Brain Tumor Res Treat.
2022 Jul;10(3):190-194. 10.14791/btrt.2022.0020.
A Huge Radiation-Induced Cavernous Hemangioma Following Stereotactic Radiosurgery for Meningioma: A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea
- KMID: 2532244
- DOI: http://doi.org/10.14791/btrt.2022.0020
Abstract
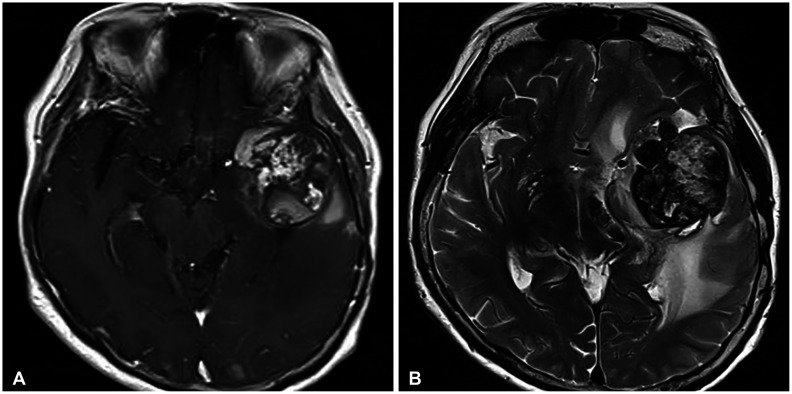
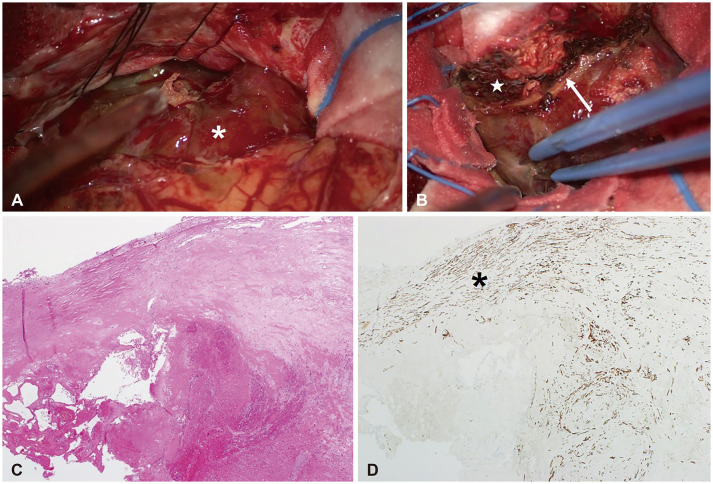
- Radiation-induced cavernous hemangiomas (RICHs) have been increasingly reported as a late complication after conventional radiotherapy. RICH after stereotactic radiosurgery (SRS) is extremely rare and the few cases have been reported to demonstrate their properties. A 72-year-old female patient presented with progressive neurologic deficits. She underwent tumor surgery for meningioma 13 years ago and two times of SRS for treating a residual tumor. Newly-developed mass was 4.3 cm-sized heterogeneously enhancing mass with severe cerebral edema. She underwent surgical resection and the histologic examinations revealed organized hematoma. Finally, it was diagnosed as a RICH following SRS based on radiological and histological findings and a history of multiple radiosurgeries. Clinical, radiological, and histological features of a RICH following SRS were discussed in this report.
Figure
Reference
-
1. Paddick I, Cameron A, Dimitriadis A. Extracranial dose and the risk of radiation-induced malignancy after intracranial stereotactic radiosurgery: is it time to establish a therapeutic reference level? Acta Neurochir (Wien). 2021; 163:971–979. PMID: 33325003.2. Nimjee SM, Powers CJ, Bulsara KR. Review of the literature on de novo formation of cavernous malformations of the central nervous system after radiation therapy. Neurosurg Focus. 2006; 21:e4.3. Cha YJ, Nahm JH, Ko JE, Shin HJ, Chang JH, Cho NH, et al. Pathological evaluation of radiation-induced vascular lesions of the brain: distinct from de novo cavernous hemangioma. Yonsei Med J. 2015; 56:1714–1720. PMID: 26446658.4. Cutsforth-Gregory JK, Lanzino G, Link MJ, Brown RD Jr, Flemming KD. Characterization of radiation-induced cavernous malformations and comparison with a nonradiation cavernous malformation cohort. J Neurosurg. 2015; 122:1214–1222. PMID: 25699412.5. Kleinschmidt-DeMasters BK, Lillehei KO. Radiation-induced cerebral vascular “malformations” at biopsy. J Neuropathol Exp Neurol. 2016; 75:1081–1092. PMID: 27694117.6. Koike T, Yanagimachi N, Ishiguro H, Yabe H, Yabe M, Morimoto T, et al. High incidence of radiation-induced cavernous hemangioma in long-term survivors who underwent hematopoietic stem cell transplantation with radiation therapy during childhood or adolescence. Biol Blood Marrow Transplant. 2012; 18:1090–1098. PMID: 22198541.7. Vinchon M, Leblond P, Caron S, Delestret I, Baroncini M, Coche B. Radiation-induced tumors in children irradiated for brain tumor: a longitudinal study. Childs Nerv Syst. 2011; 27:445–453. PMID: 21234575.8. Nagy G, McCutcheon BA, Giannini C, Link MJ, Pollock BE. Radiation-induced cavernous malformations after single-fraction meningioma radiosurgery. Oper Neurosurg (Hagerstown). 2018; 15:207–212. PMID: 29281070.9. Keezer MR, Del Maestro R. Radiation-induced cavernous hemangiomas: case report and literature review. Can J Neurol Sci. 2009; 36:303–310. PMID: 19534329.10. Heckl S, Aschoff A, Kunze S. Radiation-induced cavernous hemangiomas of the brain: a late effect predominantly in children. Cancer. 2002; 94:3285–3291. PMID: 12115362.11. Di Giannatale A, Morana G, Rossi A, Cama A, Bertoluzzo L, Barra S, et al. Natural history of cavernous malformations in children with brain tumors treated with radiotherapy and chemotherapy. J Neurooncol. 2014; 117:311–320. PMID: 24515423.12. Iwai Y, Yamanaka K, Yoshimura M. Intracerebral cavernous malformation induced by radiosurgery. Case report. Neurol Med Chir (Tokyo). 2007; 47:171–173. PMID: 17457021.13. Park YS, Kim SH, Chang JH, Chang JW, Park YG. Radiosurgery for radiosurgery-induced cavernous malformation. World Neurosurg. 2011; 75:94–98. PMID: 21492671.14. Sasagawa Y, Akai T, Itou S, Iizuka H. Gamma knife radiosurgery-induced cavernous hemangioma: case report. Neurosurgery. 2009; 64:E1006–E1007. PMID: 19404123.15. Wang X, Hui XH, Liu JP, Mao Q. Radiation-induced cavernous malformation at the site of arteriovenous malformation following gamma knife radiosurgery: case report. Clin Neurol Neurosurg. 2012; 114:1287–1289. PMID: 22456056.