Pediatr Emerg Med J.
2022 Jun;9(1):10-16. 10.22470/pemj.2021.00381.
Effect of coronavirus disease 2019 pandemic on children’s visits to the emergency department
- Affiliations
-
- 1Department of Emergency Medicine, Hallym University Sacred Heart Hospital, Hallym University Medical Center, Republic of Korea
- 2Department of Neurology, Hallym University Sacred Heart Hospital, Hallym University Medical Center, Republic of Korea
- KMID: 2531523
- DOI: http://doi.org/10.22470/pemj.2021.00381
Abstract
- Purpose
In the coronavirus disease 2019 pandemic, it is essential to supplement the changes in visiting patterns of individual emergency departments (EDs) to determine how to allocate emergency medicine resources. We compared the clinical features of children visiting the ED before and during the pandemic.
Methods
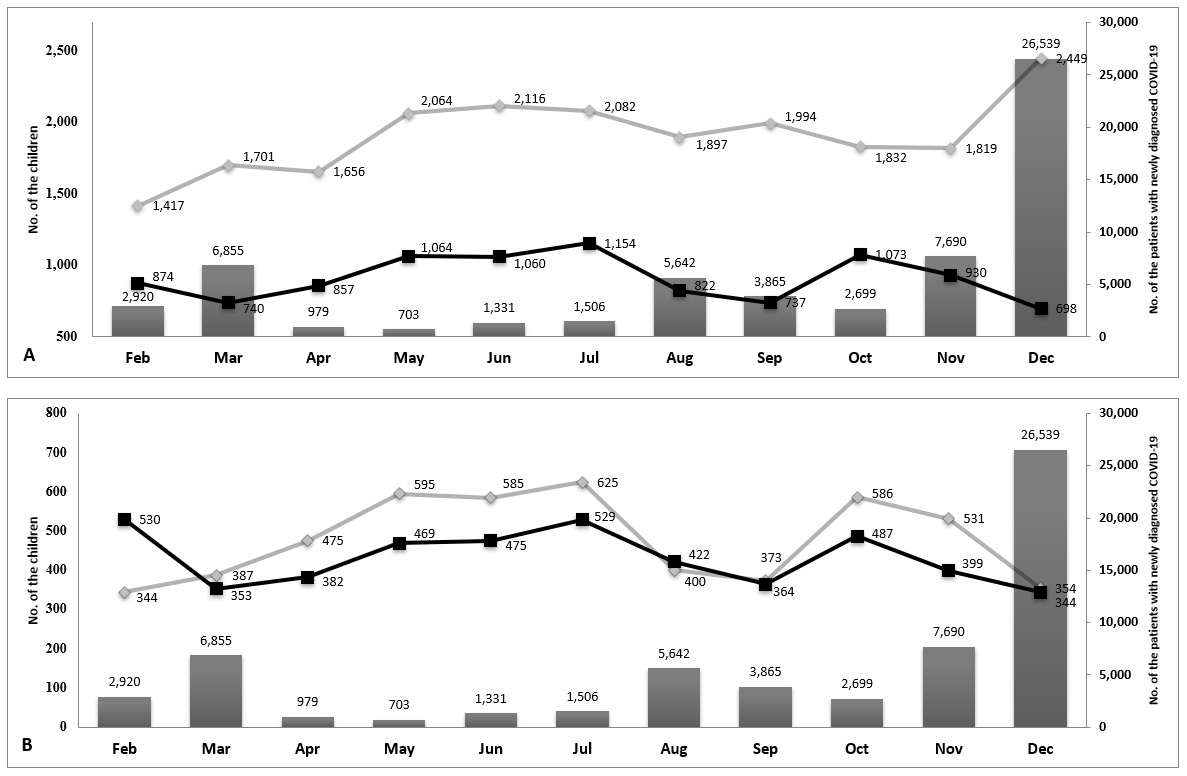
Children younger than 18 years who visited the ED from February 2019 through December 2020, except January 2020, were enrolled, and divided into those who visited before and after January 2020 (the pre-pandemic and pandemic groups, respectively). We compared the 2 groups in terms of the baseline characteristics (age, sex, mode and route of arrival, cause of visit, and time of visit), chief complaint, ED diagnosis, initial acuity and its accuracy, and ED outcomes (length of stay and disposition).
