J Korean Diabetes.
2022 Mar;23(1):64-75. 10.4093/jkd.2022.23.1.64.
Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
- Affiliations
-
- 1Department of Nursing, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Diabetes Education Unit, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- 3Diabetes Education Unit, Gangnam Severance Hospital, Yonsei University, Seoul, Korea
- 4Diabetes Education Unit, The Catholic University of Korea, Yeouido St. Mary’s Hospital, Seoul, Korea
- 5Department of Nursing, Inje University Ilsan Paik Hospital, Goyang, Korea
- 6Diabetes Education Unit, Gwangmyeong Sungae Hospital, Gwangmyeong, Korea
- 7Department of Nursing, The Catholic University of Korea, Bucheon St. Mary’s Hospital, Bucheon, Korea
- 8Diabetes Education Unit, Asan Medical Center, Seoul, Korea
- 9Diabetes Education Unit, The Catholic University of Korea, Seoul St. Mary’s Hospital, Seoul, Korea
- 10Diabetes Education Unit, Samsung Medical Center, Seoul, Korea
- 11Korean Association of Diabetes Nurse Educators
- KMID: 2528413
- DOI: http://doi.org/10.4093/jkd.2022.23.1.64
Abstract
- Background
This study aimed to explore the long-term management of diabetes patients in domestic general hospitals by reviewing 2013 and 2018 data on diabetes management status.
Methods
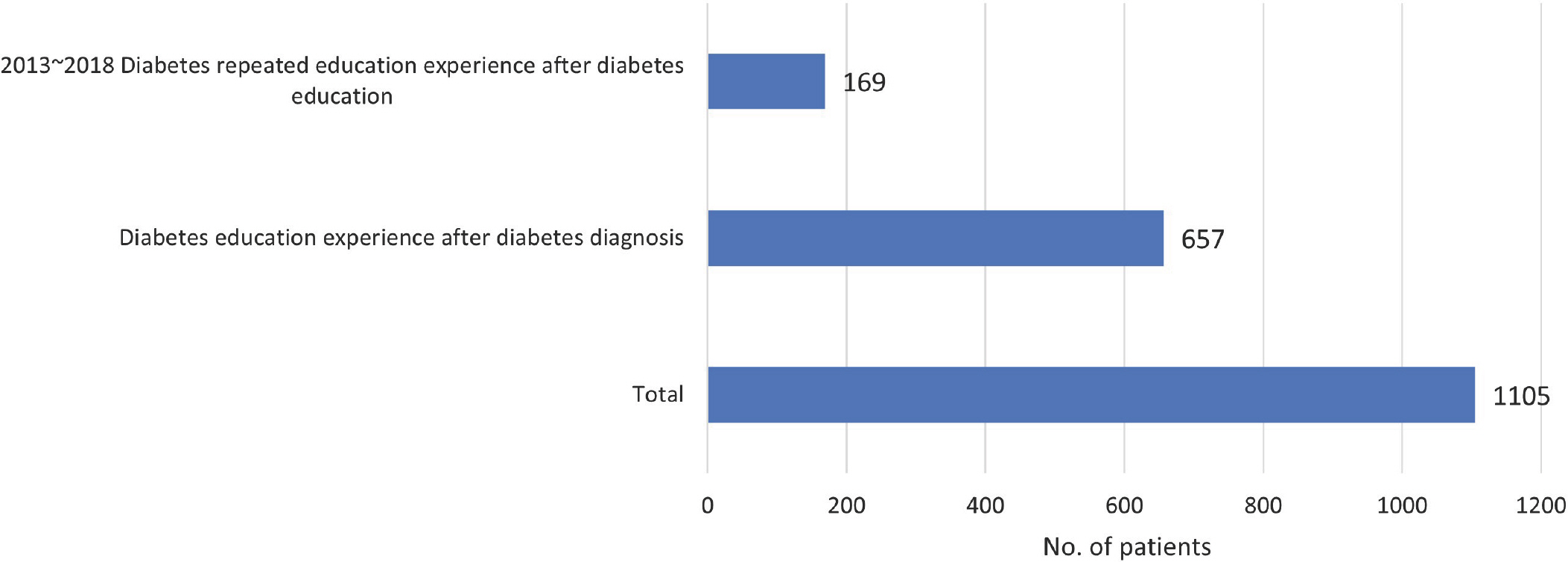
Of 1,802 type 2 diabetes patients who received outpatient treatment at nine general hospitals in Korea and who participated in the 2013 study, 1,124 were enrolled in this study. General characteristics, comorbidities, complications, and management were investigated through medical records.
