J Korean Med Sci.
2022 Dec;37(48):e342. 10.3346/jkms.2022.37.e342.
COVID-19 Sequelae and Their Implications on Social Services
- Affiliations
-
- 1Korea Institute of Public Administration, Seoul, Korea
- 2Department of Gastroenterology and Hepatology, National Medical Center, Seoul, Korea
- 3Department of Social Welfare, National Medical Center, Seoul, Korea
- 4Center for Public Health, National Medical Center, Seoul, Korea
- 5Graduate School of Public Administration, Seoul National University, Seoul, Korea
- KMID: 2536733
- DOI: http://doi.org/10.3346/jkms.2022.37.e342
Abstract
- Background
The impact of persistent coronavirus disease 2019 (COVID-19) symptoms on quality of life remains unclear. This study aimed to describe such persistent symptoms and their relationships with quality of life, including clinical frailty and subjective health status.
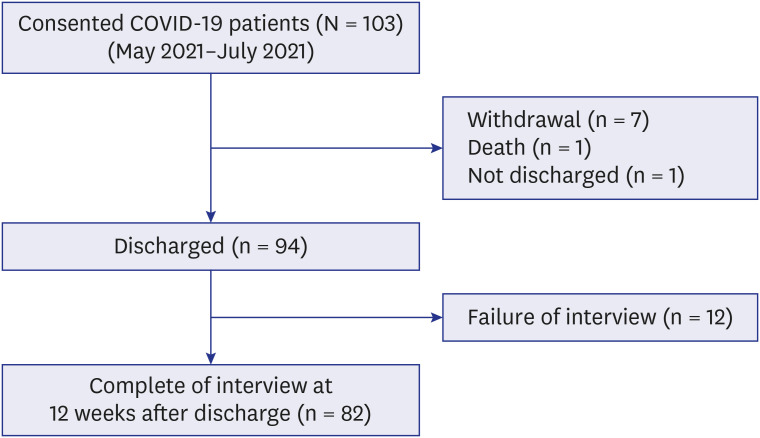
Methods
A prospective longitudinal 3-month follow-up survey monitored symptoms, health quality, support needs, frailty, and employment.
Results
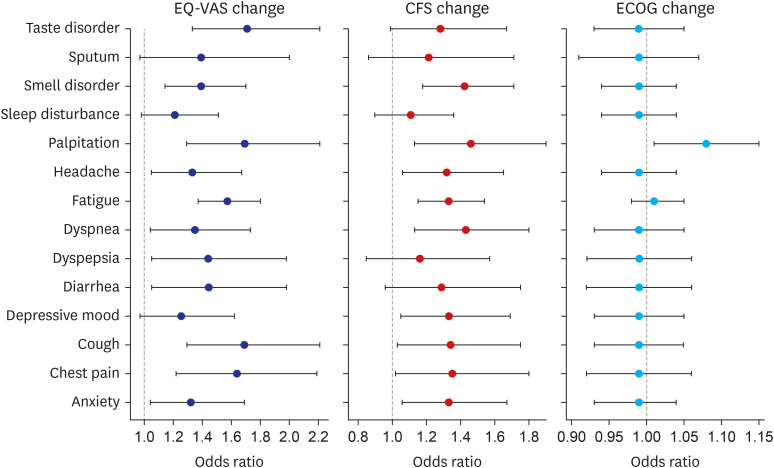
A total of 82 patients with a mean age of 52 years (ranging from 23–84 years) were enrolled, including 48 (58.6%) men, and 34 (41.5%) women. The fully active status decreased from 87.8% before admission to 78.1% post discharge. Two patients (2.4%) were ambulatory and capable of all self-care but unable to carry out any work-related activities 12 weeks after discharge. Clinical frailty scale (CFS) levels 1, 2, 3 and 4 changed drastically between admission and 12 weeks later after discharge. Just after admission, the median EuroQol visual analogue scales (EQ-VAS) was 82.23 (± 14.38), and it decreased to 78.10 (± 16.02) 12 weeks after discharge; 62 (75.6%) of patients reported at least one symptom 12 weeks after discharge. The most frequent symptom was fatigue followed by smell disorder, anxiety, sleep disorder, headache, depressive mood, dyspnea, and taste disorder. CFS was definitively associated with fatigue. Decreased EQ-VAS was associated with fatigue and palpitation, cough, taste disorder, and chest pain. EQ-VAS was worse in women (28%) than in men. Compared with regular outpatient clinic visits before admission, 21 patients (25.6%) reported increased outpatient clinic visits, one (1.4%) reported readmission, and one (1.4%) reported emergency room visits. Six of the 54 (77.1%) patients who were employed before admission lost their jobs. And most vulnerable type was self-employed, because three selfemployed job workers were not working at 12 weeks after discharge.