Results
The 31,036 children were categorized into the pre-pandemic (21,027 [67.8%]) and pandemic (10,009 [32.2%]) groups with a 52.4% decrease in the number of visits to the ED in the latter group. This decrease was more prominent in age 2-5 years (from 37.3% to 33.2%; P < 0.001), fever as a chief complaint (from 27.8% to 16.5%), diagnoses related to infection or the respiratory system (from 36.8% to 14.3%) or transfer to the ED (from 8.1% to 6.4%; P < 0.001). In contrast, increases were noted in age 12-17 years (from 14.9% to 17.4%; P < 0.001), injury (from 36.5% to 52.5%; P < 0.001), visits in the evening (from 54.9% to 57.4%; P < 0.001), length of stay longer than 6 hours (from 3.5% to 6.3%; P = 0.033), and low acuity (from 97.8% to 98.2%; P = 0.031).
Conclusion
The pandemic has brought about changes in visiting patterns of the ED. This study may help prepare strategies for the appropriate allocation and deployment of emergency medicine resources in the pandemic era.
Keyword
Figure
Cited by 2 articles
-
Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
Dae Ho Kang
Pediatr Emerg Med J. 2022;9(1):29-34. doi: 10.22470/pemj.2022.00451.Changes in emergency department utilization by neonates during the coronavirus disease 2019 pandemic: a single-center study in Korea
Sung Hee Lee, Shin Won Yoon, Ju Hyun Jin
Pediatr Emerg Med J. 2024;11(3):107-114. doi: 10.22470/pemj.2024.00976.
Reference
-
References
1. Kim AJ, Son MH, Park M. Effect of coronavirus disease 2019 on febrile children’s visits to the emergency department of a tertiary hospital. Pediatr Emerg Med J. 2021; 8:8–15.
Article2. Hwang SY, Lee JK, Ryu HS, Park SS, Choi JY, Lee HJ, et al. Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea. Pediatr Emerg Med J. 2021; 8:57–65. Korean.
Article3. Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul metropolitan area, Korea. J Korean Med Sci. 2021; 36:e44.
Article4. Raucci U, Musolino AM, Di Lallo D, Piga S, Barbieri MA, Pisani M, et al. Impact of the COVID-19 pandemic on the emergency department of a tertiary children's hospital. Ital J Pediatr. 2021; 47:21.
Article5. Dighe A, Cattarino L, Cuomo-Dannenburg G, Skarp J, Imai N, Bhatia S, et al. Response to COVID-19 in South Korea and implications for lifting stringent interventions. BMC Med. 2020; 18:321.
Article6. Lim TH, Park JB, Je SM. Pediatric Korean Triage and Acuity Scale. Pediatr Emerg Med J. 2015; 2:53–8. Korean.
Article7. Korean Standard Statistical Classification. Classification of diseases [Internet]. Daejeon (Korea): Statistics Korea;c2021 [cited 2021 Jul 3]. Available from: https://kssc.kostat.go.kr:8443/ksscNew_web/ekssc/main/main.do#.8. The Lancet. COVID-19: protecting health-care workers. Lancet. 2020; 395:922.9. Dopfer C, Wetzke M, Zychlinsky Scharff A, Mueller F, Dressler F, Baumann U, et al. COVID-19 related reduction in pediatric emergency healthcare utilization - a concerning trend. BMC Pediatr. 2020; 20:427.
Article10. Mantica G, Riccardi N, Terrone C, Gratarola A. Non-COVID-19 visits to emergency departments during the pandemic: the impact of fear. Public Health. 2020; 183:40–1.
Article11. Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2021; 41:201–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in pediatric injury-related visits during coronavirus disease 2019 pandemic at a single regional emergency medical center in Korea
- Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
- Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
- Effect of coronavirus disease 2019 on febrile children’s visits to the emergency department of a tertiary hospital
- Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic