J Yeungnam Med Sci.
2022 Apr;39(2):153-160. 10.12701/yujm.2021.01039.
Idiopathic multicentric Castleman disease presenting progressive reticular honeycomb infiltration of lung and immunoglobulin G and immunoglobulin G4 dominant hypergammaglobulinemia: a case report
- Affiliations
-
- 1Division of Rheumatology, Department of Internal Medicine, CHA Gumi Medical Center, CHA University, Gumi, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2529274
- DOI: http://doi.org/10.12701/yujm.2021.01039
Abstract
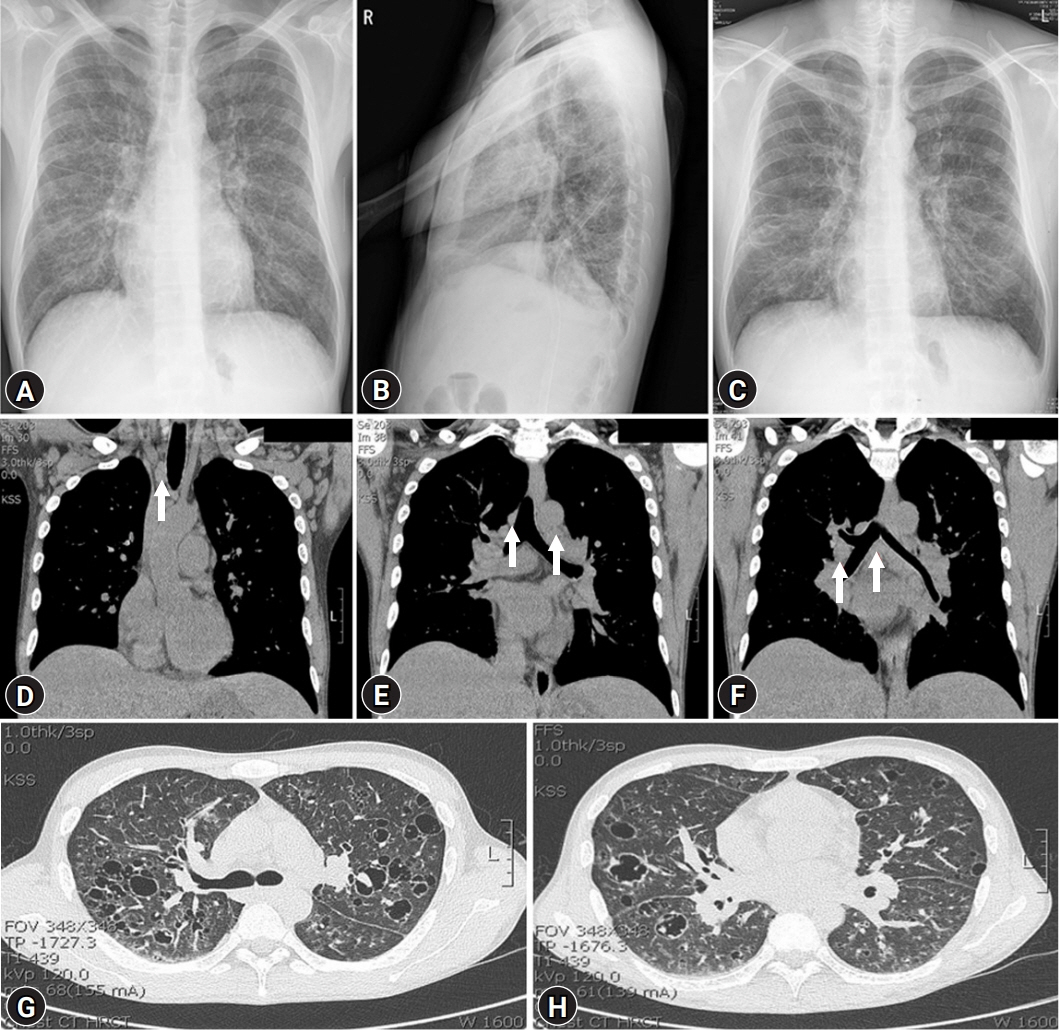
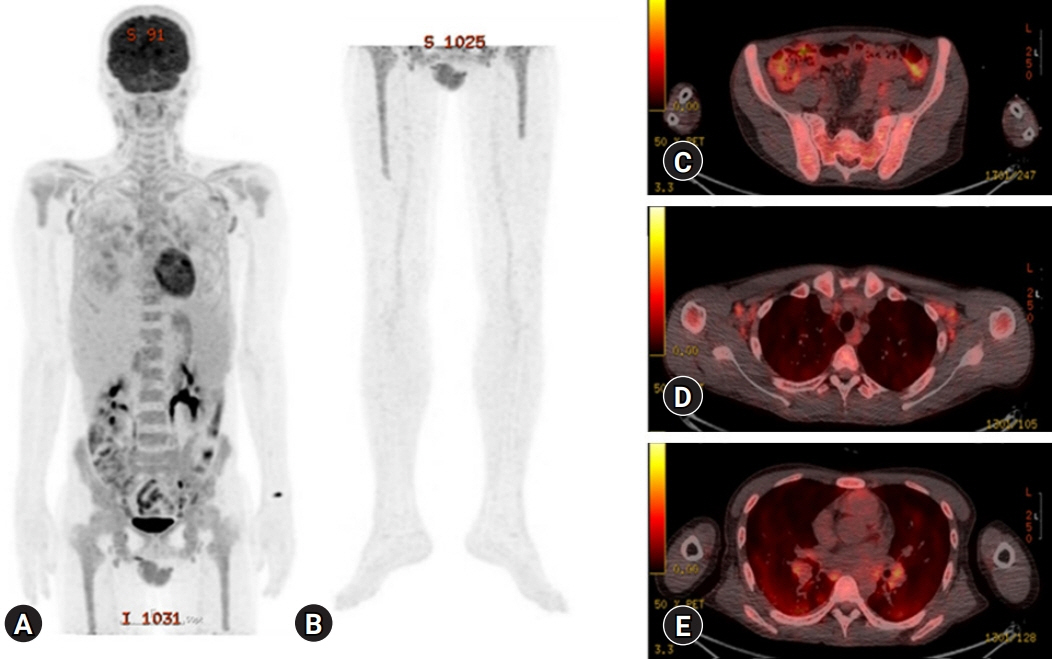
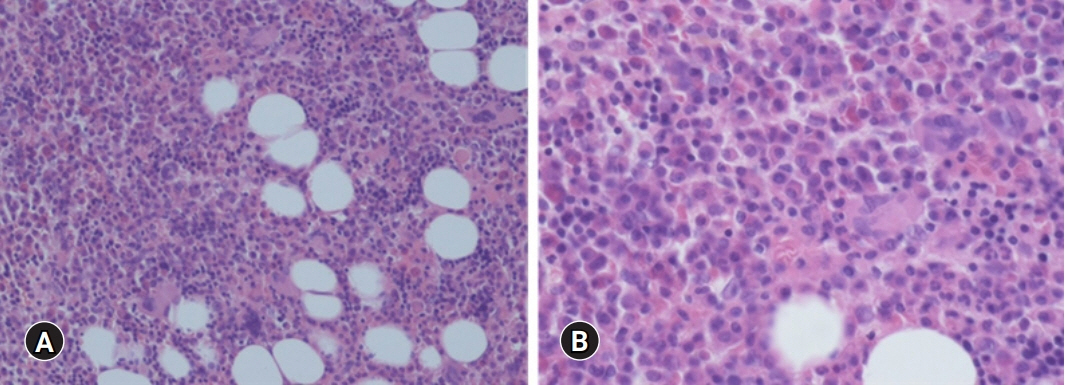
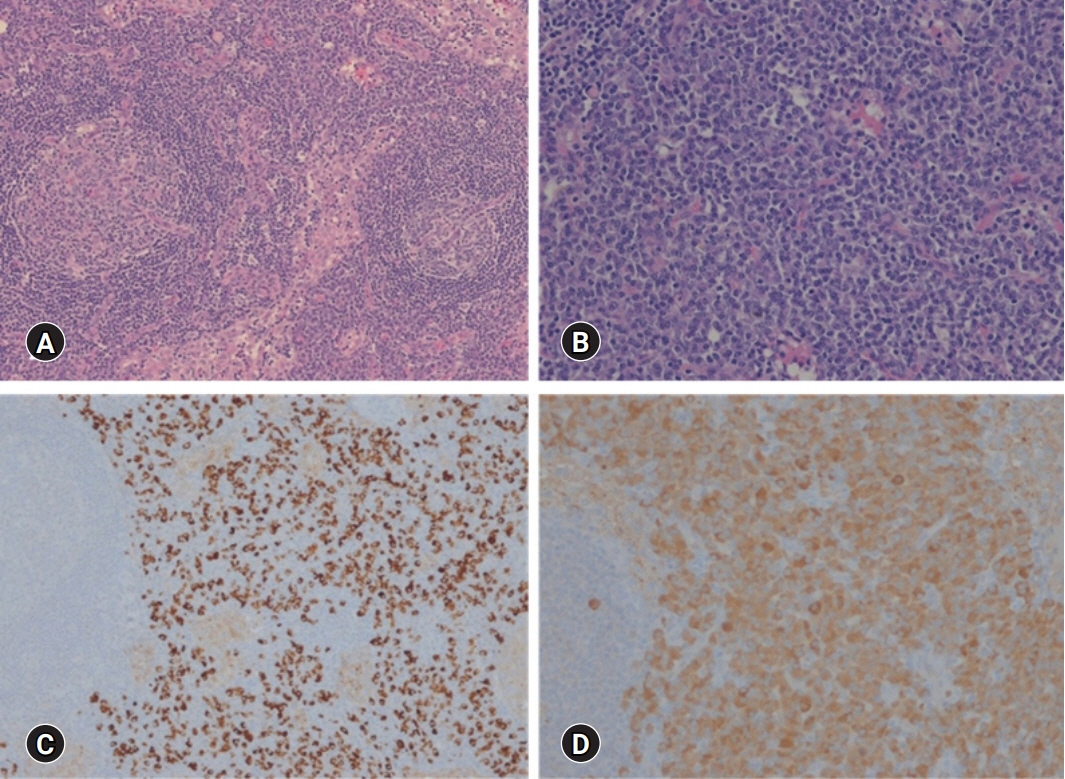
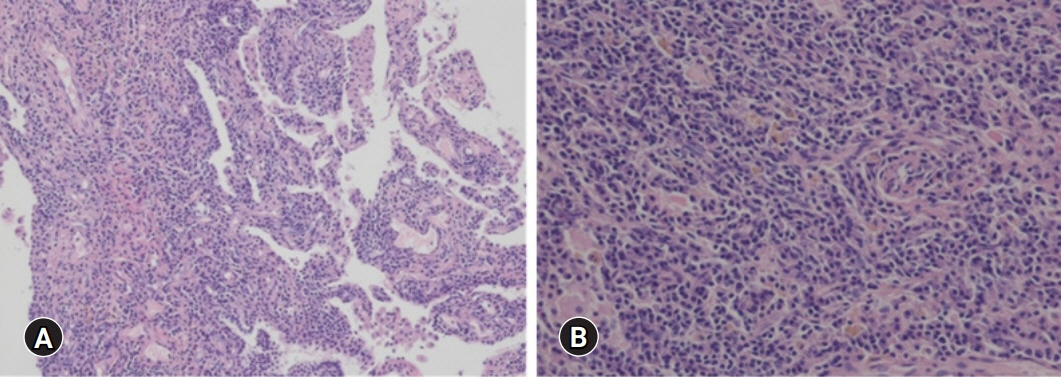
