J Korean Neurosurg Soc.
2022 Sep;65(5):741-750. 10.3340/jkns.2022.0087.
A Nationwide Study on the Impact of COVID-19 Pandemic on Volume of Spine Surgery in South Korea
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 2Department of Neurosurgery, Soonchunhyang University Gumi Hospital, Gumi, Korea
- KMID: 2533036
- DOI: http://doi.org/10.3340/jkns.2022.0087
Abstract
Objective
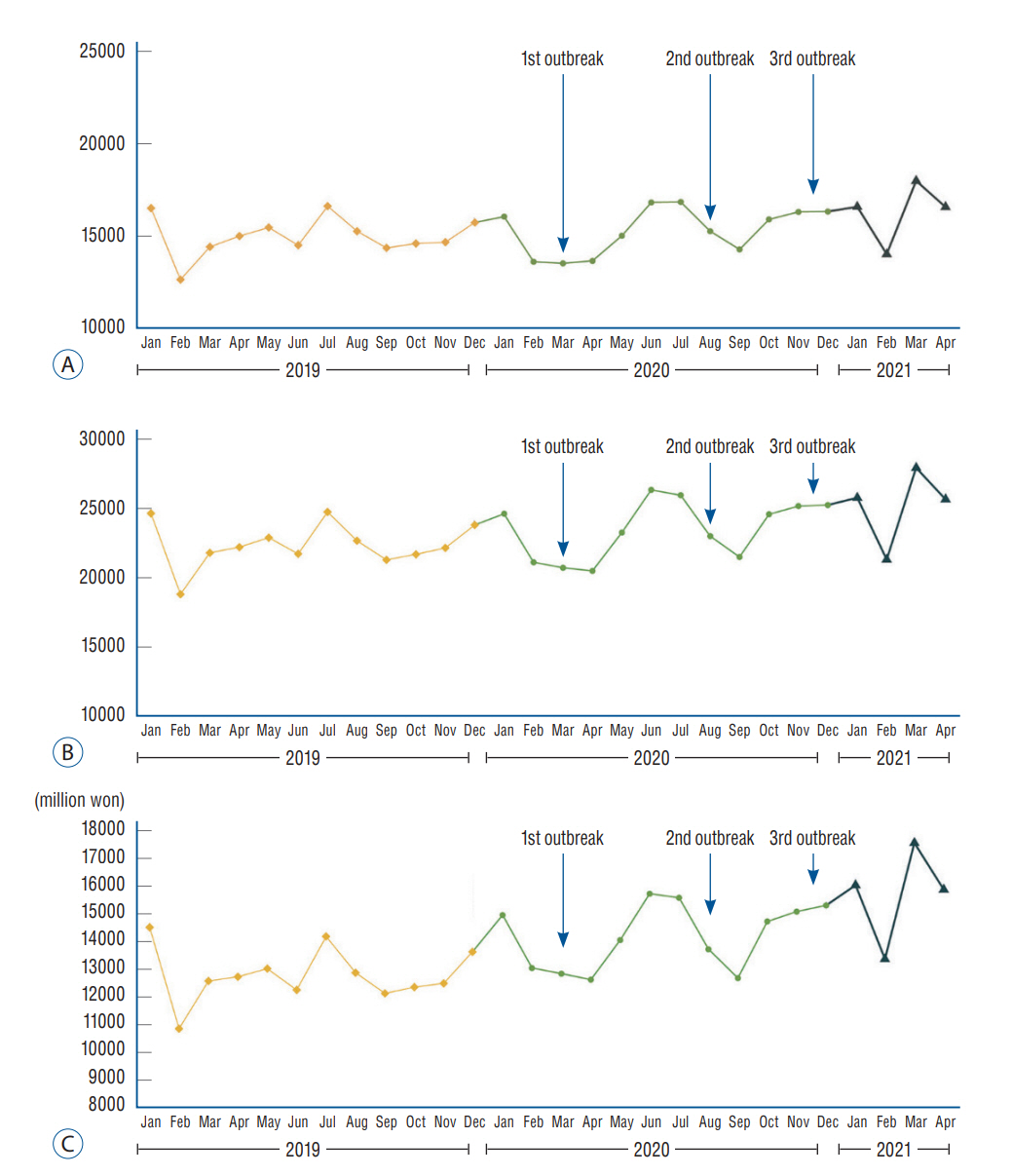
: In March 2020, World Health Organization declared a global pandemic caused by a novel coronavirus (SARS-CoV-2). The disease caused by this virus is called COVID-19. Due to its high contagiousness, many changes have occurred in overall areas of our daily life including hospital use by patients. The aim of this study was to investigate the impact of COVID-19 on volume of spine surgery in South Korea using the National Health Insurance database and compare it with the volume of a homologous period before the pandemic.
