Korean J Gastroenterol.
2022 Aug;80(2):93-98. 10.4166/kjg.2022.023.
Ischemic Colitis Presented as Pseudomembranous Colitis: An Untypical Case from Vietnam
- Affiliations
-
- 1Department of Internal Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 2Department of Gastroenterology, Gia-Dinh People's Hospital, Ho Chi Minh City, Vietnam
- 3Department of Pathology and Forensic Medicine, Pham Ngoc Thach University of Medicine, Ho Chi Minh City, Vietnam
- KMID: 2532684
- DOI: http://doi.org/10.4166/kjg.2022.023
Abstract
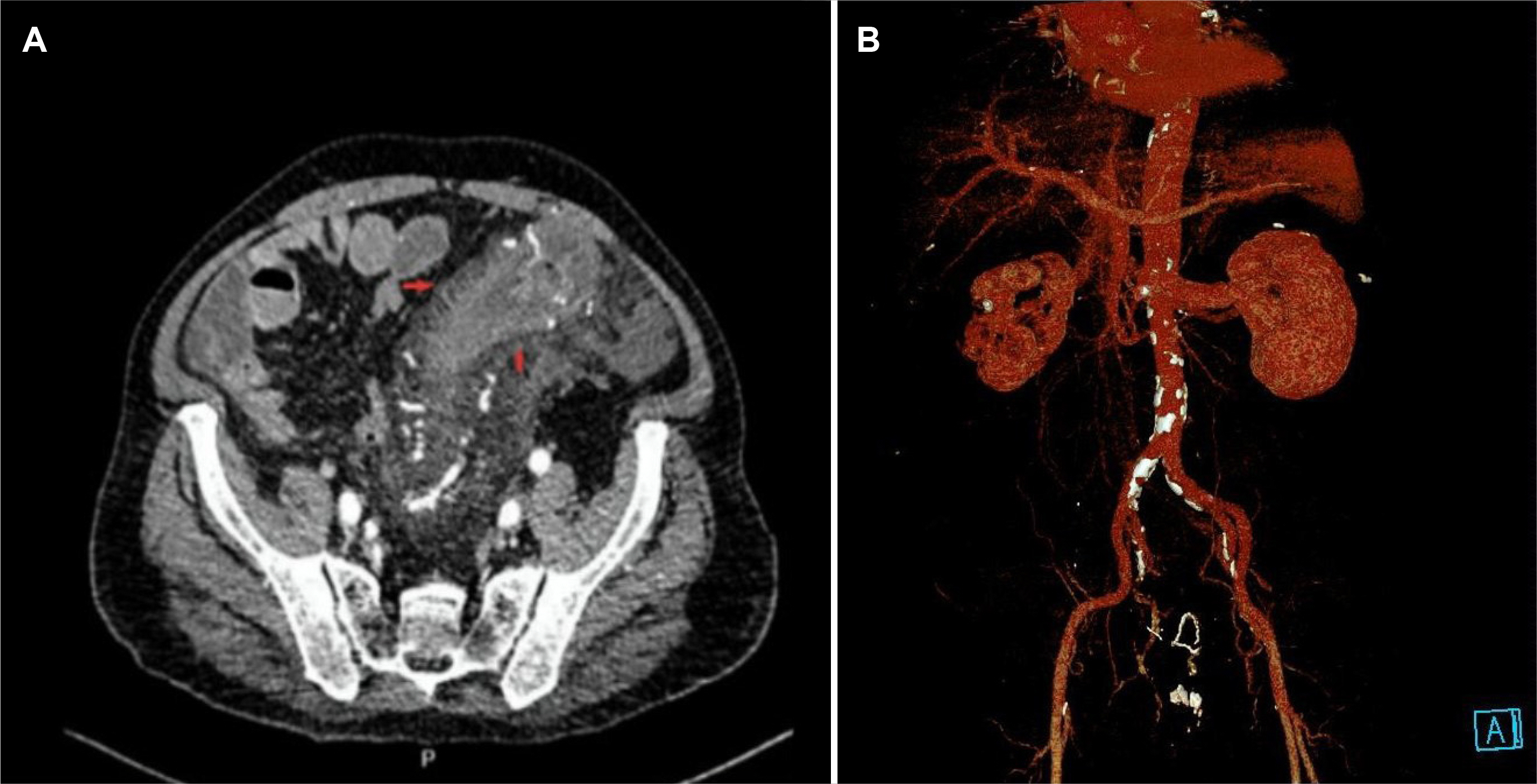
- Ischemic colitis (IC) is an underreported chronic disease characterized by the hypoperfusion of the bowel mucosa. The diagnosis and treatment may be challenging because its clinical course resembles other colitis or even colorectal malignancies. This paper reports an untypical case to underline the diversity of IC manifestation. A 68-year-old man with several comorbidities was admitted because of abdominal pain with a 6-month duration and a mass in the left lower quadrant. Colonoscopy revealed erosive pseudomembranous colitis narrowed colon segments with ulcerated mucosa mimicking colorectal cancer and inflammatory bowel disease. The stool cultures and Clostridium difficile toxin tests were negative. After the failure of conservative therapy, the Hartmann procedure with temporary ileostomy was performed uneventfully. The histological results of the surgical specimens revealed IC with focal pseudomembranous areas.
