J Korean Neurosurg Soc.
2024 Jul;67(4):467-476. 10.3340/jkns.2023.0178.
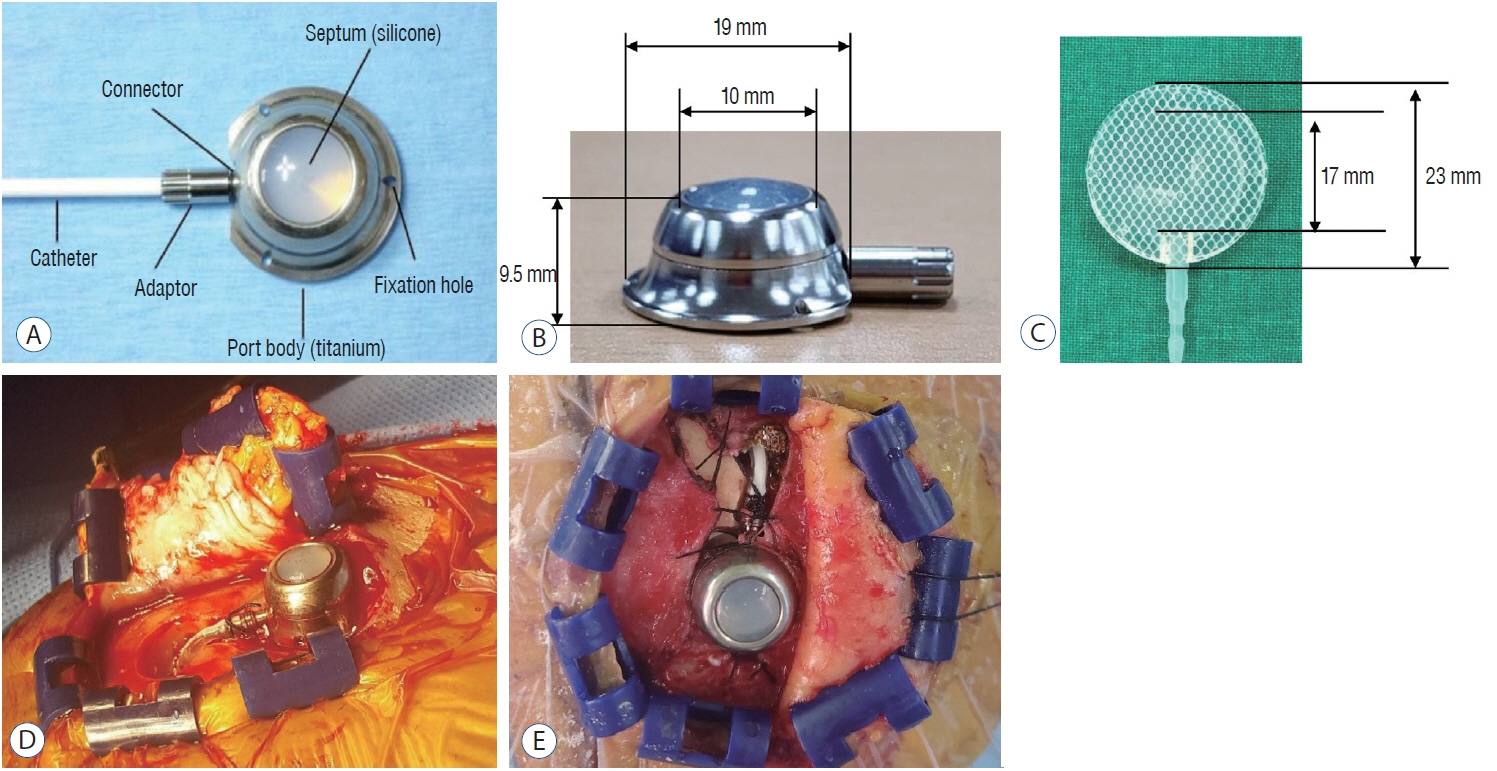
Clinical Safety and Efficiency of the H-Port for Treatment of Leptomeningeal Metastasis
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Cancer Control, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 3Neuro-Oncology Clinic, National Cancer Center, Goyang, Korea
- KMID: 2556744
- DOI: http://doi.org/10.3340/jkns.2023.0178
Abstract
Objective
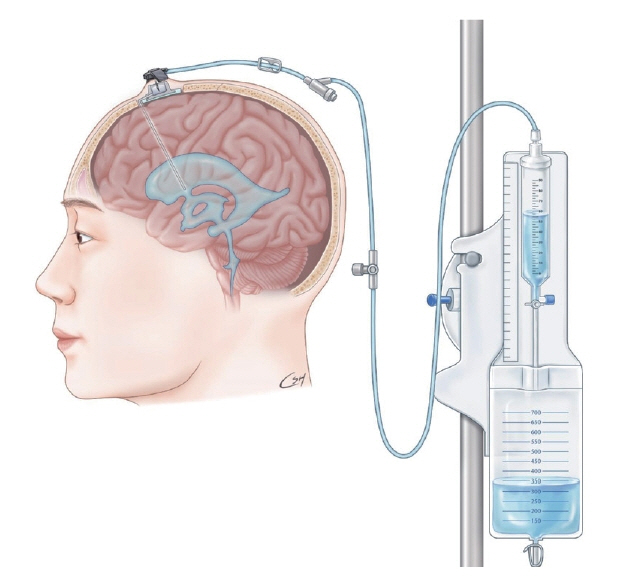
: To evaluate the usefulness of a cranial implantable chemoport, the H-port, as an alternative to the Ommaya reservoir for intraventricular chemotherapy/cerebrospinal fluid (CSF) access in patients with leptomeningeal metastasis (LM).