- Multicentric Castleman disease (MCD) is an uncommon systemic lymphoproliferative disorder that may cause multiple organ damage. Castleman disease-associated diffuse parenchymal lung disease (DPLD) has not been well studied. A 32-year-old man was referred to our hospital for progressive generalized weakness, light-headedness, and dyspnea on exertion for more than one year. Laboratory evaluations showed profound anemia, an elevated erythrocyte sedimentation rate, and an increased C-reactive protein level with polyclonal hypergammaglobulinemia. Chest radiography, computed tomography (CT), and positron emission tomography-CT scan demonstrated diffuse lung infiltration with multiple cystic lesions and multiple lymphadenopathy. In addition to these clinical laboratory findings, bone marrow, lung, and lymph node biopsies confirmed the diagnosis of idiopathic MCD (iMCD). Siltuximab, an interleukin-6 inhibitor, and glucocorticoid therapy were initiated. The patient has been tolerating the treatment well and had no disease progression or any complications in 4 years. Herein, we report this case of human herpesvirus-8-negative iMCD-associated DPLD accompanied by multiple cystic lesions, multiple lymphadenopathy, and polyclonal hypergammaglobulinemia with elevated immunoglobulin G (IgG) and IgG4 levels. We recommend a close evaluation of MCD in cases of DPLD with hypergammaglobulinemia.
