J Korean Med Sci.
2022 Oct;37(40):e295. 10.3346/jkms.2022.37.e295.
The First Systematic Gastroscopy Training Program for Surgeons in Korea
- Affiliations
-
- 1Division of Gastrointestinal Surgery, Department of Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2534334
- DOI: http://doi.org/10.3346/jkms.2022.37.e295
Abstract
- Background
Endoscopic evaluation of the stomach is essential for preoperative planning and post-surgical surveillance for various diseases of the stomach, including malignancy. The gastroscopy education program for surgeons is currently in its infancy and is not systematically organized in Korea. This study aimed to introduce the first systematic gastroscopy education program for surgeons in Korea.
Methods
The gastroscopy education program entitled “Gastroscopy School for Surgeons (GSS)” comprised of theoretical education, dry lab hands-on training, and clinical practice. All participants were beginners without any gastroscopy experience. Clinical practice started after the completion of the theoretical and dry lab training. The gastroscopy practices utilized simple luminal observation, biopsy, localization using clips or dye injection, and limited therapeutic gastroscopy. The educational performances and surveys from 33 participants were analyzed.
Results
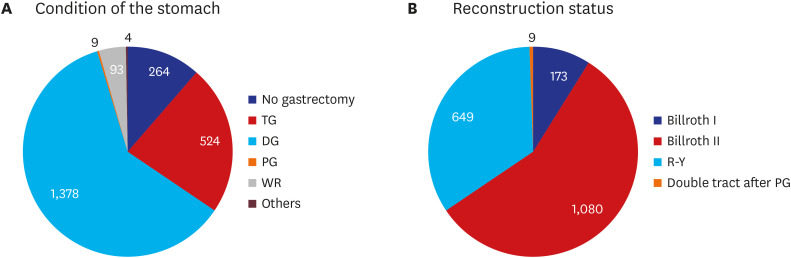
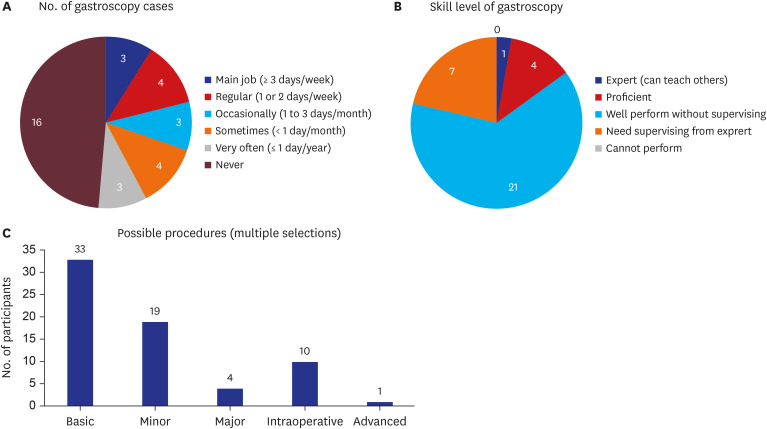
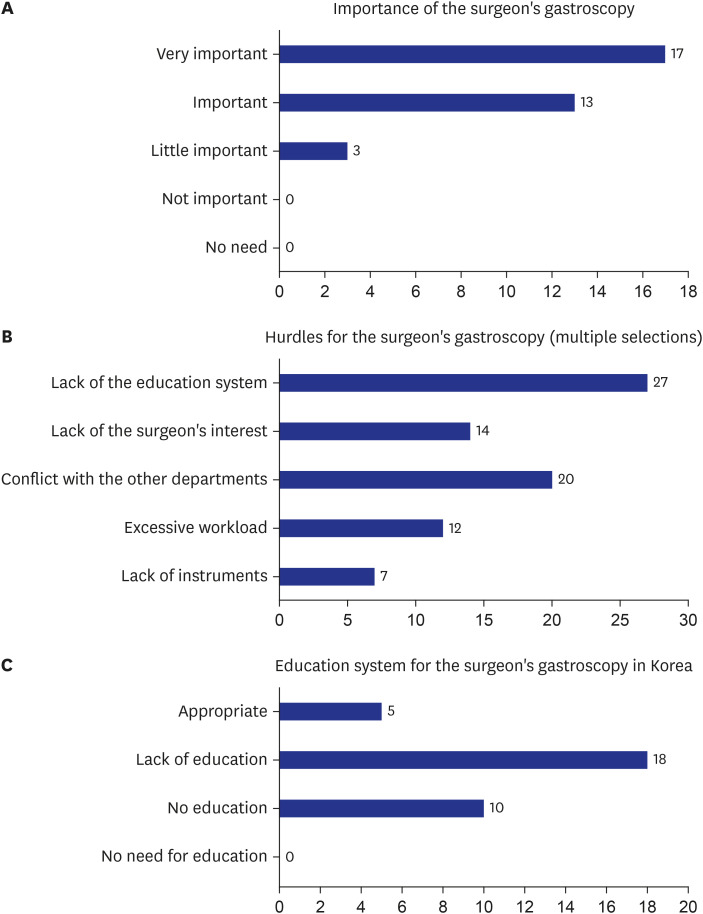
The participants consisted of surgical residents, general surgeons, gastrointestinalspecialized surgeons, and physicians. Participants performed a total of 2,272 gastroscopies, 2,008 of which were post-gastrectomy cases. Currently, of the 33 participants, 7 (21.2%) of the participants performed gastroscopy regularly, and 7 (21.2%) occasionally. According to the self-reported survey, one participant assessed their current gastroscopic technique to be at the expert level, and 25 (75.8%) at a proficient level. All participants considered gastroscopy education for surgeons to be necessary, and 28 (84.8%) stated that systematic education is not currently provided in Korea.
