Korean J Gastroenterol.
2022 Jul;80(1):6-16. 10.4166/kjg.2022.014.
Efficacy of a Restrictive Diet in Irritable Bowel Syndrome: A Systematic Review and Network Meta-analysis
- Affiliations
-
- 1Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Korea
- 2Department of Internal Medicine, Soonchunhyang University Hospital Bucheon, Bucheon, Korea
- 3Department of Internal Medicine, Chungnam National University College of Medicine, Daejeon, Korea
- 4Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea
- 5Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea
- 6Department of Internal Medicine, Dongguk University College of Medicine, Goyang, Korea
- 7Department of Internal Medicine, Konyang University Hospital, Daejeon, Korea
- 8Department of Internal Medicine, Dankook University Hospital, Cheonan, Korea
- 9Department of Public Health, Ajou University Graduate School of Public Health, Suwon, Korea
- 10Department of Orthopedic Surgery, Seoul Sacred Heart General Hospital, Seoul, Korea
- 11Inje University Medical Library, Busan, Korea
- KMID: 2532162
- DOI: http://doi.org/10.4166/kjg.2022.014
Abstract
- Background/Aims
Dietary factors can aggravate the symptoms of irritable bowel syndrome (IBS). Many IBS patients try restrictive diets to relieve their symptoms, but the types of diets with an exacerbating factor are unknown. Therefore, this paper reports the results of a systematic review and network meta-analysis of randomized-controlled trials (RCTs) reviewing the efficacy of food restriction diets in IBS.
Methods
The MEDLINE, EMBASE, Cochrane Central Register of Controlled Trials, and Clinicaltrials.gov databases were searched until July 21, 2021, to retrieve RCTs assessing the efficacy of restriction diets in adults with