J Korean Neurosurg Soc.
2022 May;65(3):370-379. 10.3340/jkns.2021.0284.
Diagnosis of Abusive Head Trauma : Neurosurgical Perspective
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2529581
- DOI: http://doi.org/10.3340/jkns.2021.0284
Abstract
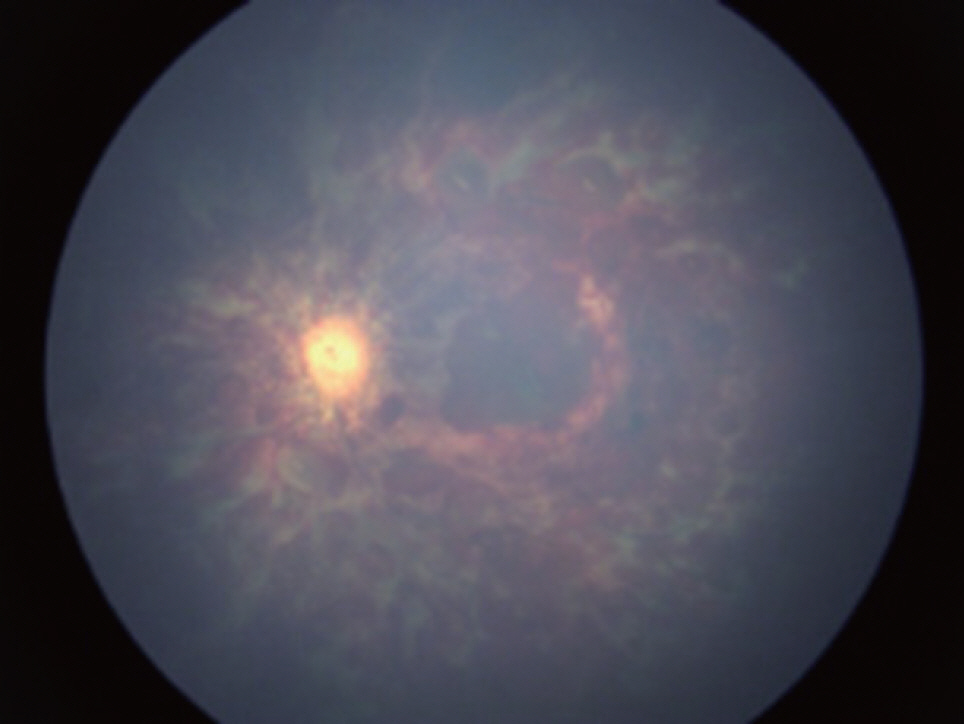
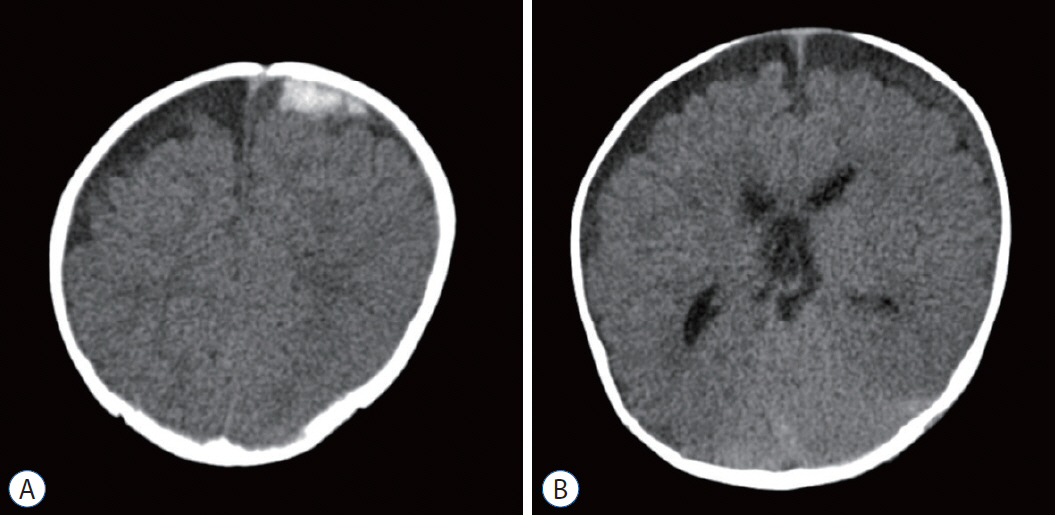
- Abusive head trauma (AHT) is the most severe form of physical abuse in children. Such injury involves traumatic damage to the head and/or spine of infants and young children. The term AHT was introduced to include a wider range of injury mechanisms, such as intentional direct blow, throw, and even penetrating trauma by perpetuator(s). Currently, it is recommended to replace the former term, shaken baby syndrome, which implicates shaking as the only mechanism, with AHT to include diverse clinical and radiological manifestations. The consequences of AHT cause devastating medical, social and financial burdens on families, communities, and victims. The potential harm of AHT to the developing brain and spinal cord of the victims is tremendous. Many studies have reported that the adverse effects of AHT are various and serious, such as blindness, mental retardation, physical limitation of daily activities and even psychological problems. Therefore, appropriate vigilance for the early recognition and diagnosis of AHT is highly recommended to stop and prevent further injuries. The aim of this review is to summarize the relevant evidence concerning the early recognition and diagnosis of AHT. To recognize this severe type of child abuse early, all health care providers maintain a high index of suspicion and vigilance. Such suspicion can be initiated with careful and thorough history taking and physical examinations. Previously developed clinical prediction rules can be helpful for decision-making regarding starting an investigation when considering meaningful findings. Even the combination of biochemical markers may be useful to predict AHT. For a more confirmative evaluation, neuroradiological imaging is required to find AHT-specific findings. Moreover, timely consultation with ophthalmologists is needed to find a very specific finding, retinal hemorrhage.
