Brain Tumor Res Treat.
2022 Oct;10(4):237-243. 10.14791/btrt.2022.0022.
Lumboperitoneal Shunt Combined With Ommaya Reservoir Enables Continued Intraventricular Chemotherapy for Leptomeningeal Metastasis With Increased Intracranial Pressure
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Cancer Control, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 3Neuro-Oncology Clinic, National Cancer Center, Goyang, Korea
- KMID: 2534722
- DOI: http://doi.org/10.14791/btrt.2022.0022
Abstract
- Background
Intra-cerebrospinal fluid (CSF) chemotherapy for leptomeningeal metastasis (LM) can be delivered intraventricularly via an Ommaya reservoir. However, hydrocephalus associated with LM can interfere with chemotherapeutic drug distribution, and ventriculoperitoneal shunts can prevent drug distribution to the extra-ventricular CSF space. This study examined the feasibility of combining a lumboperitoneal (LP) shunt with an Ommaya reservoir to both control intracranial pressure and allow for intraventricular chemotherapy.
Methods
We identified 16 patients with LM who received both an Ommaya reservoir and an LP shunt, either concurrently or sequentially, and subsequently received intraventricular chemotherapy. The feasibility of this combination for intraventricular chemotherapy was evaluated by assessing 1) the distribution of intraventricularly injected drugs in CSF samples collected 0, 6, and 12 h post-injection and 2) adverse events associated with the procedure and drug administration.
Results
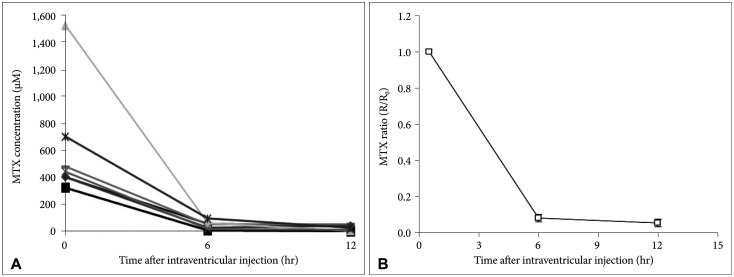
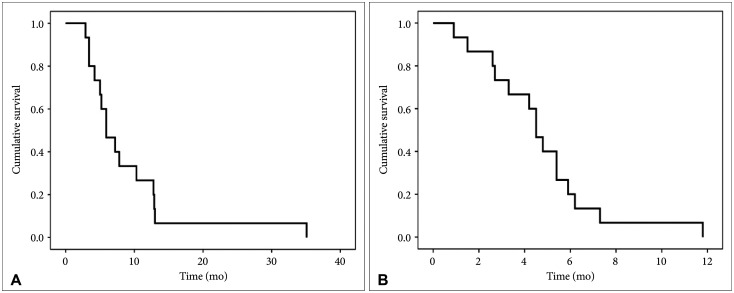
Patients received a median of seven rounds (range 1–37) of intraventricular chemotherapy during a median follow-up period of 5.2 months after LP shunt insertion. Pharmacokinetic data were obtained from six patients. Baseline methotrexate (MTX) levels from Ommaya reservoirs varied from 339.9 µM to 1,523.5 µM. CSF sampled from LP shunt reservoirs revealed an elimination halflife (t1/2) of 2.63 h, and the mean ratio of MTX concentration at 12 h to that at baseline was 0.05±0.05, ensuring drug distribution from the ventricle to the spinal canal. Nine patients (56%) underwent revision surgery due to catheter migration, malfunction, or infection. Among these patients, CSF infections attributable to intraventricular chemotherapy (n=3) occurred, but no infections occurred in later cases after we began to employ a complete aseptic technique.
Conclusion
LP shunt combined with Ommaya reservoir insertion is a feasible option for achieving both intracranial pressure control and the continuation of intraventricular chemotherapy in patients with LM.
Figure
Reference
-
2. Gwak HS, Lee SH, Park WS, Shin SH, Yoo H, Lee SH. Recent advancements of treatment for leptomeningeal carcinomatosis. J Korean Neurosurg Soc. 2015; 58:1–8. PMID: 26279806.
Article3. Morris PG, Reiner AS, Szenberg OR, Clarke JL, Panageas KS, Perez HR, et al. Leptomeningeal metastasis from non-small cell lung cancer: survival and the impact of whole brain radiotherapy. J Thorac Oncol. 2012; 7:382–385. PMID: 22089116.
Article4. Tetef ML, Margolin KA, Doroshow JH, Akman S, Leong LA, Morgan RJ Jr, et al. Pharmacokinetics and toxicity of high-dose intravenous methotrexate in the treatment of leptomeningeal carcinomatosis. Cancer Chemother Pharmacol. 2000; 46:19–26. PMID: 10912573.
Article5. Shapiro WR, Young DF, Mehta BM. Methotrexate: distribution in cerebrospinal fluid after intravenous, ventricular and lumbar injections. N Engl J Med. 1975; 293:161–166. PMID: 806016.
Article6. Boogerd W, van den Bent MJ, Koehler PJ, Heimans JJ, van der Sande JJ, Aaronson NK, et al. The relevance of intraventricular chemotherapy for leptomeningeal metastasis in breast cancer: a randomised study. Eur J Cancer. 2004; 40:2726–2733. PMID: 15571954.
