Clin Endosc.
2022 Nov;55(6):767-774. 10.5946/ce.2022.002.
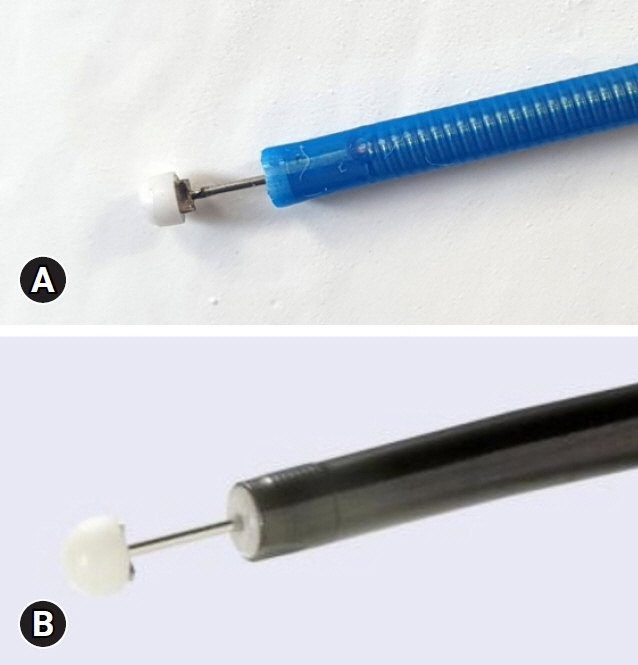
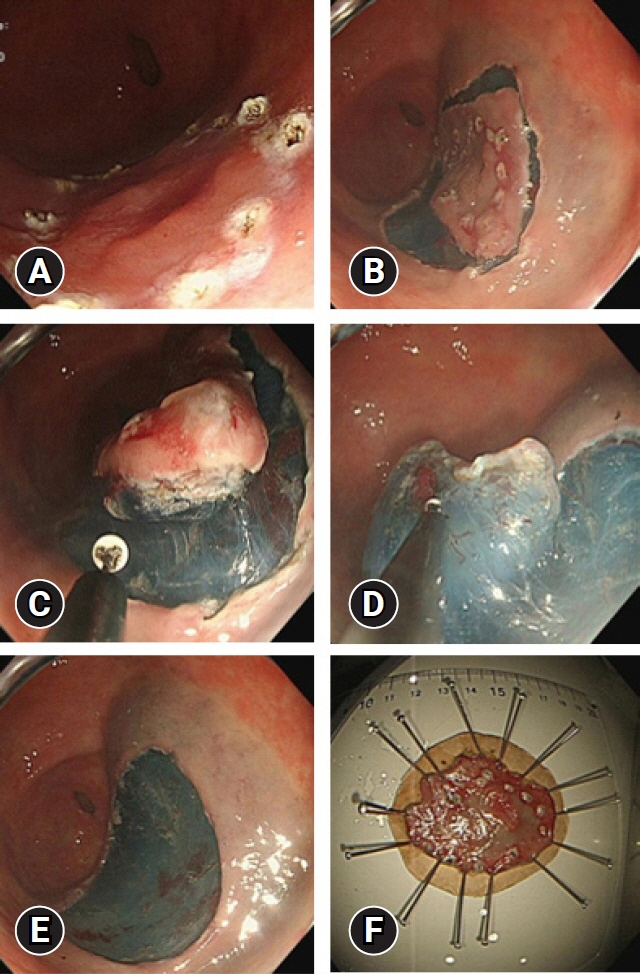
Comparison between a novel core knife and the conventional IT knife 2 for endoscopic submucosal dissection of gastric mucosal lesions
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2536077
- DOI: http://doi.org/10.5946/ce.2022.002
Abstract
- Background/Aims
Few studies have compared the performances of endoscopic knives. This study aimed to compare the therapeutic outcomes of a novel core knife and the conventional IT knife 2 for endoscopic submucosal dissection (ESD) of gastric mucosal lesions.
Methods
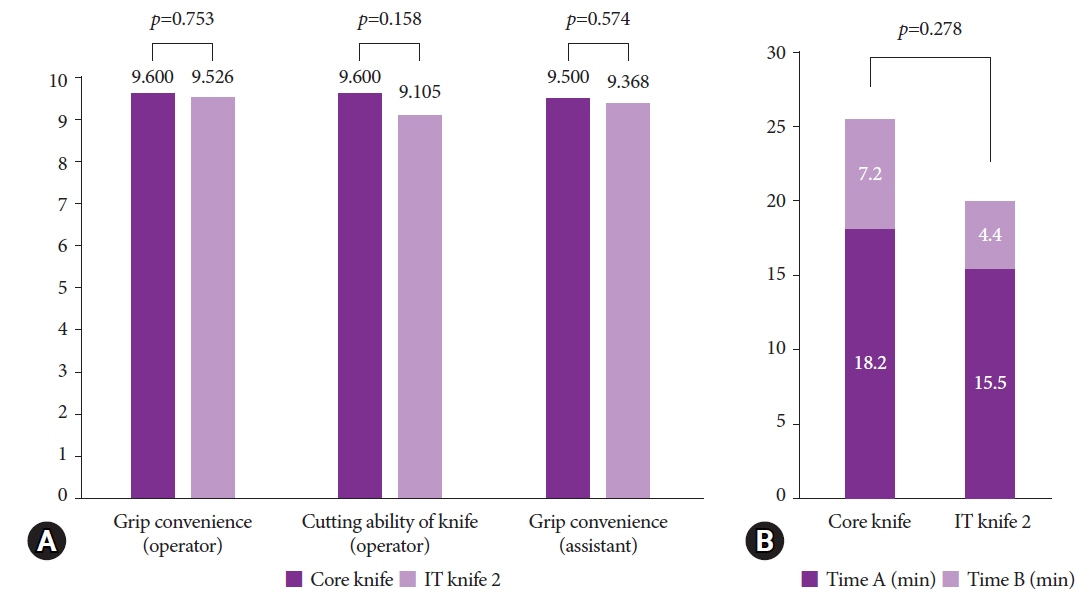
This prospective, non-inferiority trial included patients diagnosed with gastric adenoma or early-stage adenocarcinoma at Keimyung University Dongsan Hospital between June and November 2020. The patients were randomly assigned to either the core knife or the IT knife 2 group. The operators and assistants scored the knives’ grip convenience and cutting abilities.