Keyword
Figure
Reference
-
References
1. Adamsbaum C, Grabar S, Mejean N, Rey-Salmon C. Abusive head trauma: judicial admissions highlight violent and repetitive shaking. Pediatrics. 126:546–555. 2010.
Article2. Badger S, Waugh MC, Hancock J, Marks S, Oakley K. Short term outcomes of children with abusive head trauma two years post injury: a retrospective study. J Pediatr Rehabil Med. 13:241–253. 2020.
Article3. Barlow KM, Minns RA. Annual incidence of shaken impact syndrome in young children. Lancet. 356:1571–1572. 2000.
Article4. Bennett S, Ward M, Moreau K, Fortin G, King J, Mackay M, et al. Head injury secondary to suspected child maltreatment: results of a prospective canadian national surveillance program. Child Abuse Negl. 35:930–936. 2011.
Article5. Berger RP, Fromkin J, Herman B, Pierce MC, Saladino RA, Flom L, et al. Validation of the Pittsburgh infant brain injury score for abusive head trauma. Pediatrics. 138:e20153756. 2016.
Article6. Berger RP, Pak BJ, Kolesnikova MD, Fromkin J, Saladino R, Herman BE, et al. Derivation and validation of a serum biomarker panel to identify infants with acute intracranial hemorrhage. JAMA Pediatr. 171:e170429. 2017.
Article7. Burkhart ZN, Thurber CJ, Chuang AZ, Kumar KS, Davis GH, Kellaway J. Risk factors associated with retinal hemorrhage in suspected abusive head trauma. J AAPOS. 19:119–123. 2015.
Article8. Buys YM, Levin AV, Enzenauer RW, Elder JE, Letourneau MA, Humphreys RP, et al. Retinal findings after head trauma in infants and young children. Ophthalmology. 99:1718–1723. 1992.
Article9. Case ME. Distinguishing accidental from inflicted head trauma at autopsy. Pediatr Radiol. 44:S632–S640. 2014.
Article10. Choudhary AK, Ishak R, Zacharia TT, Dias MS. Imaging of spinal injury in abusive head trauma: a retrospective study. Pediatr Radiol. 44:1130–1140. 2014.
Article11. Choudhary AK, Servaes S, Slovis TL, Palusci VJ, Hedlund GL, Narang SK, et al. Consensus statement on abusive head trauma in infants and young children. Pediatr Radiol. 48:1048–1065. 2018.