IBS. Two independent reviewers performed the eligibility assessment and data abstraction. RCTs that evaluated a restriction diet versus a control diet and assessed the improvement in global IBS symptoms were included. These trials reported a dichotomous assessment of the overall response to therapy.
Results
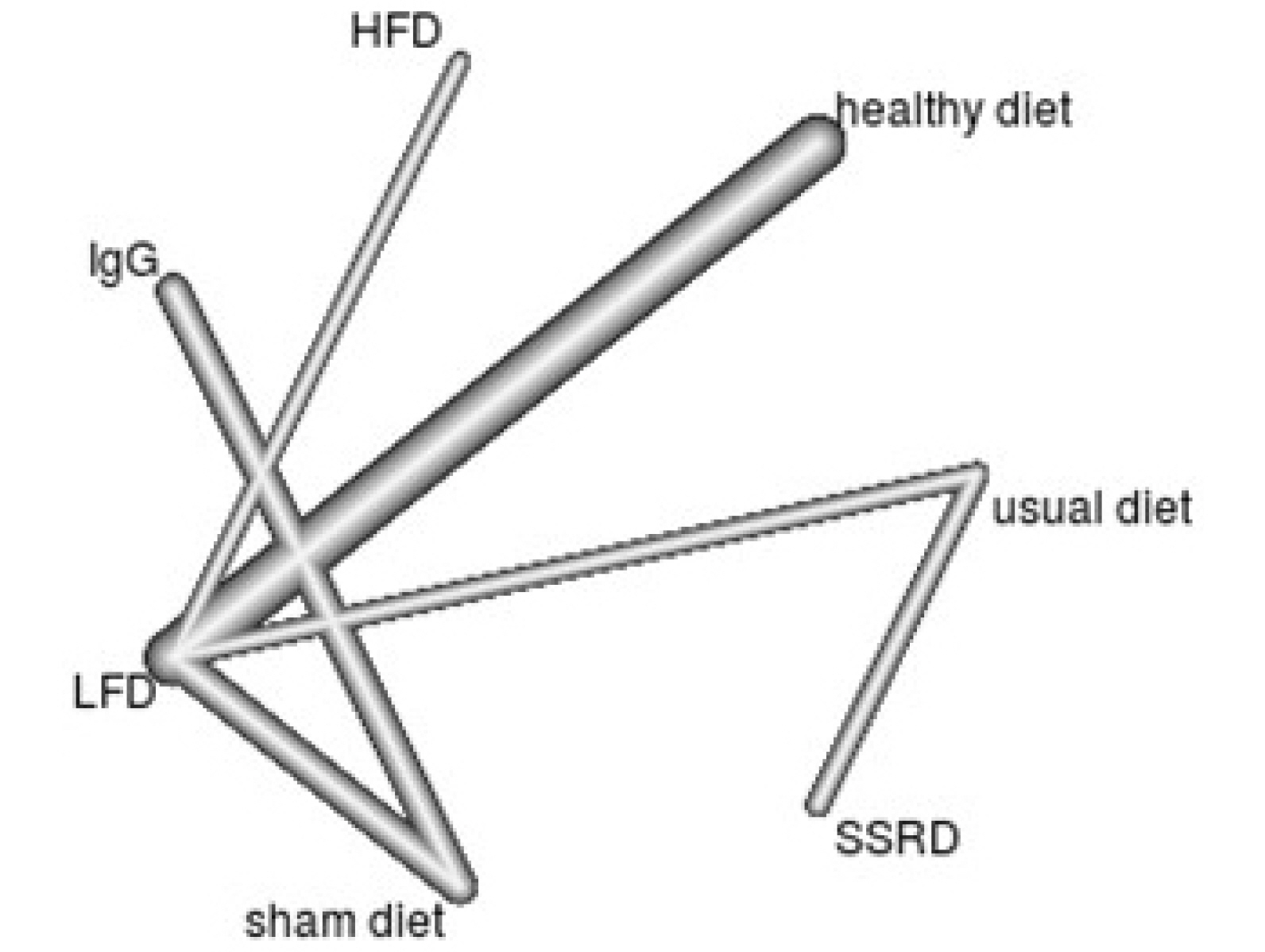
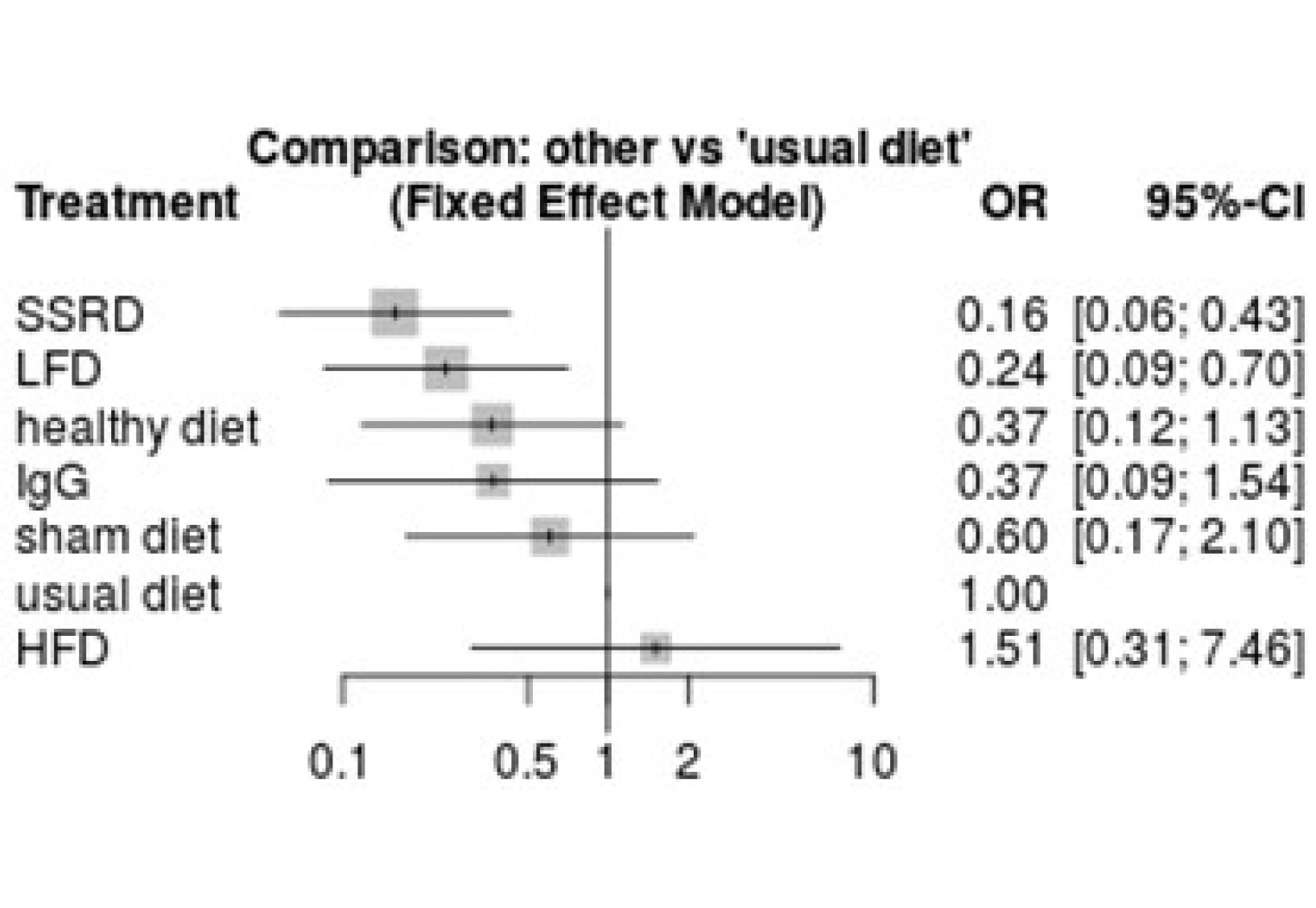
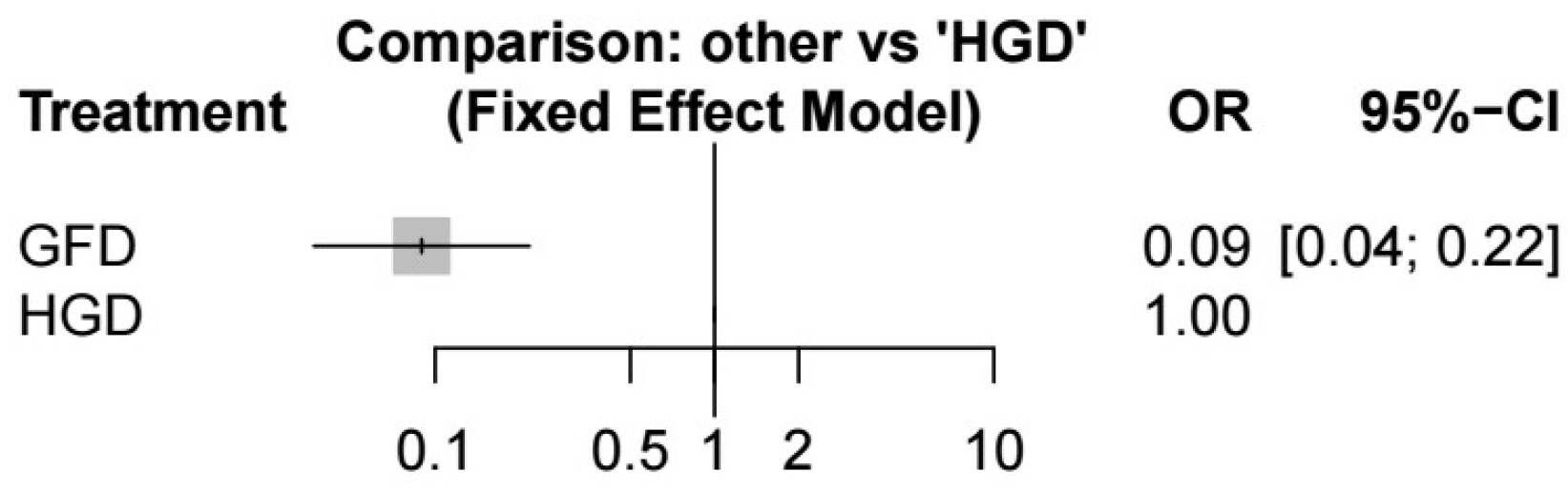
A total of 1,949 citations were identified. After full-text screening, 14 RCTs were considered eligible for the systematic review and network meta-analysis. A starch- and sucrose-reduced diet and a diet with low-fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) showed significantly better results than a usual diet. Symptom flare-ups in patients on a gluten-free diet were also significantly lower than in those on high-gluten diets.