Results
A total of 39 patients were enrolled (core knife group, 20 patients; IT knife 2 group, 19 patients). There were no significant between-group differences in operator-assessed grip convenience (9.600 vs. 9.526, p=0.753), cutting ability (9.600 vs. 9.105, p=0.158), or assistant-assessed grip convenience (9.500 vs. 9.368, p=0.574).
Conclusions
The core knife achieved therapeutic outcomes that were comparable to those of the IT knife 2 for ESD of gastric mucosal lesions.
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. Korean Statistical Information Service. Causes of Death Statistics in Korea 2019 [Internet]. Daejeon: Korean Statistical Information Service;2020. [cited 2020 Sep 21]. Available from: http://kostat.go.kr/portal/korea/kor_nw/1/1/index.board?bmode=download&bSeq=&aSeq=385219&ord=2.3. Park CH, Yang DH, Kim JW, et al. Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin Endosc. 2020; 53:142–166.
Article4. Ko BM. History and development of accessories for endoscopic submucosal dissection. Clin Endosc. 2017; 50:219–223.
Article5. Song JH, Kim SG. Endoscopic submucosal dissection for gastric neoplasia. In : Chun HJ, Yang SK, Choi MG, editors. Therapeutic gastrointestinal endoscopy: a comprehensive atlas. Singapore: Springer;2019. p. 125–141.6. Sumiyama K, Tajiri H. History of ESD. In : Fukami N, editor. Endoscopic submucosal dissection: principles and practice. New York: Springer;2015. p. 3–8.7. Gotoda T, Iwasaki M, Kusano C, et al. Endoscopic resection of early gastric cancer treated by guideline and expanded National Cancer Centre criteria. Br J Surg. 2010; 97:868–871.
Article8. Kamiya S, Rouvelas I, Lindblad M, et al. Current trends in gastric cancer treatment in Europe. J Cancer Metastasis Treat. 2018; 4:35.
Article9. Draganov PV, Wang AY, Othman MO, et al. AGA Institute Clinical Practice Update: endoscopic submucosal dissection in the United States. Clin Gastroenterol Hepatol. 2019; 17:16–25.
Article10. Fukami N. Endoscopic submucosal dissection: principles and practice. New York: Springer;2015.11. Oda I, Suzuki H, Nonaka S, et al. Complications of gastric endoscopic submucosal dissection. Dig Endosc. 2013; 25(Suppl 1):71–78.
Article12. Choi HS, Chun HJ. Accessory devices frequently used for endoscopic submucosal dissection. Clin Endosc. 2017; 50:224–233.
Article13. Fukami N. Appendix: commonly used ESD knives. In : Fukami N, editor. Endoscopic submucosal dissection: principles and practice. New York: Springer;2015. p. 257–260.14. Hosokawa K, Yoshida S. Recent advances in endoscopic mucosal resection for early gastric cancer. Gan To Kagaku Ryoho. 1998; 25:476–483.15. Cho JY, Cho WY. The current status of endoscopic submucosal dissection. Korean J Gastrointest Endosc. 2008; 37:317–320.16. Konuma H, Matsumoto K, Ueyama H, et al. Procedure time for gastric endoscopic submucosal dissection according to location, considering both mucosal circumferential incision and submucosal dissection. Gastroenterol Res Pract. 2016; 2016:9183793.
Article17. Kim KO, Kim SJ, Kim TH, et al. Do you have what it takes for challenging endoscopic submucosal dissection cases? World J Gastroenterol. 2011; 17:3580–3584.
Article18. Lee SG, Cho KB, Hong YS, et al. Nonsurgical treatment of gastric perforation complicated by endoscopic mucosal resection and endoscopic submucosal dissection. Korean J Gastrointest Endosc. 2008; 37:97–104.19. Park YS, Park SW, Song SY, et al. Endoscopic mucosal resection using insulated-tip electrosurgical knife. Korean J Gastrointest Endosc. 2003; 26:397–404.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy and Safety of ClearCut™ Knife H-type in Endoscopic Submucosal Dissection for Gastric Neoplasms: A Multicenter, Randomized Trial
- Endoscopic Submucosal Dissection for Gastric Tumors: Complete Resection Rate, Resection Time and Complications in Comparison with Endoscopic Mucosal Resection after Circumferential Mucosal Incision with a Needle Knife
- Treatment of Early Gastric Cancer: Endoscopic Submucosal Dissection with LASER
- Tips and Tricks for Better Endoscopic Treatment of Colorectal Tumors: Usefulness of Cap and Band in Colorectal Endoscopic Mucosal Resection
- Comparison of scissor-type knife to non-scissor-type knife for endoscopic submucosal dissection: a systematic review and meta-analysis