Conclusion
We introduced the first systematic gastroscopy education program for surgeons in Korea, namely the GSS, which is practical and meets clinical needs. More training centers are needed to expand gastroscopy training among Korean surgeons.
Keyword
Figure
Reference
-
1. Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002; 5(2):83–89. PMID: 12111583.
Article2. Seo HS, Yoo HM, Jung YJ, Lee SH, Park JM, Song KY, et al. Regional lymph node dissection as an additional treatment option to endoscopic resection for expanded indications in gastric cancer: a prospective cohort study. J Gastric Cancer. 2020; 20(4):442–453. PMID: 33425445.
Article3. Gotoda T. Endoscopic resection of early gastric cancer: the Japanese perspective. Curr Opin Gastroenterol. 2006; 22(5):561–569. PMID: 16891890.
Article4. Haga Y, Hiki N, Kinoshita T, Ojima T, Nabeya Y, Kuwabara S, et al. Treatment option of endoscopic stent insertion or gastrojejunostomy for gastric outlet obstruction due to gastric cancer: a propensity score-matched analysis. Gastric Cancer. 2020; 23(4):667–676. PMID: 31982964.
Article5. Lee SR, Kim HO, Park JH, Yoo CH. clinical outcomes of endoscopic metal stent placement for esophagojejunostomy leakage after total gastrectomy for gastric adenocarcinoma. Surg Laparosc Endosc Percutan Tech. 2018; 28(2):113–117. PMID: 29509565.
Article6. Han ES, Seo HS, Kim JH, Lee HH. Surveillance endoscopy guidelines for postgastrectomy patients based on risk of developing remnant gastric cancer. Ann Surg Oncol. 2020; 27(11):4216–4224. PMID: 32372310.
Article7. Jung Y, Kim JW, Im JP, Cho YK, Lee TH, Jang JY. Safety of gastrointestinal endoscopy in Korea: a nationwide survey and population-based study. J Korean Med Sci. 2022; 37(4):e24. PMID: 35075823.
Article8. Moon HS, Choi EK, Seo JH, Moon JS, Song HJ, Kim KO, et al. Education and training guidelines for the board of the Korean Society of Gastrointestinal Endoscopy. Clin Endosc. 2017; 50(4):345–356. PMID: 28783925.