Conclusions
These findings showed that the starch- and sucrose-reduced, low FODMAP, and gluten-free diets had superior effects in reducing IBS symptoms. Further studies, including head-to-head trials will be needed to establish the effectiveness of dietary restrictions on IBS symptoms.
Keyword
Figure
Reference
-
1. Lovell RM, Ford AC. 2012; Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 10:712–721.e4. DOI: 10.1016/j.cgh.2012.02.029. PMID: 22426087.2. Enck P, Aziz Q, Barbara G, et al. 2016; Irritable bowel syndrome. Nat Rev Dis Primers. 2:16014. DOI: 10.1038/nrdp.2016.14. PMID: 27159638. PMCID: PMC5001845.3. Patel NV. 2021; "Let Food Be Thy Medicine": Diet and supplements in irritable bowel syndrome. Clin Exp Gastroenterol. 14:377–384. DOI: 10.2147/CEG.S321054. PMID: 34588791. PMCID: PMC8473929.4. Simrén M, Månsson A, Langkilde AM, et al. 2001; Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. 63:108–115. DOI: 10.1159/000051878. PMID: 11244249.5. Ragnarsson G, Bodemar G. 1998; Pain is temporally related to eating but not to defaecation in the irritable bowel syndrome (IBS). Patients' description of diarrhea, constipation and symptom variation during a prospective 6-week study. Eur J Gastroenterol Hepatol. 10:415–421. DOI: 10.1097/00042737-199805000-00011. PMID: 9619389.6. Monsbakken KW, Vandvik PO, Farup PG. 2006; Perceived food intolerance in subjects with irritable bowel syndrome-- etiology, prevalence and consequences. Eur J Clin Nutr. 60:667–672. DOI: 10.1038/sj.ejcn.1602367. PMID: 16391571.7. Zhang Y, Feng L, Wang X, et al. 2021; Low fermentable oligosaccharides, disaccharides, monosaccharides, and polyols diet compared with traditional dietary advice for diarrhea-predominant irritable bowel syndrome: a parallel-group, randomized controlled trial with analysis of clinical and microbiological factors associated with patient outcomes. Am J Clin Nutr. 113:1531–1545. DOI: 10.1093/ajcn/nqab005. PMID: 33740048.8. Goyal O, Batta S, Nohria S, et al. 2021; Low fermentable oligosaccharide, disaccharide, monosaccharide, and polyol diet in patients with diarrhea-predominant irritable bowel syndrome: a prospective, randomized trial. J Gastroenterol Hepatol. 36:2107–2115. DOI: 10.1111/jgh.15410. PMID: 33464683.9. Böhn L, Störsrud S, Liljebo T, et al. 2015; Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: a randomized controlled trial. Gastroenterology. 149:1399–1407.e2. DOI: 10.1053/j.gastro.2015.07.054. PMID: 26255043.10. Moayyedi P, Quigley EM, Lacy BE, et al. 2015; The effect of dietary intervention on irritable bowel syndrome: a systematic review. Clin Transl Gastroenterol. 6:e107. DOI: 10.1038/ctg.2015.21. PMID: 26291435. PMCID: PMC4816279.11. Verdu EF, Armstrong D, Murray JA. 2009; Between celiac disease and irritable bowel syndrome: the "no man's land" of gluten sensitivity. Am J Gastroenterol. 104:1587–1594. DOI: 10.1038/ajg.2009.188. PMID: 19455131. PMCID: PMC3480312.12. Shahbazkhani B, Sadeghi A, Malekzadeh R, et al. 2015; Non-celiac gluten sensitivity has narrowed the spectrum of irritable bowel syndrome: a double-blind randomized placebo-controlled trial. Nutrients. 7:4542–4554. DOI: 10.3390/nu7064542. PMID: 26056920. PMCID: PMC4488801.13. Biesiekierski JR, Newnham ED, Irving PM, et al. 2011; Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. 106:508–515. DOI: 10.1038/ajg.2010.487. PMID: 21224837.14. Nilholm C, Roth B, Ohlsson B. 2019; A dietary intervention with reduction of starch and sucrose leads to reduced gastrointestinal and extra-intestinal symptoms in IBS patients. Nutrients. 