J Cerebrovasc Endovasc Neurosurg.
2022 Sep;24(3):210-220. 10.7461/jcen.2022.E2021.03.008.
Middle meningeal artery: An effective pathway for achieving complete obliteration following transarterial Ethylene Vinyl Copolymer (Onyx) embolization of dural arteriovenous fistulas
- Affiliations
-
- 1Neurosurgical Service, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
- 2Department of Neurosurgry, Iwate Medical University, Yahaba, Japan
- 3Department of Neurosurgery University of California San Francisco, San Francisco, CA, USA
- 4Division of Interventional Neuroradiology, Department of Radiology, University of Massachusetts Medical Center, Worcester, MA, USA
- 5Department of Neurological Surgery, Cooper University Health Care, Camden, NJ, USA
- KMID: 2533672
- DOI: http://doi.org/10.7461/jcen.2022.E2021.03.008
Abstract
Objective
Transarterial Onyx embolization is the mainstay of intracranial non-cavernous dural arteriovenous fistulas (dAVFs) treatment. Although the dural arterial supply varies depending on the location, the impact of arterial access on treatment outcomes has remained unclear. The aim of this study was to characterize factors as sociated with complete obliteration following transarterial Onyx embolization, with a special focus on arterial access routes and dAVF location.
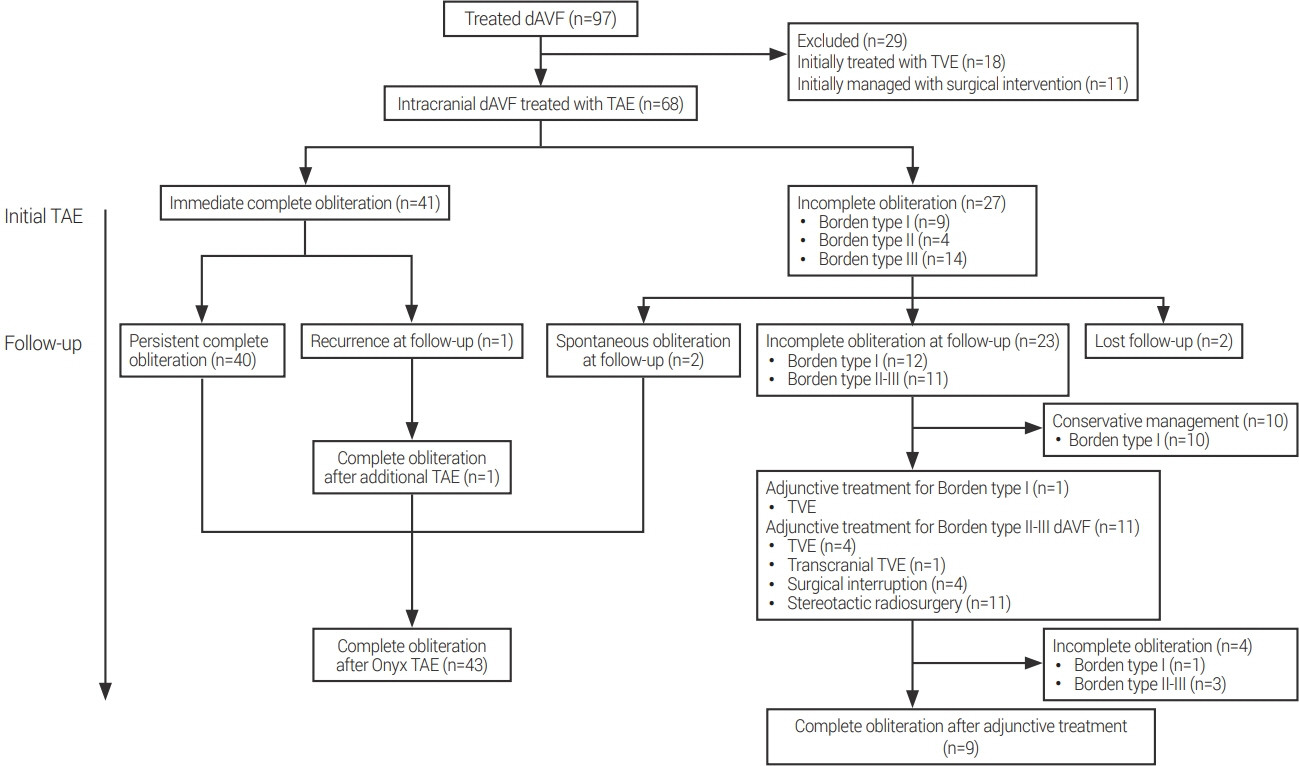
Methods
A retrospective analysis of the patients who underwent transarterial Onyx embolization for intracranial dAVFs at two academic institutions was performed. Patients with angiographic follow-up were considered eligible to investigate the impact of the arterial access on achieving complete obliteration.
