J Rhinol.
2022 Nov;29(3):155-162. 10.18787/jr.2022.00424.
Diagnostic Performance of Photoplethysmography-Based Smartwatch for Obstructive Sleep Apnea
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Daejeon Eulji Medical Center, Eulji University, Daejeon, Republic of Korea
- 2Department of Sleep Clinic Center, Daejeon Eulji Medical Center, Eulji University, Daejeon, Republic of Korea
- KMID: 2536584
- DOI: http://doi.org/10.18787/jr.2022.00424
Abstract
- Background and Objectives
Considering the prevalence and health effects of obstructive sleep apnea (OSA), early diagnosis and proper treatment are essential. Polysomnography (PSG) has limitations in diagnosing or tracking large-scale OSA patients. Smartwatches (SWs) can be equipped with a photoplethysmograph (PPG) that can indirectly measure heart rate and blood oxygen saturation by detecting the difference of light absorption through blood. The purpose of this study is to compare oxygen saturation parameters of PPG-based SWs with those of PSG to determine the diagnostic accuracy for OSA.
Methods
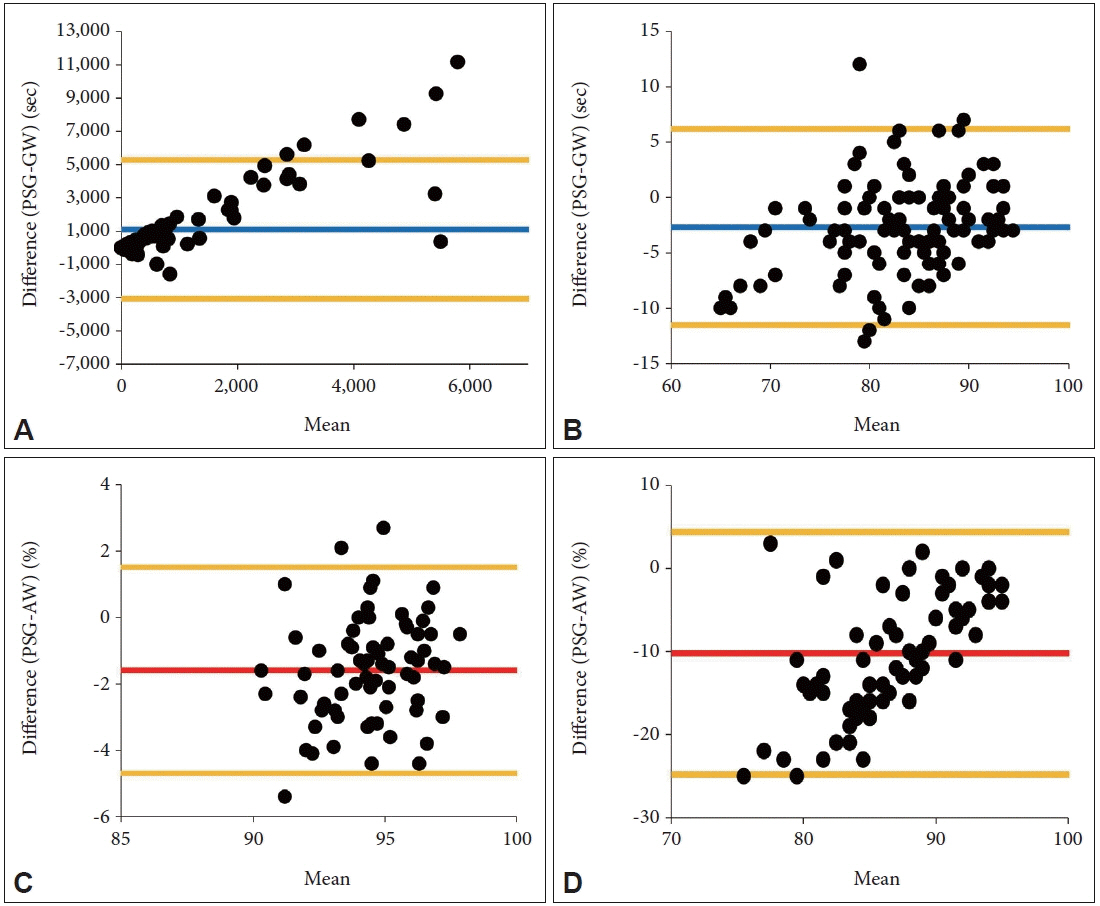
After obtaining voluntary consent from patients who were scheduled to undergo PSG in a sleep clinic due to suspected OSA, they were randomly assigned to wear a Galaxy watch4 (GW) or Apple watch7 (AW) on their wrist. The agreement rates between the oxygen saturation parameters of the two SW types and PSG were evaluated. The accuracy, sensitivity, and specificity of the oxygen saturation parameters for diagnosis of OSA (apnea-hypopnea index [AHI] ≥5/h) were compared between the two types of SW.
Results
A total of 133 patients underwent PSG while wearing an SW. Including duplicates, 109 patients wearing a GW and 69 wearing an AW were included. The diagnostic accuracy of AHI ≥5/h according to oxygen saturation time measured by a GW was less than 90%, the respective sensitivity and specificity were 82.9% and 75.8%. The area under the curve (AUC) of the receiver operating characteristic (ROC) curve was 0.807 (p<0.001). Using the lowest oxygen saturation value of GW, the sensitivity was 81.6%, the specificity was 69.7%, and the AUC of the ROC was 0.849 (p<0.001). The diagnostic accuracy of AHI ≥5/h according to the average oxygen saturation of AW, and the sensitivity and specificity were 75.6% and 70.8%, respectively. The AUC of this ROC curve was 0.757 (p<0.001). Using the lowest oxygen saturation value of AW, the sensitivity was 71.1%, the specificity was 62.5%, and the AUC of the ROC was 0.705 (p=0.005).