Keyword
Figure
Reference
-
References
1. Castleman B, Iverson L, Menendez VP. Localized mediastinal lymphnode hyperplasia resembling thymoma. Cancer. 1956; 9:822–30.2. Fajgenbaum DC, Shilling D. Castleman disease pathogenesis. Hematol Oncol Clin North Am. 2018; 32:11–21.3. Shahidi H, Myers JL, Kvale PA. Castleman’s disease. Mayo Clin Proc. 1995; 70:969–77.4. Takenaka K, Takada K, Kobayashi D, Moriguchi M, Harigai M, Miyasaka N. A case of IgG4-related disease with features of Mikulicz’s disease, and retroperitoneal fibrosis and lymphadenopathy mimicking Castleman’s disease. Mod Rheumatol. 2011; 21:410–4.5. Huang H, Feng R, Li J, Song X, Li S, Xu K, et al. Castleman disease-associated diffuse parenchymal lung disease: A STROBE-compliant retrospective observational analysis of 22 cases in a tertiary Chinese hospital. Medicine (Baltimore). 2017; 96:e8173.6. Fajgenbaum DC, Uldrick TS, Bagg A, Frank D, Wu D, Srkalovic G, et al. International, evidence-based consensus diagnostic criteria for HHV-8-negative/idiopathic multicentric Castleman disease. Blood. 2017; 129:1646–57.7. Wallace ZS, Naden RP, Chari S, Choi H, Della-Torre E, Dicaire JF, et al. The 2019 American College of Rheumatology/European League Against Rheumatism classification criteria for IgG4-related disease. Arthritis Rheumatol. 2020; 72:7–19.8. Oksenhendler E, Boutboul D, Fajgenbaum D, Mirouse A, Fieschi C, Malphettes M, et al. The full spectrum of Castleman disease: 273 patients studied over 20 years. Br J Haematol. 2018; 180:206–16.9. Bowne WB, Lewis JJ, Filippa DA, Niesvizky R, Brooks AD, Burt ME, et al. The management of unicentric and multicentric Castleman’s disease: a report of 16 cases and a review of the literature. Cancer. 1999; 85:706–17.10. Palestro G, Turrini F, Pagano M, Chiusa L. Castleman’s disease. Adv Clin Path. 1999; 3:11–22.11. Vassallo R, Ryu JH, Colby TV, Hartman T, Limper AH. Pulmonary Langerhans’-cell histiocytosis. N Engl J Med. 2000; 342:1969–78.12. Inoue D, Zen Y, Abo H, Gabata T, Demachi H, Kobayashi T, et al. Immunoglobulin G4-related lung disease: CT findings with pathologic correlations. Radiology. 2009; 251:260–70.13. Mochizuki H, Kato M, Higuchi T, Koyamada R, Arai S, Okada S, et al. Overlap of IgG4-related disease and multicentric Castleman’s disease in a patient with skin lesions. Intern Med. 2017; 56:1095–9.14. Sato Y, Kojima M, Takata K, Morito T, Asaoku H, Takeuchi T, et al. Systemic IgG4-related lymphadenopathy: a clinical and pathologic comparison to multicentric Castleman’s disease. Mod Pathol. 2009; 22:589–99.15. van Rhee F, Voorhees P, Dispenzieri A, Fosså A, Srkalovic G, Ide M, et al. International, evidence-based consensus treatment guidelines for idiopathic multicentric Castleman disease. Blood. 2018; 132:2115–24.16. Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, et al. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003; 38:982–4.17. Yamashita K, Haga H, Kobashi Y, Miyagawa-Hayashino A, Yoshizawa A, Manabe T. Lung involvement in IgG4-related lymphoplasmacytic vasculitis and interstitial fibrosis: report of 3 cases and review of the literature. Am J Surg Pathol. 2008; 32:1620–6.18. Liu AY, Nabel CS, Finkelman BS, Ruth JR, Kurzrock R, van Rhee F, et al. Idiopathic multicentric Castleman’s disease: a systematic literature review. Lancet Haematol. 2016; 3:e163–75.19. van Rhee F, Greenway A, Stone K. Treatment of idiopathic Castleman disease. Hematol Oncol Clin North Am. 2018; 32:89–106.20. van Rhee F, Casper C, Voorhees PM, Fayad LE, van de Velde H, Vermeulen J, et al. A phase 2, open-label, multicenter study of the long-term safety of siltuximab (an anti-interleukin-6 monoclonal antibody) in patients with multicentric Castleman disease. Oncotarget. 2015; 6:30408–19.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Immunoglobulin G4-Related Sclerosing Disease Mimicking Lung Cancer
- A Case of Recurrent Ischemic Stroke Associated with Immunoglobulin G4-Related Disease
- Human Herpesvirus-8 Positive Multicentric Castleman’s Disease with Complete Response after Rituximab Monotherapy: A Case Report
- Immunoglobulin G4 Related Ophthalmic Disease Presenting as Diplopia and Headache
- Immunoglobulin G4-Related Lung Disease Mimicking Lung Cancer: Two Case Reports