Results
The average age of the subjects was 65.4 ± 10.6 years, the average duration of diabetes mellitus was 15.6 ± 8.0 years, and 58.2% of the subjects had a family history of diabetes. Concomitant diseases were hypertension in 63.0% and dyslipidemia in 78.8%. Diabetic retinopathy was observed in 31.5%, nephropathy in 24.6%, and neuropathy in 24.5%. The mean glycosylated hemoglobin (HbA1c) level was 7.4 ± 2.2% and according to Korean Diabetes Association guidelines, 20.4% of patients with diabetes achieved a HbA1c level of < 6.5%, 70.1% achieved a blood pressure of < 140/85 mm Hg, and 77.1% achieved a low density lipoprotein cholesterol level of < 100 mg/dL. The target achievement rate was 12.5% for blood sugar, blood pressure, and lipid parameters.
Conclusion
In diabetes management, blood sugar control was poor compared to blood pressure and lipid control. A systematic management plan is needed to ensure proper blood sugar control.
Figure
Reference
-
1.Cho NH., Shaw JE., Karuranga S., Huang Y., da Rocha Fer-nandes JD., Ohlrogge AW, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018. 138:271–81.
Article2.Jung CH., Son JW., Kang S., Kim WJ., Kim HS., Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J. 2021. 45:1–10.
Article3.Statistics Korea. 2019 statistics of causes of death for Korea. Available from: http://kostat.go.kr/portal/korea/kor_nw/1/6/2/index.board?bmode=read&aSe-q=385219&pageNo=&rowNum=10&amSeq=&sTar-get=&sTxt= (updated 2020 Sep 22).4.Korean Diabetes Association. Diabetes & complications in Korea. Available from: https://www.diabetes.or.kr/bbs/skin/dianews/download.php?code=admin&num-ber=2009.5.The CONTROL Group. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009. 52:2288–98. Erratum in: Diabetologia 2009;52:2470.6.Stratton IM., Cull CA., Adler AI., Matthews DR., Neil HA., Holman RR. Additive effects of glycaemia and blood pressure exposure on risk of complications in type 2 diabetes: a prospective observational study (UKPDS 75). Diabetologia. 2006. 49:1761–9.
Article7.Mitsios JP., Ekinci EI., Mitsios GP., Churilov L., Thijs V. Relationship between glycated hemoglobin and stroke risk: a systematic review and meta-analysis. J Am Heart Assoc. 2018. 7:e007858.
Article8.Korean Diabetes Association. 2019 treatment guideline for diabetes. Seoul: Korean Diabetes Association;2019. p. 33–41.9.American Diabetes Association. 6. Glycemic targets: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019. 42(Suppl 1):S61–70.10.American Diabetes Association. 5. Lifestyle management: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019. 42(Suppl 1):S46–60.11.Centers for Disease Control and Prevention. 2020 National diabetes statistics report. Available from: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf.12.Jung JH., Lee JH., Noh JW., Park JE., Kim HS., Yoo JW, et al. Current status of management in type 2 diabetes mellitus at general hospitals in South Korea. Diabetes Metab J. 2015. 39:307–15.
Article13.Seo DH., Kang S., Lee YH., Ha JY., Park JS., Lee BW, et al. Current management of type 2 diabetes mellitus in primary care clinics in Korea. Endocrinol Metab (Seoul). 2019. 34:282–90.
Article14.Chen R., Ji L., Chen L., Chen L., Cai D., Feng B, et al. Glycemic control rate of T2DM outpatients in China: a multi-center survey. Med Sci Monit. 2015. 21:1440–6.
Article15.Ha KH., Kim DJ. Current status of managing diabetes mellitus in Korea. Korean J Intern Med. 2016. 31:845–50.
Article16.Song SJ., Han K., Choi KS., Ko SH., Rhee EJ., Park CY, et al. Trends in diabetic retinopathy and related medical practices among type 2 diabetes patients: results from the National Insurance Service Survey 2006-2013. J Diabetes Investig. 2018. 9:173–8.
Article17.Zhang X., Saaddine JB., Chou CF., Cotch MF., Cheng YJ., Geiss LS, et al. Prevalence of diabetic retinopathy in the United States, 2005-2008. JAMA. 2010. 304:649–56.