Article12. Christian CW, Block R. Abusive head trauma in infants and children. Pediatrics. 123:1409–1411. 2009.
Article13. Cory CZ, Jones BM. Can shaking alone cause fatal brain injury? A biomechanical assessment of the Duhaime shaken baby syndrome model. Med Sci Law. 43:317–333. 2003.14. Cowley LE, Morris CB, Maguire SA, Farewell DM, Kemp AM. Validation of a prediction tool for abusive head trauma. Pediatrics. 136:290–298. 2015.
Article15. Crumm CE, Brown ECB, Thomas-Smith S, Yu DTY, Metz JB, Feldman KW. Evaluation of an emergency department high-risk bruising screening protocol. Pediatrics. 147:e2020002444. 2021.
Article16. Dsouza R, Bertocci G. Impact sites representing potential bruising locations associated with bed falls in children. Forensic Sci Int. 286:86–95. 2018.
Article17. Duhaime AC, Christian CW, Rorke LB, Zimmerman RA. Nonaccidental head injury in infants--the “shaken-baby syndrome”. N Engl J Med. 338:1822–1829. 1998.
Article18. Eisele JA, Kegler SR, Trent RB, Coronado VG. Nonfatal traumatic brain injury-related hospitalization in very young children-15 states, 1999. J Head Trauma Rehabil. 21:537–543. 2006.
Article19. Ellingson KD, Leventhal JM, Weiss HB. Using hospital discharge data to track inflicted traumatic brain injury. Am J Prev Med. 34:S157–S162. 2008.
Article20. Feldman KW, Bethel R, Shugerman RP, Grossman DC, Grady MS, Ellenbogen RG. The cause of infant and toddler subdural hemorrhage: a prospective study. Pediatrics. 108:636–646. 2001.
Article21. Finnie JW, Blumbergs PC, Manavis J, Turner RJ, Helps S, Vink R, et al. Neuropathological changes in a lamb model of non-accidental head injury (the shaken baby syndrome). J Clin Neurosci. 19:1159–1164. 2012.
Article22. Garcia-Pires F, Jayappa S, Desai S, Ramakrishnaiah RH, Choudhary AK. Spinal subdural hemorrhage in abusive head trauma: a pictorial review. Pediatr Radiol. 51:980–990. 2021.
Article23. Geddes JF, Hackshaw AK, Vowles GH, Nickols CD, Whitwell HL. Neuropathology of inflicted head injury in children. I. Patterns of brain damage. Brain. 124:1290–1298. 2001.
Article24. Gencturk M, Tore HG, Nascene DR, Zhang L, Koksel Y, McKinney AM. Various cranial and orbital imaging findings in pediatric abusive and non-abusive head trauma, and relation to outcomes. Clin Neuroradiol. 29:253–261. 2019.
Article25. Gunda D, Cornwell BO, Dahmoush HM, Jazbeh S, Alleman AM. Pediatric central nervous system imaging of nonaccidental trauma: beyond subdural hematomas. Radiographics. 39:213–228. 2019.
Article26. Hanigan WC, Peterson RA, Njus G. Tin ear syndrome: rotational acceleration in pediatric head injuries. Pediatrics. 80:618–622. 1987.27. Hansen JB, Frazier T, Moffatt M, Zinkus T, Anderst JD. Evaluations for abuse in young children with subdural hemorrhages: findings based on symptom severity and benign enlargement of the subarachnoid spaces. J Neurosurg Pediatr. 21:31–37. 2018.
Article28. Hansen JB, Killough EF, Moffatt ME, Knapp JF. Retinal hemorrhages: abusive head trauma or not? Pediatr Emerg Care. 34:665–670. 2018.29. Hibberd O, Nuttall D, Watson RE, Watkins WJ, Kemp AM, Maguire S. Childhood bruising distribution observed from eight mechanisms of unintentional injury. Arch Dis Child. 102:1103–1109. 2017.