Conclusion
COVID-19 sequelae should not be underestimated. We find a decrease in health quality and increase in psychological problems in discharged COVID-19 patients, and some patients experience unemployment. The number of patients suffering from COVID-19 sequelae would not be negligible considering there are more than one million COVID-19 infection cases in Korea. Hence, the government should start a systematic monitoring system for discharged patients and prepare timely medical and social interventions accordingly.
Figure
Reference
-
1. Dighe A, Cattarino L, Cuomo-Dannenburg G, Skarp J, Imai N, Bhatia S, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020; 18(1):321. PMID: 33032601.2. Sachs J, Schmidt-Traub G, Kroll C, Lafortune G, Fuller G, Woelm F. Sustainable development report 2020: the sustainable development goals and COVID-19. Cambridge, MA, USA: Cambridge University Press;2020.3. Saab FG, Chiang JN, Brook R, Adamson PC, Fulcher JA, Halperin E, et al. Discharge clinical characteristics and post-discharge events in patients with severe COVID-19: a descriptive case series. J Gen Intern Med. 2021; 36(4):1017–1022. PMID: 33532963.4. Atalla E, Kalligeros M, Giampaolo G, Mylona EK, Shehadeh F, Mylonakis E. Readmissions among patients with COVID-19. Int J Clin Pract. 2021; 75(3):e13700. PMID: 32894801.5. Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol. 2021; 93(2):1013–1022. PMID: 32729939.6. Saigal A, Naidu S, Shah A, Brill S, Jarvis H, Goldring J, et al. S54|‘Long-COVID’: the need for multi-disciplinary working. Thorax. 2021; 76(Suppl 1):A33–A34.7. Somani SS, Richter F, Fuster V, De Freitas JK, Naik N, Sigel K, et al. Characterization of patients who return to hospital following discharge from hospitalization for COVID-19. J Gen Intern Med. 2020; 35(10):2838–2844. PMID: 32815060.8. Wang PR, Oyem PC, Viguera AC. Prevalence of psychiatric morbidity following discharge after COVID-19 hospitalization. Gen Hosp Psychiatry. 2021; 69:131–132. PMID: 33494979.9. Park HY, Jung J, Park HY, Lee SH, Kim ES, Kim HB, et al. Psychological consequences of survivors of COVID-19 pneumonia 1 month after discharge. J Korean Med Sci. 2020; 35(47):e409. PMID: 33289371.10. Vilches-Moraga A, Price A, Braude P, Pearce L, Short R, Verduri A, et al. Increased care at discharge from COVID-19: the association between pre-admission frailty and increased care needs after hospital discharge; a multicentre European observational cohort study. BMC Med. 2020; 18(1):408. PMID: 33334341.11. Chopra V, Flanders SA, O’Malley M, Malani AN, Prescott HC. Sixty-day outcomes among patients hospitalized with COVID-19. Ann Intern Med. 2021; 174(4):576–578. PMID: 33175566.12. Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C, et al. Health-related quality of life of COVID-19 patients after discharge: a multicenter follow-up study. J Clin Nurs. 2021; 30(11-12):1742–1750. PMID: 33656210.13. R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing;2020.14. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005; 173(5):489–495. PMID: 16129869.15. Müller I, Mancinetti M, Renner A, Bridevaux PO, Brutsche MH, Clarenbach C, et al. Frailty assessment for COVID-19 follow-up: a prospective cohort study. BMJ Open Respir Res. 2022; 9(1):e001227.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Residual Neuropsychiatric Sequelae of the Elderly and Neurocognitive Disorder Patients Who Recovered from Coronavirus Infection (COVID-19) : A review
- Chest CT Imaging Features of the Pulmonary Sequelae in Four Patients with COVID-19
- Food service industry in the era of COVID-19: trends and research implications
- Social Determinants of COVID-19 in Massachusetts, United States: An Ecological Study
- COVID-19 and Long-Term Sequelae