Methods
: Data of related to spine surgery from January 2019 to April 2021 were obtained from the National Health Insurance and Health Insurance Review and Assessment Service database. Primary outcomes were total number of patients, rate of patients per 100000 population, and total number of procedures. The number of patients by hospital size was also analyzed.
Results
: COVID-19 outbreaks occurred in South Korea in March, August, and December of 2020. Compared to the previous year, the total number of patients who underwent spinal surgery showed a decrease for 2–3 months after the first and second outbreaks. However, it showed an increasing trend after the third outbreak. The same pattern was observed in terms of the ratio of the number of patients per 100000 population. Between 2019 and 2021, the mean number of spine surgeries per month tended to increase. Mean annual medical expenses increased over the years (p=0.001). When the number of spine surgeries was analyzed by hospital size, proportion of tertiary general hospital in 2021 increased compared to those in 2019 and 2020 (vs. 2019, p=0.012; vs. 2020, p=0.016). The proportion of general hospital was significantly decreased in 2020 compared to that in 2019 (p=0.037).
Conclusion
: After the COVID-19 outbreak, patients tended to postpone spinal surgery temporarily. The number of spinal surgeries decreased for 2–3 months after the first and second outbreaks. However, as the ability to respond to the COVID-19 pandemic at the hospital and society-wide level gradually increased, the number of spine surgeries did not decrease after the third outbreak in December 2020. In addition, the annual number of spine surgeries continued to increase. However, it should be noted that patients tend to be increasingly concentrated in tertiary hospitals for spinal surgery.
Keyword
Figure
Cited by 1 articles
-
Editor’s Pick in July 2023
Bum-Tae Kim
J Korean Neurosurg Soc. 2023;66(4):341-343. doi: 10.3340/jkns.2023.0117.
Reference
-
References
1. American College of Surgeons : Clinical issues and guidance. Available at : https://www.facs.org/covid-19/clinical-guidance.2. Bregman DE, Cook T, Thorne C. Estimated national and regional impact of COVID-19 on elective case volume in aesthetic plastic surgery. Aesthet Surg J. 41:358–369. 2021.3. Carlos WG, Dela Cruz CS, Cao B, Pasnick S, Jamil S. Novel Wuhan (2019-nCoV) coronavirus. Am J Respir Crit Care Med. 201:P7–P8. 2020.4. Centers for Disease Control and Prevention : Healthcare Workers: Information on COVID-19. Available at : https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html.5. Chang DG, Park JB, Baek GH, Kim HJ, Bosco A, Hey HWD, et al. The impact of COVID-19 pandemic on orthopaedic resident education: a nationwide survey study in South Korea. Int Orthop. 44:2203–2210. 2020.6. Chapon R, Meyblum J, Simon L, Pelletier Y, Broussolle T, Marty H, et al. Global French Spine Surgery Activity: Executive Report of Demographics Data and Trends. Available at : https://doi.org/10.21203/rs.3.rs-1260367/v1.7. Choi JY. COVID-19 in South Korea. Postgrad Med J. 96:399–402. 2020.8. GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 388:1545–1602. 2016.9. Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice : preliminary report from a single (regional) university hospital in Republic of Korea. J Korean Neurosurg Soc. 63:407–414. 2020.10. Health Insurance Review & Assessment Service : Treatment practice of public interest. Available at : https://opendata.hira.or.kr/.11. Hussain A, Mahawar K, El-Hasani S. The impact of COVID-19 pandemic on obesity and bariatric surgery. Obes Surg. 30:3222–3223. 2020.12. Jain NS, Alluri RK, Schopler SS, Hah R, Wang JC. COVID-19 and spine surgery: a review and evolving recommendations. Global Spine J. 10:528–533. 2020.13. Lauer SA, Grantz KH, Bi Q, Jones FK, Zheng Q, Meredith HR, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 172:577–582. 