Intest Res.
2022 Jul;20(3):313-320. 10.5217/ir.2020.00158.
Risk factors for non-reaching of ileal pouch to the anus in laparoscopic restorative proctocolectomy with handsewn anastomosis for ulcerative colitis
- Affiliations
-
- 1Department of Surgical Oncology, The University of Tokyo, Tokyo, Japan
- KMID: 2531985
- DOI: http://doi.org/10.5217/ir.2020.00158
Abstract
- Background/Aims
Restorative proctocolectomy (RPC) with ileal pouch-anal anastomosis and handsewn anastomosis for ulcerative colitis requires pulling down of the ileal pouch into the pelvis, which can be technically challenging. We examined risk factors for the pouch not reaching the anus.
Methods
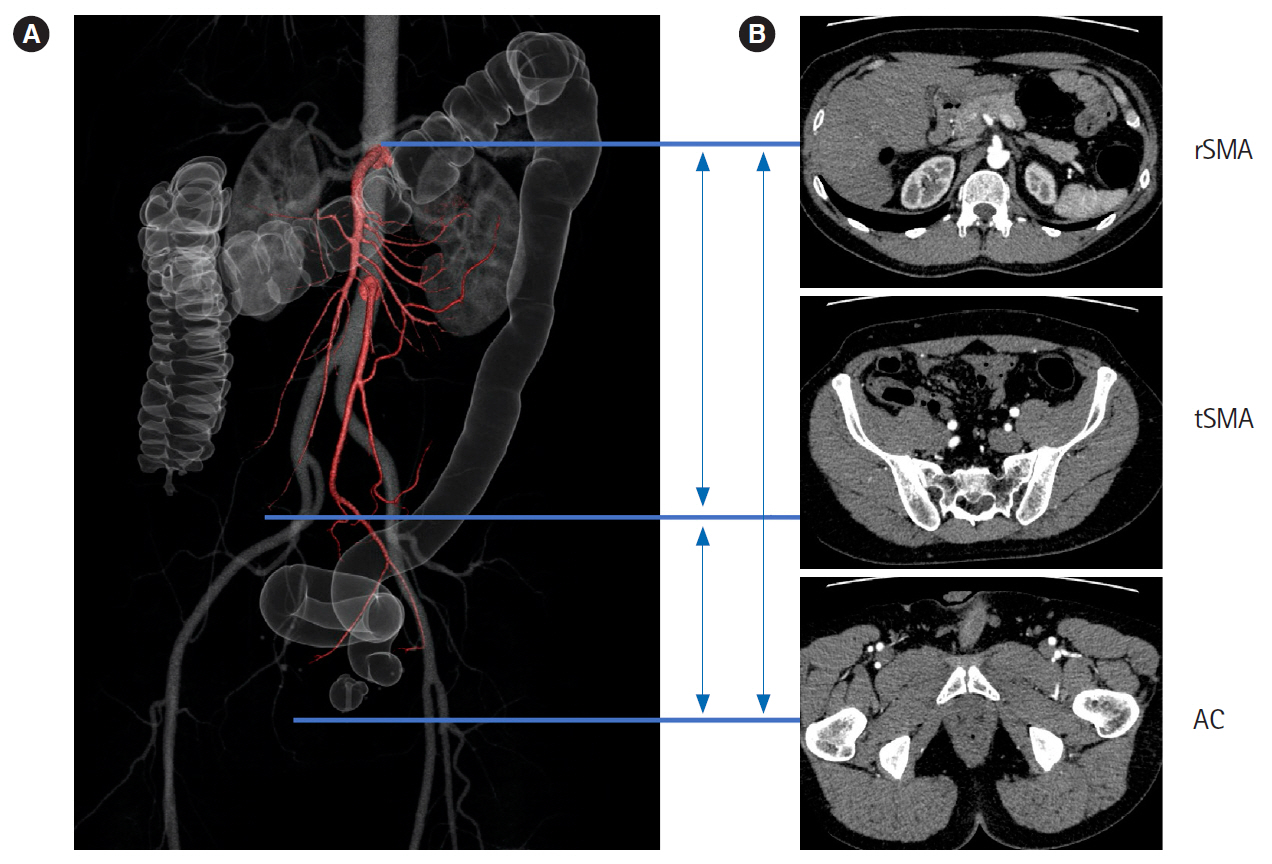
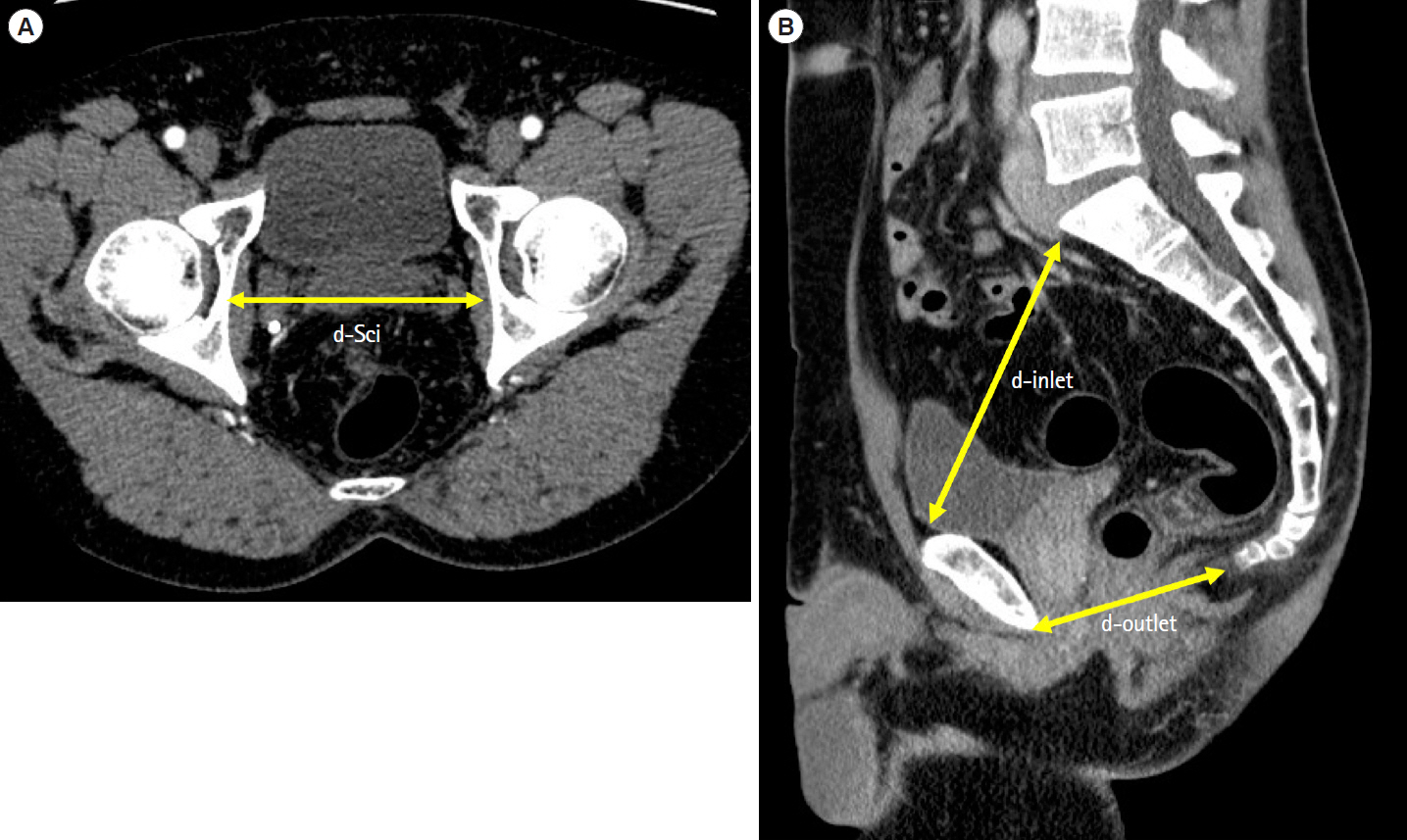
Clinical records of 62 consecutive patients who were scheduled to undergo RPC with handsewn anastomosis at the University of Tokyo Hospital during 1989–2019 were reviewed. Risk factors for non-reaching were analyzed in patients in whom hand sewing was abandoned for stapled anastomosis because of nonreaching. Risk factors for non-reaching in laparoscopic RPC were separately analyzed. Anatomical indicators obtained from presurgical computed tomography (CT) were also evaluated.
Results
Thirty-seven of 62 cases underwent laparoscopic procedures. In 6 cases (9.7%), handsewn anastomosis was changed to stapled anastomosis because of non-reaching. Male sex and a laparoscopic approach were independent risk factors of non-reaching. Distance between the terminal of the superior mesenteric artery (SMA) ileal branch and the anus > 11 cm was a risk factor for non-reaching.
Conclusions
Laparoscopic RPC with handsewn anastomosis may limit extension and induction of the ileal pouch into the anus. Preoperative CT measurement from the terminal SMA to the anus may be useful for predicting non-reaching.
Figure
Reference
-
1. Parks AG, Nicholls RJ. Proctocolectomy without ileostomy for ulcerative colitis. Br Med J. 1978; 2:85–88.
Article2. Heald RJ, Allen DR. Stapled ileo-anal anastomosis: a technique to avoid mucosal proctectomy in the ileal pouch operation. Br J Surg. 1986; 73:571–572.
Article3. Derikx LA, Kievit W, Drenth JP, et al. Prior colorectal neoplasia is associated with increased risk of ileoanal pouch neoplasia in patients with inflammatory bowel disease. Gastroenterology. 2014; 146:119–128.