Article9. Kim JS, Kim BW. Endoscopy training in Korea. Korean J Intern Med. 2019; 34(2):237–241. PMID: 30840806.
Article10. Park DJ, Lee HJ, Kim SG, Jung HC, Song IS, Lee KU, et al. Intraoperative gastroscopy for gastric surgery. Surg Endosc. 2005; 19(10):1358–1361. PMID: 16193377.
Article11. Hur H, Son SY, Cho YK, Han SU. Intraoperative gastroscopy for tumor localization in laparoscopic surgery for gastric adenocarcinoma. J Vis Exp. 2016; (114):53170.
Article12. Park SH, Lee HJ, Park JH, Kim TH, Son YG, Huh YJ, et al. Clinical significance of intra-operative gastroscopy for tumor localization in totally laparoscopic partial gastrectomy. J Gastrointest Surg. 2021; 25(5):1134–1146. PMID: 32989692.
Article13. Park JH, Jeong SH, Lee YJ, Kim TH, Kim JM, Kim DH, et al. Safety and efficacy of post-anastomotic intraoperative endoscopy to avoid early anastomotic complications during gastrectomy for gastric cancer. Surg Endosc. 2020; 34(12):5312–5319. PMID: 31834512.
Article14. An JY, Min JS, Hur H, Lee YJ, Cho GS, Park YK, et al. Laparoscopic sentinel node navigation surgery versus laparoscopic gastrectomy with lymph node dissection for early gastric cancer: short-term outcomes of a multicentre randomized controlled trial (SENORITA). Br J Surg. 2020; 107(11):1429–1439. PMID: 32492186.
Article15. Bradley NL, Bazzerelli A, Lim J, Wu Chao Ying V, Steigerwald S, Strickland M, et al. Endoscopy training in Canadian general surgery residency programs. Can J Surg. 2015; 58(3):150–152. PMID: 26011848.
Article16. Vo DM, Gauvin JM, Chen SL. Endoscopy education in general surgery residencies: meeting the new RRC requirements. J Surg Res. 2010; 163(2):210–213. PMID: 20605613.
Article17. Miller GE. The assessment of clinical skills/competence/performance. Acad Med. 1990; 65(9):Suppl. S63–S67. PMID: 2400509.
Article18. McCallum M, Curran-Smith J, Wojnar D, Williamson S. Evaluating the impact of organizational learning initiatives. J Nurses Staff Dev. 2002; 18(4):177–183. PMID: 12235416.
Article19. Zajaczkowski T. Johann Anton von Mikulicz-Radecki (1850-1905)--a pioneer of gastroscopy and modern surgery: his credit to urology. World J Urol. 2008; 26(1):75–86. PMID: 18074140.
Article20. Morgenthal CB, Richards WO, Dunkin BJ, Forde KA, Vitale G, Lin E, et al. The role of the surgeon in the evolution of flexible endoscopy. Surg Endosc. 2007; 21(6):838–853. PMID: 17180263.
Article21. Hilsden RJ, Tepper J, Moayyedi P, Rabeneck L. Who provides gastrointestinal endoscopy in Canada? Can J Gastroenterol. 2007; 21(12):843–846. PMID: 18080058.
Article22. Yıldız İ, Koca YS, Bülbül MT, Musri ÖC. Emergency endoscopy and the importance of endoscopy training in general surgery residency: a survey-based study. Med Sci Monit. 2017; 23:5184–5188. PMID: 29084936.
Article23. Xuan Y, Hur H, Byun CS, Han SU, Cho YK. Efficacy of intraoperative gastroscopy for tumor localization in totally laparoscopic distal gastrectomy for cancer in the middle third of the stomach. Surg Endosc. 2013; 27(11):4364–4370. PMID: 23780327.
Article24. Kwon IG, Son T, Kim HI, Hyung WJ. Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg. 2019; 154(2):150–158. PMID: 30427990.
