treatment of post-surgical edema. Int J Dermatol. 53:777–85. https://doi.org/10.1111/ijd.12304. DOI: 10.1111/ijd.12304. PMID: 24168080.28. Han JH, Kim J, Yoon KC, Shin HW. 2018; Treatment of post-traumatic hematoma and fibrosis using hyaluronidase injection. Arch Craniofac Surg. 19:218–21. https://doi.org/10.7181/acfs.2017.01396. DOI: 10.7181/acfs.2017.01396. PMID: 30282434. PMCID: PMC6177682.29. James L, Shetty A, Rishi D, Abraham M. 2015; Management of oral submucous fibrosis with injection of hyaluronidase and dexamethasone in grade III oral submucous fibrosis: a retrospective study. J Int Oral Health. 7:82–5. PMID: 26464545. PMCID: PMC4588796.30. Delaere L, Zeyen T, Foets B, Van Calster J, Stalmans I. 2009; Allergic reaction to hyaluronidase after retrobulbar anaesthesia: a case series and review. Int Ophthalmol. 29:521–8. https://doi.org/10.1007/s10792-008-9258-7. DOI: 10.1007/s10792-008-9258-7. PMID: 18784901.31. Kim MS, Youn S, Na CH, Shin BS. 2015; Allergic reaction to hyaluronidase use after hyaluronic acid filler injection. J Cosmet Laser Ther. 17:283–5. https://doi.org/10.3109/14764172.2015.1007069. DOI: 10.3109/14764172.2015.1007069. PMID: 25588036.32. Kim TW, Lee JH, Yoon KB, Yoon DM. 2011; Allergic reactions to hyaluronidase in pain management -a report of three cases-. Korean J Anesthesiol. 60:57–9. https://doi.org/10.4097/kjae.2011.60.1.57. DOI: 10.4097/kjae.2011.60.1.57. PMID: 21359084. PMCID: PMC3040435.33. Bailey SH, Fagien S, Rohrich RJ. 2014; Changing role of hyaluronidase in plastic surgery. Plast Reconstr Surg. 133:127e–132e. https://doi.org/10.1097/PRS.0b013e3182a4c282. DOI: 10.1097/PRS.0b013e3182a4c282. PMID: 24469183.34. Zamora-Alejo K, Moore S, Leatherbarrow B, Norris JH, Lake DB, Malhotra R, Selva D, Goggin M. 2013; Hyaluronidase toxicity: a possible cause of postoperative periorbital inflammation. Clin Exp Ophthalmol. 41(2):122–6. https://doi.org/10.1111/j.1442-9071.2012.02834.x. DOI: 10.1111/j.1442-9071.2012.02834.x. PMID: 22712486.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inferior alveolar nerve block by intraosseous injection with Quicksleeper® at the retromolar area in mandibular third molar surgery
- An Evaluation of the Effectiveness of Hyaluronidase in the Selective Nerve Root Block of Radiculopathy: A Double Blind, Controlled Clinical Trial
- Hyaluronidase: An overview of its properties, applications, and side effects
- Comparison of the effects of articaine and bupivacaine in impacted mandibular third molar tooth surgery: a randomized, controlled trial
- Clinical evaluation of efficacy of transcortical anesthesia for the extraction of impacted mandibular third molars: a randomized controlled trial