J Korean Med Sci.
2022 Dec;37(47):e337. 10.3346/jkms.2022.37.e337.
Comparison of the Clinical Characteristics of Pediatric Poisoning Patients Who Visited Emergency Department Before and During the COVID-19 Pandemic
- Affiliations
-
- 1Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Korea
- 2Department of Emergency Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea
- KMID: 2536516
- DOI: http://doi.org/10.3346/jkms.2022.37.e337
Abstract
- Background
We aimed to investigate changes in the clinical characteristics of pediatric poisoning patients who visited the emergency department (ED) before and during the coronavirus disease 2019 (COVID-19) pandemic.
Methods
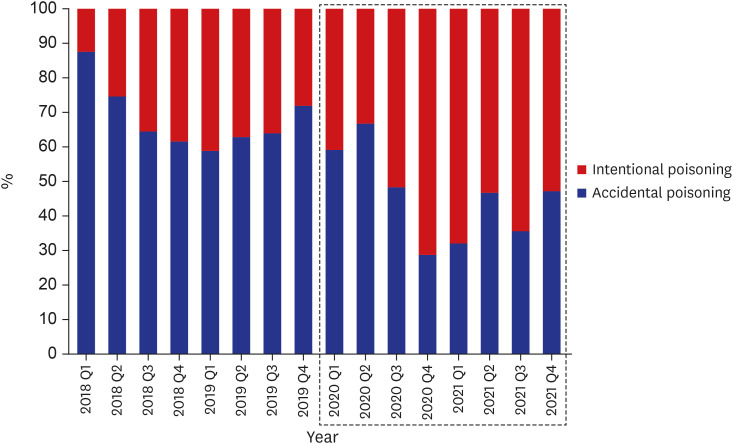
Poisoning cases below age 18 who visited the ED from January 2018 to December 2021 were retrospectively analysed. The study period was then divided into pre-COVID-19 and COVID-19 pandemic to compare poisoning patterns.
Results
During the study period, 86,153 visits to the pediatric ED had been recorded, with 625 patients being included the final analysis. During the COVID-19 period, the proportion of poisoned patients increased from 0.62% to 0.98%. The average age of the patients was higher in the COVID-19 period, with 53.4% of the cases being intentional (pre-COVID-19, 32.5%; P < 0.001). Moreover, 70.4% of poisoning cases during the COVID-19 period were caused by drugs (pre-COVID-19, 60.6%; P = 0.038). More patients underwent decontamination and laboratory investigation during the COVID-19 period than during the previous period (P= 0.007 and P < 0.001, respectively). The length of ED stay and the proportion of hospitalisation were significantly greater during the COVID-19 period. After analysing accidental poisoning cases, we found that antipyretics/nonsteroidal anti-inflammatory drugs and respiratory drugs were more common in the pre-COVID-19 group, whereas iron/vitamins, cardiovascular drugs and hormones were more common in the COVID-19 group. After analysing intentional poisoning cases, we found that 73.6% and 76.4% of the patients in the pre-COVID-19 and COVID-19 group had a history of psychiatric disease, respectively. Although no difference was observed in the frequency of previous first suicide attempts, 19.0% of the patients in the COVID-19 group attempted suicide more than three times.
Conclusion
During the COVID-19 pandemic, intentional poisoning cases, especially in adolescence, increased and were treated more. Many of the patients with intentional poisoning had a history of mental illness or suicide in the past. Therefore, it seems that policy consideration for mentally vulnerable adolescents during this new pandemic period is necessary.