Results
Sixty-eight patients underwent transarterial Onyx embolization of intracranial dAVFs. Complete obliteration was achieved in 65% of all treated patients and in 75% of those with cortical venous reflux. Multivariable analysis identified middle meningeal artery (MMA) access to be a significant independent predictive factor for complete obliteration (OR, 2.32; 95% CI, 1.06-5.06; p=0.034). Subgroup analysis showed that supratentorial and lateral cerebellar convexity dAVFs (OR, 5.72, 95% CI, 1.89-17.33, p=0.002), and Borden type III classification at pre-treatment (OR, 3.13, 95% CI, 1.05- 9.35, p=0.041), were independent predictive factors for complete obliteration following embolization through the MMA.
Conclusions
MMA access is an independent predictive factor for complete obliteration following transarterial Onyx embolization for intracranial non-cavernous dAVFs. It is particularly effective for supratentorial and lateral cerebellar convexity dAVFs and those that are Borden type III.
Keyword
Figure
Reference
-
1. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; Feb. 82(2):166–79.
Article2. Cha KC, Yeon JY, Kim GH, Jeon P, Kim JS, Hong SC. Clinical and angiographic results of patients with dural arteriovenous fistula. J Clin Neurosci. 2013; Apr. 20(4):536–42.
Article3. Chandra RV, Leslie-Mazwi TM, Mehta BP, Yoo AJ, Rabinov JD, Pryor JC, et al. Transarterial Onyx embolization of cranial dural arteriovenous fistulas: long-term follow-up. AJNR Am J Neuroradiol. 2014; Sep. 35(9):1793–7.
Article4. Chapot R, Stracke P, Velasco A, Nordmeyer H, Heddier M, Stauder M, et al. The pressure cooker technique for the treatment of brain AVMs. J Neuroradiol. 2014; Mar. 41(1):87–91.
Article5. De Keukeleire K, Vanlangenhove P, Kalala Okito JP, Hallaert G, Van Roost D, Defreyne L. Transarterial embolization with Onyx for treatment of intracranial non-cavernous dural arteriovenous fistula with or without cortical venous reflux. J Neurointerv Surg. 2011; Sep. 3(3):224–8.
Article6. Kim B, Jeon P, Kim K, Kim S, Kim H, Byun HS, et al. Predictive factors for response of intracranial dural arteriovenous fistulas to transarterial Onyx embolization: angiographic subgroup analysis of treatment outcomes. World Neurosurg. 2016; Apr. 88:609–18.
Article7. Mantilla D, Le Corre M, Cagnazzo F, Gascou G, Eker O, Machi P, et al. Outcome of transarterial treatment of dural arteriovenous fistulas with direct or indirect cortical venous drainage. J Neurointerv Surg. 2018; Oct. 10(10):958–63.
Article8. Martins C, Yasuda A, Campero A, Ulm AJ, Tanriover N, Rhoton A Jr. Microsurgical anatomy of the dural arteries. Neurosurgery. 2005; Apr. 56(2 Suppl):211–51. discussion 211-51.
Article9. Sadeh-Gonike U, Magand N, Armoiry X, Riva R, Labeyrie PE, Lamy B, et al. Transarterial Onyx embolization of intracranial dural fistulas: a prospective cohort, systematic review, and meta-analysis. Neurosurgery. 2018; Jun. 82(6):854–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Dural Arteriovenous Fistulas: Single Center Experience
- A Case of Intraosseous Dural Arteriovenous Fistulas Involving Diploic Vein Treated with Transarterial Onyx Embolization
- Transcranial Direct Middle Meningeal Artery Puncture for the Onyx Embolization of Dural Arteriovenous Fistula Involving the Superior Sagittal Sinus
- Hairball-Like Migration of “Onyx Threads” into the Draining Vein during Transarterial Embolization of a Dural Arteriovenous Fistula: A Case Report and Experimental Validation
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)