J Dent Anesth Pain Med.
2018 Apr;18(2):111-114. 10.17245/jdapm.2018.18.2.111.
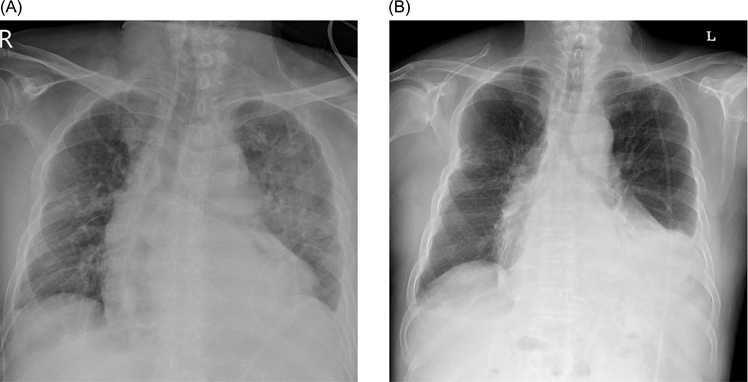
Pulmonary aspiration during intubation in a high-risk patient: A video clip and clinical implications
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Republic of Korea. shkimans@amc.seoul.kr
- KMID: 2410144
- DOI: http://doi.org/10.17245/jdapm.2018.18.2.111
Abstract
- We report a case of pulmonary aspiration during induction of general anesthesia in a patient who was status post esophagectomy. Sudden, unexpected aspiration occurred even though the patient had fasted adequately (over 13 hours) and received rapid sequence anesthesia induction. Since during esophagectomy, the lower esophageal sphincter is excised, stomach vagal innervation is lost, and the stomach is flaccid, draining only by gravity, the patient becomes vulnerable to aspiration. As the incidence of perioperative pulmonary aspiration is relatively low, precautions to prevent aspiration tend to be overlooked. We present a video clip showing pulmonary aspiration and discuss the literature concerning the risk of aspiration and its preventive strategies.
MeSH Terms
Figure
Cited by 1 articles
-
Analysis of the effect of oral midazolam and triazolam premedication before general anesthesia in patients with disabilities with difficulty in cooperation
Seon Woo Lim, Eunsun So, Hye Joo Yun, Myong-Hwan Karm, Juhea Chang, Hanbin Lee, Hyun Jeong Kim, Kwang-Suk Seo
J Dent Anesth Pain Med. 2018;18(4):245-254. doi: 10.17245/jdapm.2018.18.4.245.
Reference
-
1. Borsari TE, Hilmi IA, Sakai T. Perioperative pulmonary aspiration of patients who have had an esophagectomy with a gastric pull-up: the value of preoperative computed tomography of the neck. J Clin Anesth. 2011; 23:130–133.
Article2. Jankovic ZB, Milosavljevic S, Stamenkovic D, Stojakov D, Sabljak P, Pesko P. High risk of aspiration and difficult intubation in post-esophagectomy patients. Acta Anaesthesiol Scand. 2000; 44:899–900.
Article3. Black DR, Thangathurai D, Senthilkumar N, Roffey P, Mikhail M. High risk of aspiration and difficult intubation in post-esophagectomy patients. Acta Anaesthesiol Scand. 1999; 43:687.4. Son YG, Shin J, Ryu HG. Pneumonitis and pneumonia after aspiration. J Dent Anesth Pain Med. 2017; 17:1–12.
Article5. Sakai T, Planinsic RM, Quinlan JJ, Handley LJ, Kim TY, Hilmi IA. The incidence and outcome of perioperative pulmonary aspiration in a university hospital: a 4-year retrospective analysis. Anesth Analg. 2006; 103:941–947.
Article6. Neelakanta G, Chikyarappa A. A review of patients with pulmonary aspiration of gastric contents during anesthesia reported to the Departmental Quality Assurance Committee. J Clin Anesth. 2006; 18:102–107.
Article7. Warner MA, Warner ME, Weber JG. Clinical significance of pulmonary aspiration during the perioperative period. Anesthesiology. 1993; 78:56–62.
Article8. de Souza DG, Gaughen CL. Aspiration risk after esophagectomy. Anesth Analg. 2009; 109:1352.
Article9. Lim HK, Lee MH, Jin CI, Byeon HJ, Song JH. Pulmonary aspiration occurring during the induction of anesthesia in a patient with esophageal dilatation. Korean J Anesthesiol. 2013; 64:474–475.
Article10. Neilipovitz DT, Crosby ET. No evidence for decreased incidence of aspiration after rapid sequence induction. Can J Anaesth. 2007; 54:748–764.
Article11. Brimacombe JR, Berry AM. Cricoid pressure. Can J Anaesth. 1997; 44:414–425.
Article12. Smith KJ, Dobranowski J, Yip G, Dauphin A, Choi PT. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003; 99:60–64.
Article13. Muravchick S, Burkett L, Gold MI. Succinylcholine-induce fasciculations and intragastric pressure during induction of anesthesia. Anesthesiology. 1981; 55:180–183.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Aspiration Pneumonia after General Anesthesia Using Laryngeal Mask Airway: A case report
- Management of pulmonary aspiration due to undiagnosed achalasia during induction of general anesthesia - A case report -
- Fiberoptic Bronchoscopic Treatment of Pulmonary Aspiration Occurring in a Child during Induction of Anesthesia: A case report
- The utilization of video laryngoscopy in nasotracheal intubation for oral and maxillofacial surgical procedures: a narrative review
- Development of Educational Contents for Therapeutic Communication based on Video Clip