Article25. Roh CK, Choi S, Seo WJ, Cho M, Son T, Kim HI, et al. Indocyanine green fluorescence lymphography during gastrectomy after initial endoscopic submucosal dissection for early gastric cancer. Br J Surg. 2020; 107(6):712–719. PMID: 32031248.
Article26. Nunobe S, Hiki N, Gotoda T, Murao T, Haruma K, Matsumoto H, et al. Successful application of laparoscopic and endoscopic cooperative surgery (LECS) for a lateral-spreading mucosal gastric cancer. Gastric Cancer. 2012; 15(3):338–342. PMID: 22350555.
Article27. Min JS, Seo KW, Jeong SH. Choice of LECS procedure for benign and malignant gastric tumors. J Gastric Cancer. 2021; 21(2):111–121. PMID: 34234973.
Article28. De Bie C, Bronswijk M, Vanella G, Pérez-Cuadrado-Robles E, van Malenstein H, Laleman W, et al. EUS-guided hepaticogastrostomy for patients with afferent loop syndrome: a comparison with EUS-guided gastroenterostomy or percutaneous drainage. Surg Endosc. 2022; 36(4):2393–2400. PMID: 33909126.
Article29. Bell RL, Reinhardt KE, Flowers JL. Surgeon-performed endoscopic dilatation of symptomatic gastrojejunal anastomotic strictures following laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2003; 13(5):728–733. PMID: 14627467.
Article30. Seo HS, Jung YJ, Kim JH, Park CH, Lee HH. Three-port right-side approach-duet totally laparoscopic distal gastrectomy for uncut Roux-en-Y reconstruction. J Laparoendosc Adv Surg Tech A. 2018; 28(9):1109–1114. PMID: 30088978.
Article31. Lee I, Oh Y, Park SH, Kwon Y, Park S. Postoperative nutritional outcomes and quality of life-related complications of proximal versus total gastrectomy for upper-third early gastric cancer: a meta-analysis. Sci Rep. 2020; 10(1):21460. PMID: 33293604.
Article32. Park JH, Kong SH, Choi JH, Park SH, Suh YS, Park DJ, et al. Proximal anterior-antrum posterior (PAAP) overlapping anastomosis in minimally invasive pylorus-preserving gastrectomy for early gastric cancer located in the high body and posterior wall of the stomach. J Gastric Cancer. 2020; 20(3):277–289. PMID: 33024584.
Article33. Ekkelenkamp VE, Koch AD, de Man RA, Kuipers EJ. Training and competence assessment in GI endoscopy: a systematic review. Gut. 2016; 65(4):607–615. PMID: 25636697.
Article34. Waschke KA, Anderson J, Valori RM, MacIntosh DG, Kolars JC, DiSario JA, et al. ASGE principles of endoscopic training. Gastrointest Endosc. 2019; 90(1):27–34. PMID: 31122745.
Article35. Pearl JP, Marks JM. The future of teaching surgical endoscopy. Surg Innov. 2006; 13(4):280–282. PMID: 17227927.
Article36. Morales MP, Mancini GJ, Miedema BW, Rangnekar NJ, Koivunen DG, Ramshaw BJ, et al. Integrated flexible endoscopy training during surgical residency. Surg Endosc. 2008; 22(9):2013–2017. PMID: 18297358.
Article37. Subhas G, Gupta A, Mittal VK. Necessity for improvement in endoscopy training during surgical residency. Am J Surg. 2010; 199(3):331–334. PMID: 20226905.
Article38. Fonseca AL, Reddy V, Yoo PS, Gusberg RJ, Longo WE. Senior surgical resident confidence in performing flexible endoscopy: What can we do differently? J Surg Educ. 2016; 73(2):311–316. PMID: 26531744.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Taking More Gastroscopy Images Increases the Detection Rate of Clinically Significant Gastric Lesions: Validation of a Systematic Screening Protocol for the Stomach
- Residency training: training program renewal and evaluation of training
- Current Endoscopy Training in Korea and Future Aspects
- Residency training guideline for esophagogastroduodenoscopy skills in family practice
- Residents' Expectation of Family Medicine-Specific Training Program and Its Current State