Article30. Hymel KP, Armijo-Garcia V, Foster R, Frazier TN, Stoiko M, Christie LM, et al. Validation of a clinical prediction rule for pediatric abusive head trauma. Pediatrics. 134:e1537–1544. 2014.
Article31. Hymel KP, Rumack CM, Hay TC, Strain JD, Jenny C. Comparison of intracranial computed tomographic (CT) findings in pediatric abusive and accidental head trauma. Pediatr Radiol. 27:743–747. 1997.
Article32. Hymel KP, Wang M, Chinchilli VM, Karst WA, Willson DF, Dias MS, et al. Estimating the probability of abusive head trauma after abuse evaluation. Child Abuse Negl. 88:266–274. 2019.
Article33. Hymel KP, Willson DF, Boos SC, Pullin DA, Homa K, Lorenz DJ, et al. Derivation of a clinical prediction rule for pediatric abusive head trauma. Pediatr Crit Care Med. 14:210–220. 2013.
Article34. Jacob R, Cox M, Koral K, Greenwell C, Xi Y, Vinson L, et al. MR imaging of the cervical spine in nonaccidental trauma: a tertiary institution experience. AJNR Am J Neuroradiol. 37:1944–1950. 2016.
Article35. Keenan HT, Runyan DK, Marshall SW, Nocera MA, Merten DF, Sinal SH. A population-based study of inflicted traumatic brain injury in young children. JAMA. 290:621–626. 2003.
Article36. Kelly P, Farrant B. Shaken baby syndrome in New Zealand, 2000-2002. J Paediatr Child Health. 44:99–107. 2008.
Article37. Kelly P, John S, Vincent AL, Reed P. Abusive head trauma and accidental head injury: a 20-year comparative study of referrals to a hospital child protection team. Arch Dis Child. 100:1123–1130. 2015.
Article38. Kemp AM, Jaspan T, Griffiths J, Stoodley N, Mann MK, Tempest V, et al. Neuroimaging: what neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch Dis Child. 96:1103–1112. 2011.
Article39. Kemp AM, Maguire SA, Nuttall D, Collins P, Dunstan F. Bruising in children who are assessed for suspected physical abuse. Arch Dis Child. 99:108–113. 2014.
Article40. Koumellis P, McConachie NS, Jaspan T. Spinal subdural haematomas in children with non-accidental head injury. Arch Dis Child. 94:216–219. 2009.
Article41. Ludwig S, Warman M. Shaken baby syndrome: a review of 20 cases. Ann Emerg Med. 13:104–107. 1984.
Article42. Maguire S, Mann M. Systematic reviews of bruising in relation to child abuse-what have we learnt: an overview of review updates. Evid Based Child Health. 8:255–263. 2013.
Article43. Maguire SA, Kemp AM, Lumb RC, Farewell DM. Estimating the probability of abusive head trauma: a pooled analysis. Pediatrics. 128:e550–e564. 2011.
Article44. Maguire SA, Watts PO, Shaw AD, Holden S, Taylor RH, Watkins WJ, et al. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: a systematic review. Eye (Lond). 27:28–36. 2013.
Article45. Manfield J, Oakley K, Macey JA, Waugh MC. Understanding the five-year outcomes of abusive head trauma in children: a retrospective cohort study. Dev Neurorehabil. 24:361–367. 2021.
Article46. Matschke J, Büttner A, Bergmann M, Hagel C, Püschel K, Glatzel M. Encephalopathy and death in infants with abusive head trauma is due to hypoxic-ischemic injury following local brain trauma to vital brainstem centers. Int J Legal Med. 129:105–114. 2015.
Article47. McKeag H, Christian CW, Rubin D, Daymont C, Pollock AN, Wood J. Subdural hemorrhage in pediatric patients with enlargement of the subarachnoid spaces. J Neurosurg Pediatr. 11:438–444. 2013.