Conclusion
This study found that the two types of SW showed considerable accuracy in diagnosing OSA, but the accuracy decreased as the severity of OSA increased.
Keyword
Figure
Cited by 1 articles
-
STOP-Bang and Smartwatch’s Two-Step Approach for Obstructive Sleep Apnea Screening
Min Woo Kim, Myoung Su Choi
Korean J Otorhinolaryngol-Head Neck Surg. 2023;66(7):455-461. doi: 10.3342/kjorl-hns.2023.00402.
Reference
-
References
1. Lee YJ. Updates of diagnosis and treatment of sleep-related breathing disorders-focusing on obstructive sleep apnea. J Korean Neuropsychiatr Assoc. 2020; 59(1):20–4.
Article2. Kim J, In K, Kim J, You S, Kang K, Shim J, et al. Prevalence of sleepdisordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med. 2004; 170(10):1108–13.3. Gilman MP, Floras JS, Usui K, Kaneko Y, Leung RS, Bradley TD. Continuous positive airway pressure increases heart rate variability in heart failure patients with obstructive sleep apnoea. Clin Sci (Lond). 2008; 114(3):243–9.
Article4. Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Nieto FJ, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the sleep heart health study. Am J Respir Crit Care Med. 2001; 163(1):19–25.
Article5. Harding SM. Complications and consequences of obstructive sleep apnea. Curr Opin Pulm Med. 2000; 6(6):485–9.
Article6. Caples SM, Anderson WM, Calero K, Howell M, Hashmi SD. Use of polysomnography and home sleep apnea tests for the longitudinal management of obstructive sleep apnea in adults: an American Academy of Sleep Medicine clinical guidance statement. J Clin Sleep Med. 2021; 17(6):1287–93.
Article7. Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of M-health technologies for improving health and health services: a systematic review protocol. BMC Res Notes. 2010; 3:250.
Article8. Kim K, Park DY, Song YJ, Han S, Kim HJ. Consumer-grade sleep trackers are still not up to par compared to polysomnography. Sleep Breath. 2022; 26(4):1573–82.
Article9. Stone JD, Rentz LE, Forsey J, Ramadan J, Markwald RR, Finomore VS, et al. Evaluations of commercial sleep technologies for objective monitoring during routine sleeping conditions. Nat Sci Sleep. 2020; 12:821–42.10. Moreno-Pino F, Porras-Segovia A, López-Esteban P, Artés A, Baca-García E. Validation of Fitbit Charge 2 and Fitbit Alta HR against polysomnography for assessing sleep in adults with obstructive sleep apnea. J Clin Sleep Med. 2019; 15(11):1645–53.
Article11. Wali SO, Abaalkhail B, AlQassas I, Alhejaili F, Spence DW, Pandi-Perumal SR. The correlation between oxygen saturation indices and the standard obstructive sleep apnea severity. Ann Thorac Med. 2020; 15(2):70–5.
Article12. Kainulainen S, Töyräs J, Oksenberg A, Korkalainen H, Sefa S, Kulkas A, et al. Severity of desaturations reflects OSA-related daytime sleepiness better than AHI. J Clin Sleep Med. 2019; 15(8):1135–42.
Article13. Rashid NH, Zaghi S, Scapuccin M, Camacho M, Certal V, Capasso R. The value of oxygen desaturation index for diagnosing obstructive sleep apnea: a systematic review. Laryngoscope. 2021; 131(2):440–7.
Article14. Zijlstra WG, Buursma A, Meeuwsen-van der Roest WP. Absorption spectra of human fetal and adult oxyhemoglobin, de-oxyhemoglobin, carboxyhemoglobin, and methemoglobin. Clin Chem. 1991; 37(9):1633–8.
Article15. Jung H, Kim D, Lee W, Seo H, Seo J, Choi J, et al. Performance evaluation of a wrist-worn reflectance pulse oximeter during sleep. Sleep Health. 2022; 8(5):420–8.
Article16. Chen Y, Wang W, Guo Y, Zhang H, Chen Y, Xie L. A single-center validation of the accuracy of a photoplethysmography-based smartwatch for screening obstructive sleep apnea. Nat Sci Sleep. 2021; 13:1533–44.
Article17. Papini GB, Fonseca P, van Gilst MM, Bergmans JWM, Vullings R, Overeem S. Wearable monitoring of sleep-disordered breathing: estimation of the apnea-hypopnea index using wrist-worn reflective photoplethysmography. Sci Rep. 2020; 10(1):13512.
Article18. Dawson A, Loving RT, Gordon RM, Abel SL, Loewy D, Kripke DF, et al. Type III home sleep testing versus pulse oximetry: is the respiratory disturbance index better than the oxygen desaturation index to predict the apnoea-hypopnoea index measured during laboratory polysomnography? BMJ Open. 2015; 5(6):e007956.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- STOP-Bang and Smartwatch’s Two-Step Approach for Obstructive Sleep Apnea Screening
- Pathophysiology and Diagnosis of Sleep Apnea
- Pediatric sleep questionnaires for screening of obstructive sleep apnea syndrome
- A Case of Huge Lingual Tonsillar Hypertrophy Causing Obstructive Sleep Apnea in Adult
- Pathogenesis of Obstructive Sleep Apnea