11:1662. DOI: 10.3390/nu11071662. PMID: 31330810. PMCID: PMC6682926.15. Atkinson W, Sheldon TA, Shaath N, Whorwell PJ. 2004; Food elimination based on IgG antibodies in irritable bowel syndrome: a randomised controlled trial. Gut. 53:1459–1464. DOI: 10.1136/gut.2003.037697. PMID: 15361495. PMCID: PMC1774223.16. Hutton B, Salanti G, Caldwell DM, et al. 2015; The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 162:777–784. DOI: 10.7326/M14-2385. PMID: 26030634.17. Salanti G, Ades AE, Ioannidis JP. 2011; Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 64:163–171. DOI: 10.1016/j.jclinepi.2010.03.016. PMID: 20688472.18. Higgins JP, Thompson SG, Deeks JJ, Altman DG. 2003; Measuring inconsistency in meta-analyses. BMJ. 327:557–560. DOI: 10.1136/bmj.327.7414.557. PMID: 12958120. PMCID: PMC192859.19. Garcia-Etxebarria K, Zheng T, Bonfiglio F, et al. 2018; Increased prevalence of rare sucrase-isomaltase pathogenic variants in irritable bowel syndrome patients. Clin Gastroenterol Hepatol. 16:1673–1676. DOI: 10.1016/j.cgh.2018.01.047. PMID: 29408290. PMCID: PMC6103908.20. Nilholm C, Larsson E, Roth B, Gustafsson R, Ohlsson B. 2019; Irregular dietary habits with a high intake of cereals and sweets are associated with more severe gastrointestinal symptoms in IBS patients. Nutrients. 11:1279. DOI: 10.3390/nu11061279. PMID: 31195706. PMCID: PMC6627681.21. Staudacher HM, Whelan K. 2017; The low FODMAP diet: recent advances in understanding its mechanisms and efficacy in IBS. Gut. 66:1517–1527. DOI: 10.1136/gutjnl-2017-313750. PMID: 28592442.22. Ong DK, Mitchell SB, Barrett JS, et al. 2010; Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 25:1366–1373. DOI: 10.1111/j.1440-1746.2010.06370.x. PMID: 20659225.23. McIntosh K, Reed DE, Schneider T, et al. 2017; FODMAPs alter symptoms and the metabolome of patients with IBS: a randomised controlled trial. Gut. 66:1241–1251. DOI: 10.1136/gutjnl-2015-311339. PMID: 26976734.24. Irritable bowel syndrome in adults: diagnosis and management. [Internet]. London: National Institute for Health and Care Excellence (NICE);2008. Feb. 23. updated 2017 Apr 4; cited 2022 Apr 12. Available from: https://www.nice.org.uk/guidance/cg61.25. Black CJ, Staudacher HM, Ford AC. 2022; Efficacy of a low FODMAP diet in irritable bowel syndrome: systematic review and network meta-analysis. Gut. 71:1117–1126. DOI: 10.1136/gutjnl-2021-325214. PMID: 34376515.26. Rej A, Shaw CC, Buckle RL, et al. 2021; The low FODMAP diet for IBS; A multicentre UK study assessing long term follow up. Dig Liver Dis. 53:1404–1411. DOI: 10.1016/j.dld.2021.05.004. PMID: 34083153.27. Lacy BE, Pimentel M, Brenner DM, et al. 2021; ACG clinical guideline: management of irritable bowel syndrome. Am J Gastroenterol. 116:17–44. DOI: 10.14309/ajg.0000000000001036. PMID: 33315591.28. Sapone A, Bai JC, Ciacci C, et al. 2012; Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 10:13. DOI: 10.1186/1741-7015-10-13. PMID: 22313950. PMCID: PMC3292448.29. Bellini M, Tonarelli S, Mumolo MG, et al. 2020; Low fermentable oligodi-and mono-saccharides and polyols (FODMAPs) or gluten free diet: what is best for irritable bowel syndrome? Nutrients. 12:3368. DOI: 10.3390/nu12113368. PMID: 33139629. PMCID: PMC7692077.30. Paduano D, Cingolani A, Tanda E, Usai P. 2019; Effect of three diets (low-FODMAP, gluten-free and balanced) on irritable bowel syndrome symptoms and health-related quality of life. Nutrients. 