Anesth Pain Med.
2022 Apr;17(2):239-244. 10.17085/apm.21102.
Management of pulmonary aspiration due to undiagnosed achalasia during induction of general anesthesia - A case report -
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Severance Hospital and Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2531702
- DOI: http://doi.org/10.17085/apm.21102
Abstract
- Background
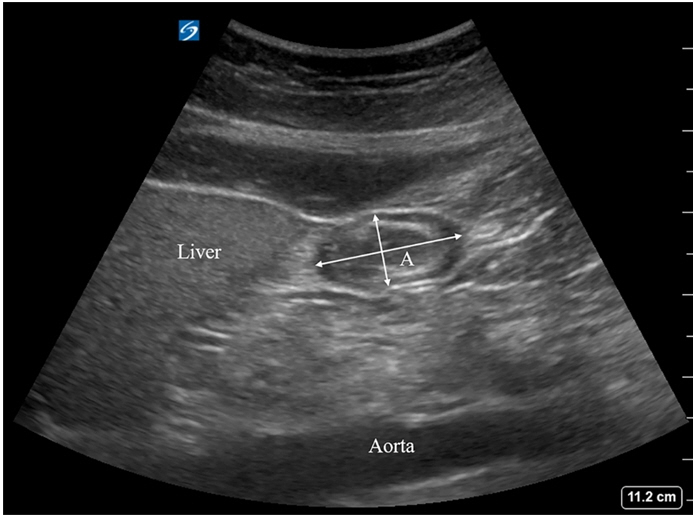
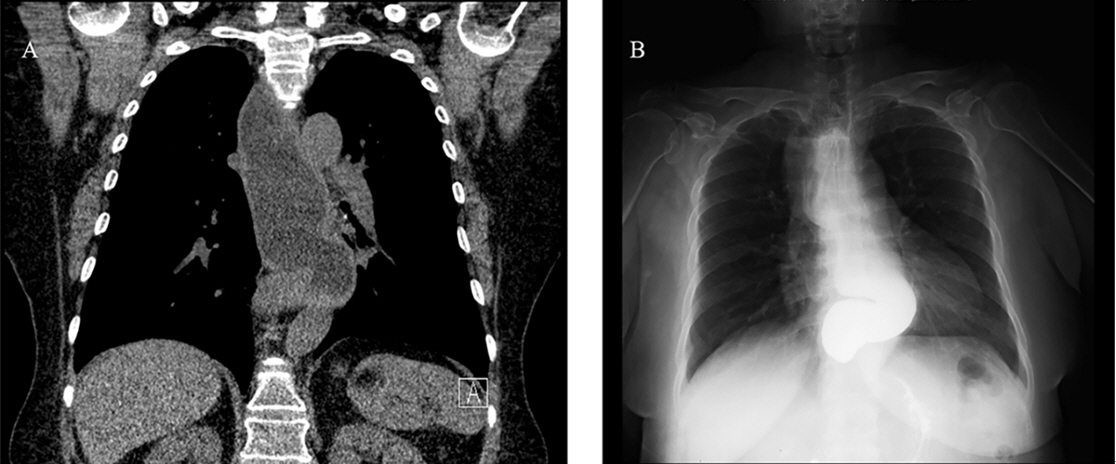
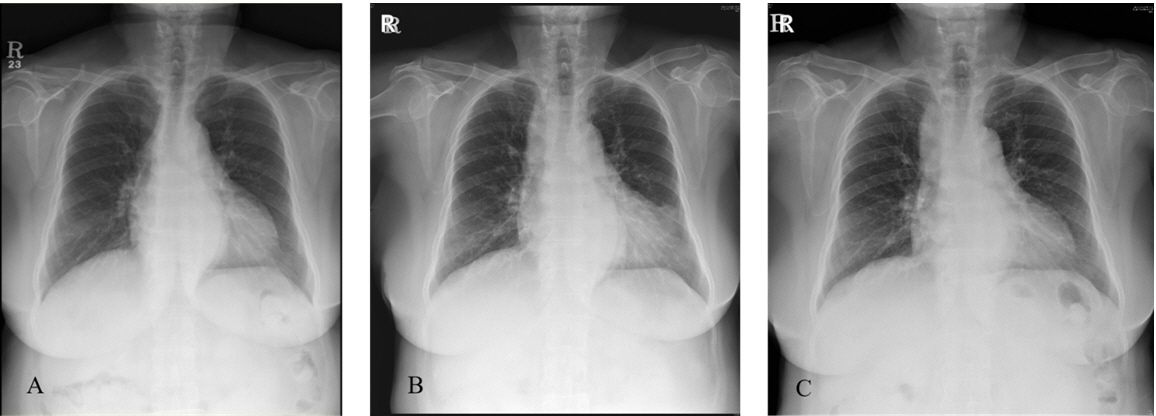
Intraoperative pulmonary aspiration is a rare but potentially fatal complication associated with various risk factors. Preoperative recognition of these risk factors can prevent aspiration events during general anesthesia or facilitate prompt corrective measures in patients experiencing this complication. Case: A 70-year-old female patient with hypertension underwent bilateral total knee arthroplasty under general anesthesia. Despite using a midnight nothing-per-oral (NPO) protocol, an unpredictable intraoperative aspiration event occurred during anesthesia induction. A detailed evaluation of the patient’s medical history and subsequent diagnostic imaging examinations indicated achalasia. She was treated for aspiration pneumonia for 2 weeks. After 2 months, rescheduled total knee arthroplasty was performed under spinal anesthesia without any complications.