Article48. McNeely PD, Atkinson JD, Saigal G, O’Gorman AM, Farmer JP. Subdural hematomas in infants with benign enlargement of the subarachnoid spaces are not pathognomonic for child abuse. AJNR Am J Neuroradiol. 27:1725–1728. 2006.49. Minns RA, Jones PA, Mok JY. Annual incidence of shaken impact syndrome in young children. Am J Prev Med. 34:S126–S133. 2008.50. Narang SK, Fingarson A, Lukefahr J, Council on Child Abuse. Abusive head trauma in infants and children. Pediatrics. 145:e20200203. 2020.
Article51. Oates AJ, Sidpra J, Mankad K. Parenchymal brain injuries in abusive head trauma. Pediatr Radiol. 51:898–910. 2021.
Article52. Paek SH, Jung JH, Kwak YH, Kim DK, Ryu JM, Noh H, et al. Development of screening tool for child abuse in the Korean emergency department: using modified Delphi study. Medicine (Baltimore). 97:e13724. 2018.53. Pfeiffer H, Crowe L, Kemp AM, Cowley LE, Smith AS, Babl FE, et al. Clinical prediction rules for abusive head trauma: a systematic review. Arch Dis Child. 103:776–783. 2018.
Article54. Pierce MC, Kaczor K, Aldridge S, O’Flynn J, Lorenz DJ. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 125:67–74. 2010.
Article55. Pierce MC, Kaczor K, Lorenz DJ, Bertocci G, Fingarson AK, Makoroff K, et al. Validation of a clinical decision rule to predict abuse in young children based on bruising characteristics. JAMA Netw Open. 4:e215832. 2021.
Article56. Piteau SJ, Ward MG, Barrowman NJ, Plint AC. Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: a systematic review. Pediatrics. 130:315–323. 2012.
Article57. Reece RM, Sege R. Childhood head injuries: accidental or inflicted? Arch Pediatr Adolesc Med. 154:11–15. 2000.58. Roach JP, Acker SN, Bensard DD, Sirotnak AP, Karrer FM, Partrick DA. Head injury pattern in children can help differentiate accidental from non-accidental trauma. Pediatr Surg Int. 30:1103–1106. 2014.
Article59. Shanahan ME, Zolotor AJ, Parrish JW, Barr RG, Runyan DK. National, regional, and state abusive head trauma: application of the CDC algorithm. Pediatrics. 132:e1546–e1553. 2013.
Article60. Sibert JR, Payne EH, Kemp AM, Barber M, Rolfe K, Morgan RJ, et al. The incidence of severe physical child abuse in wales. Child Abuse Negl. 26:267–276. 2002.
Article61. Suh DY, Davis PC, Hopkins KL, Fajman NN, Mapstone TB. Nonaccidental pediatric head injury: diffusion-weighted imaging findings. Neurosurgery. 49:309–318. 2001.
Article62. Thackeray JD, Scribano PV, Lindberg DM. Yield of retinal examination in suspected physical abuse with normal neuroimaging. Pediatrics. 125:e1066–e1071. 2010.
Article63. Thomas AG, Hegde SV, Dineen RA, Jaspan T. Patterns of accidental craniocerebral injury occurring in early childhood. Arch Dis Child. 98:787–792. 2013.
Article64. Tung GA, Kumar M, Richardson RC, Jenny C, Brown WD. Comparison of accidental and nonaccidental traumatic head injury in children on noncontrast computed tomography. Pediatrics. 118:626–633. 2006.65. Westrick AC, Moore M, Monk S, Greeno A, Shannon C. Identifying characteristics in abusive head trauma: a single-institution experience. Pediatr Neurosurg. 50:179–186. 2015.
Article66. Wright JN. CNS injuries in abusive head trauma. AJR Am J Roentgenol. 208:991–1001. 2017.
Article67. Zimmerman RA, Bilaniuk LT, Farina L. Non-accidental brain trauma in infants: diffusion imaging, contributions to understanding the injury process. J Neuroradiol. 34:109–114. 2007.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging of Abusive Head Trauma : A Radiologists’ Perspective
- Abusive Head Trauma in Infants and Children in Japan
- Complex Pathophysiology of Abusive Head Trauma with Poor Neurological Outcome in Infants
- Smartphone Fundus Photography in an Infant with Abusive Head Trauma
- Abusive Head Traumas in 4 Infants