Keyword
Figure
Reference
-
1. Azam B, Kumar M, Mishra K, Dhibar DP. 2019; Ischemic colitis. J Emerg Med. 56:e85–e86. DOI: 10.1016/j.jemermed.2019.01.016. PMID: 30850260.2. Hung A, Calderbank T, Samaan MA, Plumb AA, Webster G. 2019; Ischaemic colitis: practical challenges and evidence-based recommendations for management. Frontline Gastroenterol. 12:44–52. DOI: 10.1136/flgastro-2019-101204. PMID: 33489068. PMCID: PMC7802492.3. Xu Y, Xiong L, Li Y, Jiang X, Xiong Z. 2021; Diagnostic methods and drug therapies in patients with ischemic colitis. Int J Colorectal Dis. 36:47–56. DOI: 10.1007/s00384-020-03739-z. PMID: 32936393. PMCID: PMC7493065.4. Khor TS, Lauwers GY, Odze RD, Srivastava A. 2015; "Mass-forming" variant of ischemic colitis is a distinct entity with predilection for the proximal colon. Am J Surg Pathol. 39:1275–1281. DOI: 10.1097/PAS.0000000000000438. PMID: 26034865.5. Killebrew SR, Patel NJ, Lam JP, Zhai Q, Lewis MD. 2020; It's not always cancer: ischemic colitis masquerading as a colonic mass. Gastrointest Endosc. 91:954–955. DOI: 10.1016/j.gie.2019.11.006. PMID: 31733198.6. Kim HS, Sauri F, Kang JH, Kim NK. 2020; Mass-forming ischemic colitis that mimics colon cancer. Chin Med J (Engl). 133:1253–1254. DOI: 10.1097/CM9.0000000000000800. PMID: 32433062. PMCID: PMC7249714.7. Farooq PD, Urrunaga NH, Tang DM, von Rosenvinge EC. 2015; Pseudomembranous colitis. Dis Mon. 61:181–206. DOI: 10.1016/j.disamonth.2015.01.006. PMID: 25769243. PMCID: PMC4402243.8. Tang DM, Urrunaga NH, De Groot H, von Rosenvinge EC, Xie G, Ghazi LJ. 2014; Pseudomembranous colitis: not always caused by Clostridium difficile. Case Rep Med. 2014:812704. DOI: 10.1155/2014/812704. PMID: 25214850. PMCID: PMC4151585.9. Brandt LJ, Feuerstadt P, Longstreth GF, Boley SJ. 2015; ACG clinical guideline: epidemiology, risk factors, patterns of presentation, diagnosis, and management of colon ischemia (CI). Am J Gastroenterol. 110:18–45. DOI: 10.1038/ajg.2014.395. PMID: 25559486.10. Montoro MA, Brandt LJ, Santolaria S, et al. 2011; Clinical patterns and outcomes of ischaemic colitis: results of the Working Group for the Study of Ischaemic Colitis in Spain (CIE study). Scand J Gastroenterol. 46:236–246. DOI: 10.3109/00365521.2010.525794. PMID: 20961178.11. Lorber J, Pessegueiro A. Ischemic colitis masquerading as pseudomembranous colitis. Proceedings of UCLA Healthcare. 2014; 18.12. Dignan CR, Greenson JK. 1997; Can ischemic colitis be differentiated from C difficile colitis in biopsy specimens? Am J Surg Pathol. 21:706–710. DOI: 10.1097/00000478-199706000-00011. PMID: 9199649.13. Danakas AM, Fazili BG, Huber AR. 2019; Mass-forming ischemic colitis: a potential mimicker of malignancy. Case Rep Pathol. 2019:8927872. DOI: 10.1155/2019/8927872. PMID: 31007961. PMCID: PMC6441522.14. Madureira AJ. 2004; The comb sign. Radiology. 230:783–784. DOI: 10.1148/radiol.2303020645. PMID: 14990842.15. Chen W, Zhu H, Chen H, et al. 2018; Phlebosclerotic colitis: our clinical experience of 25 patients in China. Medicine (Baltimore). 97:e12824. DOI: 10.1097/MD.0000000000012824. PMID: 30412073. PMCID: PMC6221691.16. Song SJ, Shroff SG. 2017; Idiopathic myointimal hyperplasia of mesenteric veins of the ileum and colon in a patient with crohn's disease: a case report and brief review of the literature. Case Rep Pathol. 2017:6793031. DOI: 10.1155/2017/6793031. PMID: 28894617. PMCID: PMC5574263.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of amebic colitis mimicking pseudomembranous colitis
- Ischemic colitis complicated by Clostridioides difficile infection treated with fecal microbiota transplantation
- Case of Pseudomembranous Colitis Caused by a Clostridioides difficile Infection Concomitant with Cytomegalovirus colitis Mimicking Ischemic Colitis
- Ischemic Pseudomembranous Colitis with Perforation due to Polyarteritis Nodosa
- A Case of Rifampicin Induced Pseudomembranous Colitis in Elderly Patient