11:1566. DOI: 10.3390/nu11071566. PMID: 31336747. PMCID: PMC6683324.31. Dionne J, Ford AC, Yuan Y, et al. 2018; A systematic review and meta-analysis evaluating the efficacy of a gluten-free diet and a low FODMAPs diet in treating symptoms of irritable bowel syndrome. Am J Gastroenterol. 113:1290–1300. DOI: 10.1038/s41395-018-0195-4. PMID: 30046155.32. De Giorgio R, Volta U, Gibson PR. 2016; Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction? Gut. 65:169–178. DOI: 10.1136/gutjnl-2015-309757. PMID: 26078292.33. Guo H, Jiang T, Wang J, Chang Y, Guo H, Zhang W. 2012; The value of eliminating foods according to food-specific immunoglobulin G antibodies in irritable bowel syndrome with diarrhoea. J Int Med Res. 40:204–210. DOI: 10.1177/147323001204000121. PMID: 22429360.34. Aydinlar EI, Dikmen PY, Tiftikci A, et al. 2013; IgG-based elimination diet in migraine plus irritable bowel syndrome. Headache. 53:514–525. DOI: 10.1111/j.1526-4610.2012.02296.x. PMID: 23216231.35. McKenzie YA, Alder A, Anderson W, et al. 2012; British Dietetic Association evidence-based guidelines for the dietary management of irritable bowel syndrome in adults. J Hum Nutr Diet. 25:260–274. DOI: 10.1111/j.1365-277X.2012.01242.x. PMID: 22489905.36. Dalrymple J, Bullock I. 2008; Diagnosis and management of irritable bowel syndrome in adults in primary care: summary of NICE guidance. BMJ. 336:556–558. DOI: 10.1136/bmj.39484.712616.AD. PMID: 18325967. PMCID: PMC2265348.37. Moayyedi P, Simrén M, Bercik P. 2020; Evidence-based and mechanistic insights into exclusion diets for IBS. Nat Rev Gastroenterol Hepatol. 17:406–413. DOI: 10.1038/s41575-020-0270-3. PMID: 32123377.38. Wilson B, Rossi M, Kanno T, et al. 2020; β-galactooligosaccharide in conjunction with low FODMAP diet improves irritable bowel syndrome symptoms but reduces fecal bifidobacteria. Am J Gastroenterol. 115:906–915. DOI: 10.14309/ajg.0000000000000641. PMID: 32433273.39. Hustoft TN, Hausken T, Ystad SO, et al. 2017; Effects of varying dietary content of fermentable short-chain carbohydrates on symptoms, fecal microenvironment, and cytokine profiles in patients with irritable bowel syndrome. Neurogastroenterol Motil. 29:e12969. DOI: 10.1111/nmo.12969. PMID: 27747984.40. Staudacher HM, Lomer MCE, Farquharson FM, et al. 2017; A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: a randomized controlled trial. Gastroenterology. 153:936–947. DOI: 10.1053/j.gastro.2017.06.010. PMID: 28625832.41. Eswaran SL, Chey WD, Han-Markey T, Ball S, Jackson K. 2016; A randomized controlled trial comparing the low FODMAP diet vs. modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol. 111:1824–1832. DOI: 10.1038/ajg.2016.434. PMID: 27725652.42. Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. 2014; A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 146:67–75.e5. DOI: 10.1053/j.gastro.2014.01.071. PMID: 24076059.43. Staudacher HM, Lomer MC, Anderson JL, et al. 2012; Fermentable carbohydrate restriction reduces luminal bifidobacteria and gastrointestinal symptoms in patients with irritable bowel syndrome. J Nutr. 142:1510–1518. DOI: 10.3945/jn.112.159285. PMID: 22739368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Amitriptyline in Irritable Bowel Syndrome: A Systematic Review and Meta-analysis
- The Efficacy of Hypnotherapy in the Treatment of Irritable Bowel Syndrome: A Systematic Review and Meta-analysis
- Can Low FODMAP Diet Be Considered as First-line Therapy in the Management of Irritable Bowel Syndrome?
- Irritable bowel syndrome
- Can a Diet Low in Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols (FODMAPs) Reduce the Symptoms of Irritable Bowel Syndrome?