2020.14. Lee MH, Jang SR, Lee TK. Comparative analysis of COVID-19 outbreak and changes in neurosurgical emergency patients. J Korean Neurosurg Soc. 65:130–137. 2022.15. Li LQ, Huang T, Wang YQ, Wang ZP, Liang Y, Huang TB, et al. COVID-19 patients' clinical characteristics, discharge rate, and fatality rate of meta-analysis. J Med Virol. 92:577–583. 2020.16. Mackay ND, Wilding CP, Langley CR, Young J. The impact of COVID-19 on trauma and orthopaedic patients requiring surgery during the peak of the pandemic: a retrospective cohort study. Bone Jt Open. 1:520–529. 2020.17. Noureldine MHA, Pressman E, Krafft PR, Greenberg MS, Agazzi S, van Loveren H, et al. Impact of the COVID-19 pandemic on neurosurgical practice at an academic tertiary referral center: a comparative study. World Neurosurg. 139:e872–e876. 2020.18. O'Connell RM, Khan MA, Amir M, Bucheeri M, Khan W, Khan IZ, et al. The impact of COVID-19 on emergency general surgery admissions and operative volumes: a single centre experience. Surgeon. 19:e207–e212. 2021.19. Okuno T, Takada D, Shin JH, Morishita T, Itoshima H, Kunisawa S, et al. Impact of the coronavirus disease 2019 pandemic on surgical volume in Japan: a cohort study using administrative data. Available at : https://doi.org/10.1101/2020.11.18.20233882.20. Ozoner B, Gungor A, Hasanov T, Toktas ZO, Kilic T. Neurosurgical practice during coronavirus disease 2019 (COVID-19) pandemic. World Neurosurg. 140:198–207. 2020.21. Prost S, Charles YP, Allain J, Barat JL, d'Astorg H, Delhaye M, et al. French Spine Surgery Society guidelines for management of spinal surgeries during COVID-19 pandemic. World J Clin Cases. 8:1756–1762. 2020.22. Rocco B, Sighinolfi MC, Sandri M, Altieri V, Amenta M, Annino F, et al. The dramatic COVID 19 outbreak in Italy is responsible of a huge drop of urological surgical activity: a multicenter observational study. BJU Int. 127:56–63. 2021.23. Royal College of Surgeons of England : COVID-19. Available at : https://www.rcseng.ac.uk/coronavirus/.24. Sarac NJ, Sarac BA, Schoenbrunner AR, Janis JE, Harrison RK, Phieffer LS, et al. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. J Bone Joint Surg Am. 102:942–945. 2020.25. Saraswathula A, Gourin CG, Stewart CM. National trends in US otolaryngology surgical volume during the early COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 147:397–399. 2021.26. Soh TLT, Ho SWL, Yap WMQ, Oh JY. Spine surgery and COVID-19: challenges and strategies from the front lines. J Bone Joint Surg Am. 102:e56. 2020.27. Stinner DJ, Lebrun C, Hsu JR, Jahangir AA, Mir HR. The orthopaedic trauma service and COVID-19: practice considerations to optimize outcomes and limit exposure. J Orthop Trauma. 34:333–340. 2020.28. Tanaka M, Kanayama M, Hashimoto T, Oha F, Shimamura Y, Tsujimoto T, et al. Trends of spine surgeries during the first COVID-19 semilockdown: survey in a non-epidemic region in Japan. Spine Surg Relat Res. 6:109–114. 2022.29. The North American Spine Society : NASS Guidance Document on Elective, Emergent and Urgent Procedures. Available at : https://www.spine.org/COVID-19.30. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 581:465–469. 2020.31. Wolrd Health Organization : Coronavirus disease (COVID-19) pandemic. Available at : https://www.who.int/emergencies/diseases/novelcoronavirus-2019.32. Wordie SJ, Tsirikos AI. The impact of the COVID-19 pandemic on spinal surgery. Orthop Trauma. 35:314–320. 2021.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of the COVID-19 Pandemic on Esophagogastroduodenoscopy and Gastric Cancer Claims in South Korea: A Nationwide, Population-Based Study
- The COVID-19 pandemic's impact on prostate cancer screening and diagnosis in Korea
- The impact of the COVID-19 pandemic on clinical practices related to colorectal cancer and colonoscopy in South Korea: a nationwide population-based study
- The coronavirus disease 2019 pandemic and chronic diseases
- Impact of COVID-19 Pandemic on Performance of Gastrointestinal Endoscopy