Methods
: One hundred fifty-two consecutive patients with a diagnosis of LM and who underwent H-port installation between 2015 and 2021 were evaluated. Adverse events associated with installation and intraventricular chemotherapy, and the rate of increased intracranial pressure (ICP) control via the port were evaluated for safety and efficacy. These indices were compared with published data of Ommaya (n=89), from our institution.
Results
: Time-to-install and installation-related complications of intracranial hemorrhage (n=2) and catheter malposition (n=5) were not significantly different between the two groups. Intraventricular chemotherapy-related complications of CSF leakage occurred more frequently in the Ommaya than in the H-port group (13/89 vs. 3/152, respectively, p<0.001). Intracranial hemorrhage during chemotherapy occurred only in the Ommaya group (n=4). The CSF infection rate was not statistically different between groups (14/152 vs. 12/89, respectively). The ICP control rate according to reservoir type revealed a significantly higher ICP control rate with the H-port (40/67), compared with the Ommaya result (12/58, p<0.001). Analyzing the ICP control rate based on the CSF drainage method, continuous extraventricular drainage (implemented only with the H-port), found a significantly higher ICP control rate than with intermittent CSF drainage (33/40 vs. 6/56, respectively, p<0.0001).
Conclusion
: The H-port for intraventricular chemotherapy in patients with LM was superior for ICP control; it had equal or lower complication rates than the Ommaya reservoir.
Figure
Reference
-
References
1. Bleyer WA, Pizzo PA, Spence AM, Platt WD, Benjamin DR, Kolins CJ, et al. The Ommaya reservoir: newly recognized complications and recommendations for insertion and use. Cancer. 41:2431–2437. 1978.
Article2. Byun YH, Gwak HS, Kwon JW, Kim KG, Shin SH, Lee SH, et al. A novel implantable cerebrospinal fluid reservoir : a pilot study. J Korean Neurosurg Soc. 61:640–644. 2018.
Article3. Chamberlain MC. Leptomeningeal metastases: a review of evaluation and treatment. J Neurooncol. 37:271–284. 1998.4. Chamberlain MC. Radioisotope CSF flow studies in leptomeningeal metastases. J Neurooncol. 38:135–140. 1998.5. Chamberlain MC, Kormanik P. Carcinoma meningitis secondary to nonsmall cell lung cancer: combined modality therapy. Arch Neurol. 55:506–512. 1998.
Article6. Chamberlain MC, Kormanik PA. Prognostic significance of 111 indiumDTPA CSF flow studies in leptomeningeal metastases. Neurology. 46:1674–1677. 1996.
Article7. Chamberlain MC, Kormanik PA, Barba D. Complications associated with intraventricular chemotherapy in patients with leptomeningeal metastases. J Neurosurg. 87:694–699. 1997.
Article8. Chen Y, Liu L, Zhu M. Intraventricular administration of antibiotics by ommaya reservoir for patients with multidrug-resistant Acinetobacter baumannii central nervous system infection. Br J Neurosurg. 35:170–173. 2021.
Article9. Gwak HS, Joo J, Kim S, Yoo H, Shin SH, Han JY, et al. Analysis of treatment outcomes of intraventricular chemotherapy in 105 patients for leptomeningeal carcinomatosis from non-small-cell lung cancer. J Thorac Oncol. 8:599–605. 2013.
