Korean J Schizophr Res.
2022 Oct;25(2):62-68. 10.16946/kjsr.2022.25.2.62.
Probability of Transition to Psychosis and Bipolar Disorder in Individuals With Neurodevelopmental Disorders
- Affiliations
-
- 1Department of Psychiatry, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2RaRa Psychiatric Clinic, Busan, Korea
- KMID: 2535946
- DOI: http://doi.org/10.16946/kjsr.2022.25.2.62
Abstract
Objectives
The clinical trajectories of adolescent-onset psychosis and bipolar disorder are worse than that of adult-onset cases. Although psychosis and bipolar disorder are more prevalent among those with neurodevelopmental disorders such as ADHD and autism spectrum disorder compared with the general population, the incidence during adolescence has not yet been explored.
Methods
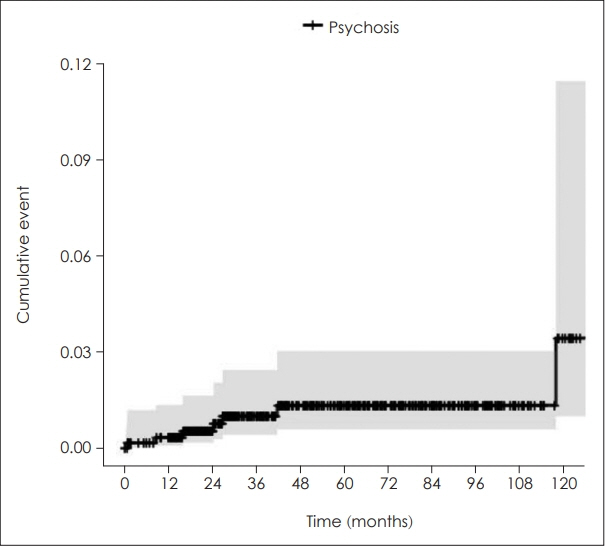
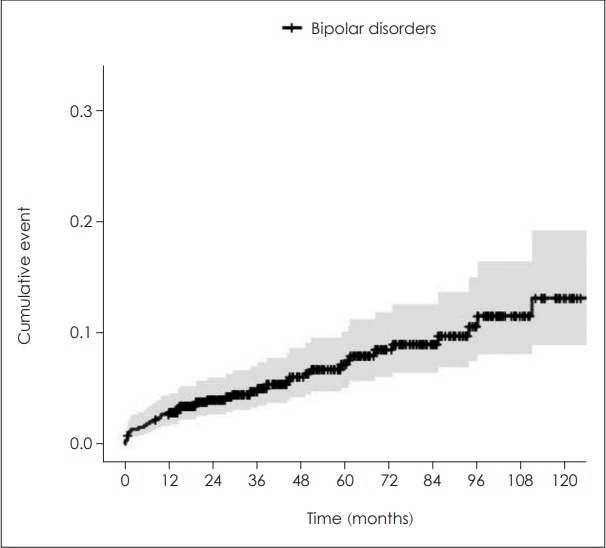
Out of 3,730 patients who visited the Department of Pediatric Psychiatry at Pusan National University Yangsan Hospital between November 2008 and May 2021, patients with neurodevelopmental disorders who did not meet the criteria for psychosis or bipolar disorder and had at least one year of the follow-up period were selected. A Kaplan-Meier analysis was performed to examine the cumulative incidence of psychosis and bipolar disorder in patients with neurodevelopmental disorders.
Results
The sample included 591 patients with neurodevelopmental disorders (mean age 12.6 years, range 10-18 years). The 9-years cumulative incidences of psychosis and bipolar disorder are 1.3% (95% CI=0.2%-2.4%), 11.6% (95% CI=7.4%-15.6%), respectively.
Conclusion
Patients with neurodevelopmental disorders showed a high incidence of psychosis and bipolar disorder during adolescence. This suggests that patients diagnosed with neurodevelopmental disorders should be continuously evaluated and monitored of the occurrence of comorbidities during adolescence.