Figure
Reference
-
1. Han CS, Jeon WC, Min YG, Choi SC, Lee JS. Retrospective analysis on the clinical differences of children and adolescents treated for acute pediatric poisoning in an emergency department. J Korean Soc Emerg Med. 2013; 24(6):742–749.2. Lam LT. Childhood and adolescence poisoning in NSW, Australia: an analysis of age, sex, geographic, and poison types. Inj Prev. 2003; 9(4):338–342. PMID: 14693896.3. Hon KL, Ho JK, Leung TF, Wong Y, Nelson EA, Fok TF. Review of children hospitalised for ingestion and poisoning at a tertiary centre. Ann Acad Med Singapore. 2005; 34(5):356–361. PMID: 16021225.4. Suh J, Eo E. The differences of clinical aspects in children and adolescents poisoning. J Korean Soc Clin Toxicol. 2006; 4(1):17–24.5. Cunningham RM, Walton MA, Carter PM. The major causes of death in children and adolescents in the United States. N Engl J Med. 2018; 379(25):2468–2475. PMID: 30575483.6. Mintegi S, Fernández A, Alustiza J, Canduela V, Mongil I, Caubet I, et al. Emergency visits for childhood poisoning: a 2-year prospective multicenter survey in Spain. Pediatr Emerg Care. 2006; 22(5):334–338. PMID: 16714960.7. Kim DY, Kim JH, Paik JH, Han SB, Jung HM. Analysis of characteristics in children and adolescents with poisoning at emergency department. J Korean Soc Clin Toxicol. 2017; 15(2):140–147.8. Ryu WS, Choi JY, Cho JS, Lim YS, Hyun SY, Yang HJ. Age group characteristics of children who visited the emergency department with acute poisoning by ingestion. Pediatr Emerg Med J. 2018; 5(1):5–12.9. Andiran N, Sarikayalar F. Pattern of acute poisonings in childhood in Ankara: what has changed in twenty years? Turk J Pediatr. 2004; 46(2):147–152. PMID: 15214744.10. Sahin S, Carman KB, Dinleyici EC. Acute poisoning in children; data of a pediatric emergency unit. Iran J Pediatr. 2011; 21(4):479–484. PMID: 23056835.11. Gul MK, Demirci E. Psychiatric disorders and symptoms in children and adolescents during the COVID-19 pandemic; a review. Eurasian J Med Oncol. 2021; 5(1):20–36.12. Deolmi M, Pisani F. Psychological and psychiatric impact of COVID-19 pandemic among children and adolescents. Acta Biomed. 2020; 91(4):e2020149. PMID: 33525229.13. Ye J. Pediatric mental and behavioral health in the period of quarantine and social distancing with COVID-19. JMIR Pediatr Parent. 2020; 3(2):e19867. PMID: 32634105.14. Yard E, Radhakrishnan L, Ballesteros MF, Sheppard M, Gates A, Stein Z, et al. Emergency department visits for suspected suicide attempts among persons aged 12-25 years before and during the COVID-19 pandemic - United States, January 2019-May 2021. MMWR Morb Mortal Wkly Rep. 2021; 70(24):888–894. PMID: 34138833.15. Liguoro I, Pilotto C, Vergine M, Pusiol A, Vidal E, Cogo P. The impact of COVID-19 on a tertiary care pediatric emergency department. Eur J Pediatr. 2021; 180(5):1497–1504. PMID: 33409588.16. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020; 291:113264. PMID: 32622172.17. Jefsen OH, Rohde C, Nørremark B, Østergaard SD. Editorial pserspective: COVID-19 pandemic-related psychopathology in children and adolescents with mental illness. J Child Psychol Psychiatry. 2021; 62(6):798–800. PMID: 32779748.18. Longobardi C, Morese R, Fabris MA. COVID-19 emergency: social distancing and social exclusion as risks for suicide ideation and attempts in adolescents. Front Psychol. 2020; 11:551113. PMID: 33329182.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in the characteristics of acute carbon monoxide poisoning patients who visited the emergency department during the COVID-19 pandemic
- Characteristics of poisoning patients visiting emergency departments before and after the COVID-19 pandemic
- Characteristics and clinical outcomes of older patients with trauma visiting the emergency department before and during the COVID-19 Pandemic: A level 1 trauma center cohort study
- Impact of coronavirus disease 2019 pandemic on pediatric poisoning in a single emergency department in Korea
- Comparison of Monthly Characteristics of Adolescent Suicide Attempts Before, During and After COVID-19