Article10. Gwak HS, Lee CH, Yang HS, Joo J, Shin SH, Yoo H, et al. Chemoport with a non-collapsible chamber as a replacement for an Ommaya reservoir in the treatment of leptomeningeal carcinomatosis. Acta Neurochir (Wien). 153:1971–1978. discussion 1978. 2011.
Article11. Hitchins RN, Bell DR, Woods RL, Levi JA. A prospective randomized trial of single-agent versus combination chemotherapy in meningeal carcinomatosis. J Clin Oncol. 5:1655–1662. 1987.
Article12. Jacobs A, Clifford P, Kay HE. The Ommaya reservoir in chemotherapy for malignant disease in the CNS. Clin Oncol. 7:123–129. 1981.13. Jung TY, Chung WK, Oh IJ. The prognostic significance of surgically treated hydrocephalus in leptomeningeal metastases. Clin Neurol Neurosurg. 119:80–83. 2014.
Article14. Kim HS, Park JB, Gwak HS, Kwon JW, Shin SH, Yoo H. Clinical outcome of cerebrospinal fluid shunts in patients with leptomeningeal carcinomatosis. World J Surg Oncol. 17:59. 2019.
Article15. Lee TL, Kumar A, Baratham G. Intraventricular morphine for intractable craniofacial pain. Singapore Med J. 31:273–276. 1990.16. Lemann W, Wiley RG, Posner JB. Leukoencephalopathy complicating intraventricular catheters: clinical, radiographic and pathologic study of 10 cases. J Neurooncol. 6:67–74. 1988.
Article17. Lishner M, Perrin RG, Feld R, Messner HA, Tuffnell PG, Elhakim T, et al. Complications associated with Ommaya reservoirs in patients with cancer. The Princess Margaret Hospital experience and a review of the literature. Arch Intern Med. 150:173–176. 1990.
Article18. Liu HG, Liu DF, Zhang K, Meng FG, Yang AC, Zhang JG. Clinical application of a neurosurgical robot in intracranial ommaya reservoir implantation. Front Neurorobot. 15:638633. 2021.
Article19. Obbens EA, Leavens ME, Beal JW, Lee YY. Ommaya reservoirs in 387 cancer patients: a 15-year experience. Neurology. 35:1274–1278. 1985.20. Ommaya AK. Subcutaneous reservoir and pump for sterile access to ventricular cerebrospinal fluid. Lancet. 2:983–984. 1963.
Article21. Ongerboer de Visser BW, Somers R, Nooyen WH, van Heerde P, Hart AA, McVie JG. Intraventricular methotrexate therapy of leptomeningeal metastasis from breast carcinoma. Neurology. 33:1565–1572. 1983.
Article22. Rogers LR, Barnett G. Percutaneous aspiration of brain tumor cysts via the Ommaya reservoir system. Neurology. 41(2_part_1):279–282. 1991.
Article23. Sandberg DI, Bilsky MH, Souweidane MM, Bzdil J, Gutin PH. Ommaya reservoirs for the treatment of leptomeningeal metastases. Neurosurgery. 47:49–54. discussion 54-55. 2000.
Article24. Taillibert S, Laigle-Donadey F, Chodkiewicz C, Sanson M, Hoang-Xuan K, Delattre JY. Leptomeningeal metastases from solid malignancy: a review. J Neurooncol. 75:85–99. 2005.
Article25. Takahashi M, Yamada R, Tabei Y, Nakamura O, Shinoura N. Navigationguided Ommaya reservoir placement: implications for the treatment of leptomeningeal metastases. Minim Invasive Neurosurg. 50:340–345. 2007.
Article26. Vinchurkar KM, Maste P, Togale MD, Pattanshetti VM. Chemoportassociated complications and its management. Indian J Surg Oncol. 11:394–397. 2020.
Article27. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 49:759–772. 1982.
Article28. Zubair A, De Jesus O. Ommaya Reservoir. StatPearls. Treasure Island: StatPearls Publishing;2022.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Cancer with Leptomeningeal Metastasis
- A Case of Leptomeningeal Metastasis Associated with Cerebral Venous Thrombosis
- Diagnostic Value of Cerebrospinal Fluid Level of Carcinoembryonic Antigen in Patients with Leptomeningeal Carcinomatous Metastasis
- Malignant Ascites after Subduroperitoneal Shunt in a Patient with Leptomeningeal Metastasis
- Incidentally Found Port Site Metastasis followings Laparoscopic Radical Nephrectomy for a Renal Cell Carcinoma