Keyword
Figure
Reference
-
1. Valli I, Fabbri C, Young AH. Uncovering neurodevelopmental features in bipolar affective disorder. Br J Psychiatry. 2019; 215:383–385.2. Morris-Rosendahl DJ, Crocq MA. Neurodevelopmental disorders the history and future of a diagnostic concept. Dialogues Clin Neurosci. 2020; 22:65–72.3. Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10-year follow-up study. Psychol Med. 2006; 36:167–179.4. Buck TR, Viskochil J, Farley M, Coon H, McMahon WM, Morgan J, et al. Psychiatric comorbidity and medication use in adults with autism spectrum disorder. J Autism Dev Disord. 2014; 44:3063–3071.5. Lawrie SM, Whalley H, Kestelman JN, Abukmeil SS, Byrne M, Hodges A, et al. Magnetic resonance imaging of brain in people at high risk of developing schizophrenia. The Lancet. 1999; 353:30–33.6. Vita A, Dieci M, Giobbio GM, Tenconi F, Invernizzi G. Time course of cerebral ventricular enlargement in schizophrenia supports the hypothesis of its neurodevelopmental nature. Schizophr Res. 1997; 23:25–30.7. Kieseppä T, Erp TGMV, Haukka J, Partonen T, Cannon TD, Poutanen V-P, et al. The volumetric findings in MRI brain study of bipolar twins and their healthy co-twins. Bipolar Disord. 2002.8. Noga JT, Vladar K, Torrey EF. A volumetric magnetic resonance imaging study of monozygotic twins discordant for bipolar disorder. Psychiatry Res. 2001.9. Coulon N, Godin O, Bulzacka E, Dubertret C, Mallet J, Fond G, et al. Early and very early-onset schizophrenia compared with adult-onset schizophrenia: French FACE-SZ database. Brain Behav. 2020; 10:e01495.10. Clemmensen L, Vernal DL, Steinhausen HC. A systematic review of the long-term outcome of early onset schizophrenia. BMC Psychiatry. 2012.11. Cirone C, Secci I, Favole I, Ricci F, Amianto F, Davico C, et al. What Do We Know about the Long-Term Course of Early Onset Bipolar Disorder? A Review of the Current Evidence. Brain Sci. 2021; 11:341.12. Cannon M, Jones P, Huttunen MO, Tanskanen A, Huttunen T, RabeHesketh S, et al. School performance in finnish children and later development of schizophrenia: a population-based longitudinal study. Arch Gen Psychiatry. 1999.13. Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD). Biol Psychiatry. 2004; 55:875–881.14. Nourredine M, Gering A, Fourneret P, Rolland B, Falissard B, Cucherat M, et al. Association of Attention-Deficit/Hyperactivity Disorder in Childhood and Adolescence With the Risk of Subsequent Psychotic Disorder: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2021; 78:519–529.15. Varcin KJ, Herniman SE, Lin A, Chen Y, Perry Y, Pugh C, et al. Occurrence of psychosis and bipolar disorder in adults with autism: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2022; 134:104543.16. Lowe TL, Capriotti MR, McBurnett K. Long-Term Follow-up of Patients with Tourette’s Syndrome. Mov Disord Clin Pract. 2019; 6:40–45.17. Raskind MH, Goldberg RJ, Higgins EL, Herman KL. Patterns of Change and Predictors of Success in Individuals With Learning Disabilities: Results From a Twenty-Year Longitudinal Study. Learning Disabilities Research & Practice. 1999; 14:35–49.18. Mouridsen SE, Hauschild KM. A longitudinal study of schizophrenia- and affective spectrum disorders in individuals diagnosed with a developmental language disorder as children. J Neural Transm (Vienna). 2008; 115:1591–1597.19. Statistics Korea. Korean Standard Classification of Diseases. 8th ed. Daejeon: Statistics Korea;2020, p.297-352.20. Schalbroeck R, Termorshuizen F, Visser E, van Amelsvoort T, Selten JP. Risk of non-affective psychotic disorder or bipolar disorder in autism spectrum disorder: a longitudinal register-based study in the Netherlands. Psychol Med. 2019; 49:2543–2550.21. Brancati GE, Perugi G, Milone A, Masi G, Sesso G. Development of bipolar disorder in patients with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis of prospective studies. J Affect Disord. 2021; 293:186–196.22. Rosenberg RE, Kaufmann WE, Law JK, Law PA. Parent report of community psychiatric comorbid diagnoses in autism spectrum disorders. Autism Res Treat. 2011; 2011:405849.23. Van Meter A, Moreira ALR, Youngstrom E. Updated Meta-Analysis of Epidemiologic Studies of Pediatric Bipolar Disorder. J Clin Psychiatry. 2019; 80:3.24. Connor DF, Ford JD, Pearson GS, Scranton VL, Dusad A. Early-Onset Bipolar Disorder: Characteristics and Outcomes in the Clinic. J Child Adolesc Psychopharmacol. 2017; 27:875–883.25. Burd L, Kerbeshian J. A North Dakota Prevalence Study of Schizophrenia Presenting in Childhood. J Am Acad Child Adolesc Psychiatry. 1987.26. Driver DI, Gogtay N, Rapoport JL. Childhood onset schizophrenia and early onset schizophrenia spectrum disorders. Child Adolesc Psychiatr Clin N Am. 2013; 22:539–555.27. Remschmidt H, Theisen F. Early-onset schizophrenia. Neuropsychobiology. 2012; 66:63–69.28. Fusar-Poli P, Cappucciati M, Rutigliano G, Heslin M, Stahl D, Brittenden Z, et al. Diagnostic Stability of ICD/DSM First Episode Psychosis Diagnoses: Meta-analysis. Schizophr Bull. 2016; 42:1395–1406.29. Liu H, Tang Y, Womer F, Fan G, Lu T, Driesen N, et al. Differentiating patterns of amygdala-frontal functional connectivity in schizophrenia and bipolar disorder. Schizophrenia bulletin. 2014; 40:469–477.30. Correll CU, Penzner JB, Frederickson AM, Richter JJ, Auther AM, Smith CW, et al. Differentiation in the preonset phases of schizophrenia and mood disorders: evidence in support of a bipolar mania prodrome. Schizophrenia Bulletin. 2007; 33:703–714.31. Murray RM, Sham P, Van Os J, Zanelli J, Cannon M, McDonald C. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophrenia research. 2004; 71:405–416.32. Correll CU, Hauser M, Penzner JB, Auther AM, Kafantaris V, Saito E, et al. Type and duration of subsyndromal symptoms in youth with bipolar I disorder prior to their first manic episode. Bipolar Disord. 2014; 16:478–492.33. Magee C, Guhn M, Puyat JH, Gadermann A, Oberle E. Diagnosed Incidence of Non-Affective Psychotic Disorders Amongst Adolescents in British Columbia and Sociodemographic Risk Factors: A Retrospective Cohort Study. Can J Psychiatry. 2022; 67:295–304.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Probability of Transition to Psychosis and Bipolar Disorder in Individuals With Neurodevelopmental Disorders
- Psychological Assessment in Neurodevelopmental Disorders
- Comorbid Anxiety in Bipolar Disorder
- Influence of Attachment Behavior in Psychosis
- The Neurobiology of Bipolar Disorder: An Integrated Approach