Article4. Nobel T, Khaitov S, Greenstein AJ. Controversies in J pouch surgery for ulcerative colitis: a focus on handsewn versus stapled anastomosis. Inflamm Bowel Dis. 2016; 22:2302–2309.5. Browning SM, Nivatvongs S. Intraoperative abandonment of ileal pouch to anal anastomosis: the Mayo Clinic experience. J Am Coll Surg. 1998; 186:441–445.6. Smith L, Friend WG, Medwell SJ. The superior mesenteric artery: the critical factor in the pouch pull-through procedure. Dis Colon Rectum. 1984; 27:741–744.7. Cherqui D, Valleur P, Perniceni T, Hautefeuille P. Inferior reach of ileal reservoir in ileoanal anastomosis: experimental anatomic and angiographic study. Dis Colon Rectum. 1987; 30:365–371.8. Burnstein MJ, Schoetz DJ Jr, Coller JA, Veidenheimer MC. Technique of mesenteric lengthening in ileal reservoir-anal anastomosis. Dis Colon Rectum. 1987; 30:863–866.
Article9. Thirlby RC. Optimizing results and techniques of mesenteric lengthening in ileal pouch-anal anastomosis. Am J Surg. 1995; 169:499–502.
Article10. Goes RN, Nguyen P, Huang D, Beart RW Jr. Lengthening of the mesentery using the marginal vascular arcade of the right colon as the blood supply to the ileal pouch. Dis Colon Rectum. 1995; 38:893–895.
Article11. Martel P, Majery N, Savigny B, Sezeur A, Gallot D, Malafosse M. Mesenteric lengthening in ileoanal pouch anastomosis for ulcerative colitis: is high division of the superior mesenteric pedicle a safe procedure? Dis Colon Rectum. 1998; 41:862–866.
Article12. Martel P, Blanc P, Bothereau H, Malafosse M, Gallot D. Comparative anatomical study of division of the ileocolic pedicle or the superior mesenteric pedicle for mesenteric lengthening. Br J Surg. 2002; 89:775–778.
Article13. Araki T, Parc Y, Lefevre J, Dehni N, Tiret E, Parc R. The effect on morbidity of mesentery lengthening techniques and the use of a covering stoma after ileoanal pouch surgery. Dis Colon Rectum. 2006; 49:621–628.
Article14. Baig MK, Weiss EG, Nogueras JJ, Wexner SD. Lengthening of small bowel mesentery: stepladder incision technique. Am J Surg. 2006; 191:715–717.
Article15. Uraiqat AA, Byrne CM, Phillips RK. Gaining length in ileal-anal pouch reconstruction: a review. Colorectal Dis. 2007; 9:657–661.
Article16. İsmail E, Açar Hİ, Arslan MN, et al. Comparison of mesenteric lengthening techniques in IPAA: an anatomic and angiographic study on fresh cadavers. Dis Colon Rectum. 2018; 61:979–987.
Article17. Ohira G, Miyauchi H, Narushima K, et al. Predicting difficulty in extending the ileal pouch to the anus in restorative proctocolectomy: investigation of a simple predictive method using computed tomography. Colorectal Dis. 2017; 19:O34–O38.
Article18. Polle SW, van Berge Henegouwen MI, Slors JF, Cuesta MA, Gouma DJ, Bemelman WA. Total laparoscopic restorative proctocolectomy: are there advantages compared with the open and hand-assisted approaches? Dis Colon Rectum. 2008; 51:541–548.
Article19. Hemandas AK, Jenkins JT. Laparoscopic pouch surgery in ulcerative colitis. Ann Gastroenterol. 2012; 25:309–316.20. Hata K, Kazama S, Nozawa H, et al. Laparoscopic surgery for ulcerative colitis: a review of the literature. Surg Today. 2015; 45:933–938.
Article21. Baek SJ, Lightner AL, Boostrom SY, et al. Functional outcomes following laparoscopic ileal pouch-anal anastomosis in patients with chronic ulcerative colitis: long-term follow-up of a case-matched study. J Gastrointest Surg. 2017; 21:1304–1308.
Article22. Utsunomiya J, Yamamura T, Kusonoki M, Iwama T. The current technique of ileoanal anastomosis. Dig Surg. 1988; 5:207–214.
Article23. Ikeuchi H, Uchino M, Matsuoka H, et al. Surgery for ulcerative colitis in 1,000 patients. Int J Colorectal Dis. 2010; 25:959–965.
Article24. Akiyoshi T, Kuroyanagi H, Oya M, et al. Factors affecting the difficulty of laparoscopic total mesorectal excision with double stapling technique anastomosis for low rectal cancer. Surgery. 2009; 146:483–489.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Functional Outcome after Ileal J-pouch Anal Anastomosis in Patients with Ulcerative Colitis
- Carcinoma in an Ileal Pouch after Proctocolectomy, with Ileal Pouch-Anal
- Operative Outcomes of Open versus Laparoscopic Total Proctocolectomy with Ileal Pouch Anal Anastomosis in Ulcerative Colitis
- Adenocarcinoma in Ileal Pouch after Proctocolectomy for Familial Adenomatous Polyposis: Report of A Case
- The Clinical Results of a Total Proctocolectomy with an Ileal Pouch-Anal Anastomosis: 12 Cases