Article7. Bokstein F, Lossos A, Siegal T. Leptomeningeal metastases from solid tumors: a comparison of two prospective series treated with and without intra-cerebrospinal fluid chemotherapy. Cancer. 1998; 82:1756–1763. PMID: 9576299.8. Chamberlain MC. Radioisotope CSF flow studies in leptomeningeal metastases. J Neurooncol. 1998; 38:135–140. PMID: 9696363.9. Blasberg RG, Patlak CS, Shapiro WR. Distribution of methotrexate in the cerebrospinal fluid and brain after intraventricular administration. Cancer Treat Rep. 1977; 61:633–641. PMID: 406996.10. Kim HS, Park JB, Gwak HS, Kwon JW, Shin SH, Yoo H. Clinical outcome of cerebrospinal fluid shunts in patients with leptomeningeal carcinomatosis. World J Surg Oncol. 2019; 17:59. PMID: 30917830.
Article11. Freilich RJ, Krol G, DeAngelis LM. Neuroimaging and cerebrospinal fluid cytology in the diagnosis of leptomeningeal metastasis. Ann Neurol. 1995; 38:51–57. PMID: 7611725.
Article12. Gwak HS, Lee CH, Yang HS, Joo J, Shin SH, Yoo H, et al. Chemoport with a non-collapsible chamber as a replacement for an Ommaya reservoir in the treatment of leptomeningeal carcinomatosis. Acta Neurochir (Wien). 2011; 153:1971–1978. PMID: 21796363.
Article13. Yoon JH, Gwak HS, Kwon JW, Shin SH, Yoo H. Clinical results of lumboperitoneal shunt with a valve reservoir compared with ventriculoperitoneal shunt. Nerve. 2017; 3:58–63.
Article14. Bloch O, McDermott MW. Lumboperitoneal shunts for the treatment of normal pressure hydrocephalus. J Clin Neurosci. 2012; 19:1107–1111. PMID: 22705135.
Article15. Hinderliter P, Saghir SA. Pharmacokinetics. Wexler P, editor. Encyclopedia of toxicology. 3rd ed. London: Academic Press/Elsevier;2014. p. 849–855.16. Balis FM, Blaney SM, McCully CL, Bacher JD, Murphy RF, Poplack DG. Methotrexate distribution within the subarachnoid space after intraventricular and intravenous administration. Cancer Chemother Pharmacol. 2000; 45:259–264. PMID: 10663645.
Article17. Jacobs A, Clifford P, Kay HE. The Ommaya reservoir in chemotherapy for malignant disease in the CNS. Clin Oncol. 1981; 7:123–129. PMID: 7249435.18. Obbens EA, Leavens ME, Beal JW, Lee YY. Ommaya reservoirs in 387 cancer patients: a 15-year experience. Neurology. 1985; 35:1274–1278. PMID: 3839573.
Article19. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982; 49:759–772. PMID: 6895713.
Article20. Gwak HS, Joo J, Kim S, Yoo H, Shin SH, Han JY, et al. Analysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non-small-cell lung cancer. J Thorac Oncol. 2013; 8:599–605. PMID: 23422833.21. Bleyer WA, Pizzo PA, Spence AM, Platt WD, Benjamin DR, Kolins CJ, et al. The Ommaya reservoir: newly recognized complications and recommendations for insertion and use. Cancer. 1978; 41:2431–2437. PMID: 274993.
Article22. Sandberg DI, Bilsky MH, Souweidane MM, Bzdil J, Gutin PH. Ommaya reservoirs for the treatment of leptomeningeal metastases. Neurosurgery. 2000; 47:49–54. discussion 54-5. PMID: 10917346.
Article23. Eisenberg HM, Davidson RI, Shillito J Jr. Lumboperitoneal shunts. Review of 34 cases. J Neurosurg. 1971; 35:427–431. PMID: 5133591.24. Eggenberger ER, Miller NR, Vitale S. Lumboperitoneal shunt for the treatment of pseudotumor cerebri. Neurology. 1996; 46:1524–1530. PMID: 8649541.25. Aschoff A, Kremer P, Hashemi B, Kunze S. The scientific history of hydrocephalus and its treatment. Neurosurg Rev. 1999; 22:67–93. discussion 94-5. PMID: 10547004.
Article26. Duthel R, Nuti C, Motuo-Fotso MJ, Beauchesne P, Brunon J. [Complications of lumboperitoneal shunts. A retrospective study of a series of 195 patients (214 procedures)]. Neurochirurgie. 1996; 42:83–89. discussion 89-90. PMID: 8952901.27. Menger RP, Connor DE Jr, Thakur JD, Sonig A, Smith E, Guthikonda B, et al. A comparison of lumboperitoneal and ventriculoperitoneal shunting for idiopathic intracranial hypertension: an analysis of economic impact and complications using the Nationwide Inpatient Sample. Neurosurg Focus. 2014; 37:E4.28. Burger MC, Wagner M, Franz K, Harter PN, Bähr O, Steinbach JP, et al. Ventriculoperitoneal shunts equipped with on-off valves for intraventricular therapies in patients with communicating hydrocephalus due to leptomeningeal metastases. J Clin Med. 2018; 7:216.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Safety and Efficiency of the H-Port for Treatment of Leptomeningeal Metastasis
- Therapeutic Trials in Two Cases with Chronic Meningitisvia Ommaya Reservoir
- Traumatic Subdural Hygroma Due to Injury of an Ommaya Reservoir: A Case Report
- Malignant Ascites after Subduroperitoneal Shunt in a Patient with Leptomeningeal Metastasis
- Posterior Fossa Migration of the Lumboperitoneal Shunt Catheter: A Case Report