Article18.Mao W., Yip CW., Chen W. Complications of diabetes in China: health system and economic implications. BMC Public Health. 2019. 19:269.
Article19.Afkarian M., Zelnick LR., Hall YN., Heagerty PJ., Tuttle K., Weiss NS, et al. Clinical manifestations of kidney disease among US adults with diabetes, 1988-2014. JAMA. 2016. 316:602–10.
Article20.Song KH., Jeong JS., Kim MK., Kwon HS., Baek KH., Ko SH, et al. Discordance in risk factors for the progression of diabetic retinopathy and diabetic nephropathy in patients with type 2 diabetes mellitus. J Diabetes Investig. 2019. 10:745–52.
Article21.Callaghan BC., Cheng HT., Stables CL., Smith AL., Feld-man EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. 2012. 11:521–34.
Article22.Su JB., Zhao LH., Zhang XL., Cai HL., Huang HY., Xu F, et al. HbA1c variability and diabetic peripheral neuropathy in type 2 diabetic patients. Cardiovasc Diabetol. 2018. 17:47.
Article23.Jung CH., Chung JO., Han K., Ko SH., Ko KS., Park JY. Improved trends in cardiovascular complications among subjects with type 2 diabetes in Korea: a nationwide study (2006-2013). Cardiovasc Diabetol. 2017. 16:1.
Article24.Zheng Y., Ley SH., Hu FB. Global aetiology and epidemiol-ogy of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018. 14:88–98.
Article25.Wan EYF., Fung CSC., Yu EYT., Chin WY., Fong DYT., Chan AKC, et al. Effect of multifactorial treatment targets and relative importance of hemoglobin A1c, blood pressure, and low-density lipoprotein-cholesterol on cardiovascular diseases in Chinese primary care patients with type 2 diabetes mellitus: a population-based retrospective cohort study. J Am Heart Assoc. 2017. 6:e006400.
Article26.Chrvala CA., Sherr D., Lipman RD. Diabetes self-management education for adults with type 2 diabetes mellitus: a systematic review of the effect on glycemic control. Patient Educ Couns. 2016. 99:926–43.
Article27.Chatterjee S., Davies MJ., Heller S., Speight J., Snoek FJ., Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. 2018. 6:130–42. Erratum in: Lancet Diabetes Endocrinol 2018;6:e2.
Article28.He X., Li J., Wang B., Yao Q., Li L., Song R, et al. Diabetes self-management education reduces risk of all-cause mortality in type 2 diabetes patients: a systematic review and meta-analysis. Endocrine. 2017. 55:712–31.
Article29.Kim JM., Hong JW., Noh JH., Kim DJ. Factors associated with participation in diabetes education: The Korea National Health and Nutrition Examination Survey 2007 to 2009. Diabetes Metab J. 2016. 40:447–53.
Article30.Kim HS., Kim H., Yang HK., Lee EY., Jeong YJ., Kim TM, et al. Physician-directed diabetes education without a medi-cation change and associated patient outcomes. Diabetes Metab J. 2017. 41:187–94.
Article31.McBrien KA., Naugler C., Ivers N., Weaver RG., Campbell D., Desveaux L, et al. Barriers to care in patients with diabetes and poor glycemic control- a cross-sectional survey. PLoS One. 2017. 12:e0176135.32.Kim MY., Suh S., Jin SM., Kim SW., Bae JC., Hur KY, et al. Education as prescription for patients with type 2 diabetes mellitus: compliance and efficacy in clinical practice. Diabetes Metab J. 2012. 36:452–9.
Article33.Yong YM., Shin KM., Lee KM., Cho JY., Ko SH., Yoon MH, et al. Intensive individualized reinforcement education is important for the prevention of hypoglycemia in patients with type 2 diabetes. Diabetes Metab J. 2015. 39:154–63.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Why Does the MOHW Consider Type 2 Diabetes Mellitus to be a Slight Illness?
- Comprehensive Management in Patients with Type 2 Diabetes Mellitus
- Successful Management of Tardive Dyskinesia with Quetiapine and Clonazepam in a Patient of Schizophrenia with Type 2 Diabetes Mellitus
- Genetics in Diabetes Mellitus - Contribution to the Classification and Management
- Management of Type 1 Diabetes Mellitus in Adults