Conclusions
Obtaining the patient’s medical history and assessing the risk factors are important to prevent unpredictable intraoperative pulmonary aspiration. High-risk patients should undergo adequate preoperative fasting and regional anesthesia or rapid-sequence intubation should be considered for safe induction of general anesthesia.
Figure
Reference
-
1. Nason KS. Acute intraoperative pulmonary aspiration. Thorac Surg Clin. 2015; 25:301–7.
Article2. Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 2020; 115:1393–411.
Article3. Van de Putte P, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014; 113:12–22.
Article4. Kim E, Lee H, Jung HK, Lee KJ. Achalasia in Korea: an epidemiologic study using a national healthcare database. J Korean Med Sci. 2014; 29:576–80.
Article5. Jung HK, Hong SJ, Lee OY, Pandolfino J, Park H, Miwa H, et al. Korean Society of Neurogastroenterology and Motility. 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 2020; 26:180–203.
Article6. Taft TH, Carlson DA, Triggs J, Craft J, Starkey K, Yadlapati R, et al. Evaluating the reliability and construct validity of the Eckardt symptom score as a measure of achalasia severity. Neurogastroenterol Motil. 2018; 30:e13287.
Article7. Löser B, Recio Ariza O, Saugel B, Reuter DA, Zöllner C, Werner YB, et al. Anesthesia for patients undergoing peroral endoscopic myotomy procedures: a review of the literature. Anesth Analg. 2020; 130:1331–40.8. Kluger MT, Visvanathan T, Myburgh JA, Westhorpe RN. Crisis management during anaesthesia: regurgitation, vomiting, and aspiration. Qual Saf Health Care. 2005; 14:e4.
Article9. Butler J, Sen A. Towards evidence-based emergency medicine: best BETs from the Manchester Royal Infirmary. BET 1: cricoid pressure in emergency rapid sequence induction. Emerg Med J. 2013; 30:163–5.10. Creagh-Barry P, Parsons J, Pattison CW. Achalasia and anaesthesia, a case report. Anaesth Intensive Care. 1988; 16:371–3.
Article11. Choi JW, Lee JH, Kim EJ, Lee SG, Ban JS, Min BW. Aspiration pneumonitis in achalasia patient treated by per oral endoscopic myotomy: a case report. Anesth Pain Med. 2012; 7:151–4.12. Takenaka I, Aoyama K, Iwagaki T. Combining head-neck position and head-down tilt to prevent pulmonary aspiration of gastric contents during induction of anaesthesia: a volunteer and manikin study. Eur J Anaesthesiol. 2012; 29:380–5.13. Higgs A, McGrath BA, Goddard C, Rangasami J, Suntharalingam G, Gale R, et al. Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018; 120:323–52.14. Kruisselbrink R, Gharapetian A, Chaparro LE, Ami N, Richler D, Chan VWS, et al. Diagnostic accuracy of point-of-care gastric ultrasound. Anesth Analg. 2019; 128:89–95.
Article15. Haskins SC, Kruisselbrink R, Boublik J, Wu CL, Perlas A. Gastric ultrasound for the regional anesthesiologist and pain specialist. Reg Anesth Pain Med. 2018; 43:689–98.
Article16. Fawcett WJ, Thomas M. Pre-operative fasting in adults and children: clinical practice and guidelines. Anaesthesia. 2019; 74:83–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspiration Pneumonia in Esophageal Achalasia Patient during Anesthesia for Cesarian Section
- Aspiration pneumonitis in achalasia patient treated by per oral endoscopic myotomy: A case report
- Pulmonary thromboembolism occurred immediately after leg elevation under induction of general anesthesia in a patient with femur fracture : A case report
- Pulmonary aspiration during intubation in a high-risk patient: A video clip and clinical implications
- Effectiveness of milrinone for cardiogenic shock due to massive pulmonary aspiration: a case report