Korean J Pain.
2022 Apr;35(2):152-159. 10.3344/kjp.2022.35.2.152.
Effectiveness of graded motor imagery in subjects with frozen shoulder: a pilot randomized controlled trial
- Affiliations
-
- 1Department of Orthopedic Physiotherapy, KAHER Institute of Physiotherapy, Belagavi, India
- KMID: 2527766
- DOI: http://doi.org/10.3344/kjp.2022.35.2.152
Abstract
- Background
Subjects with frozen shoulder (FS) might not be comfortable with vigorous physical therapy. Clinical trials assessing the effect of graded motor imagery (GMI) in FS are lacking. The aim of this study was to determine the effect of GMI as an adjunct to conventional physiotherapy in individuals with painful FS.
Methods
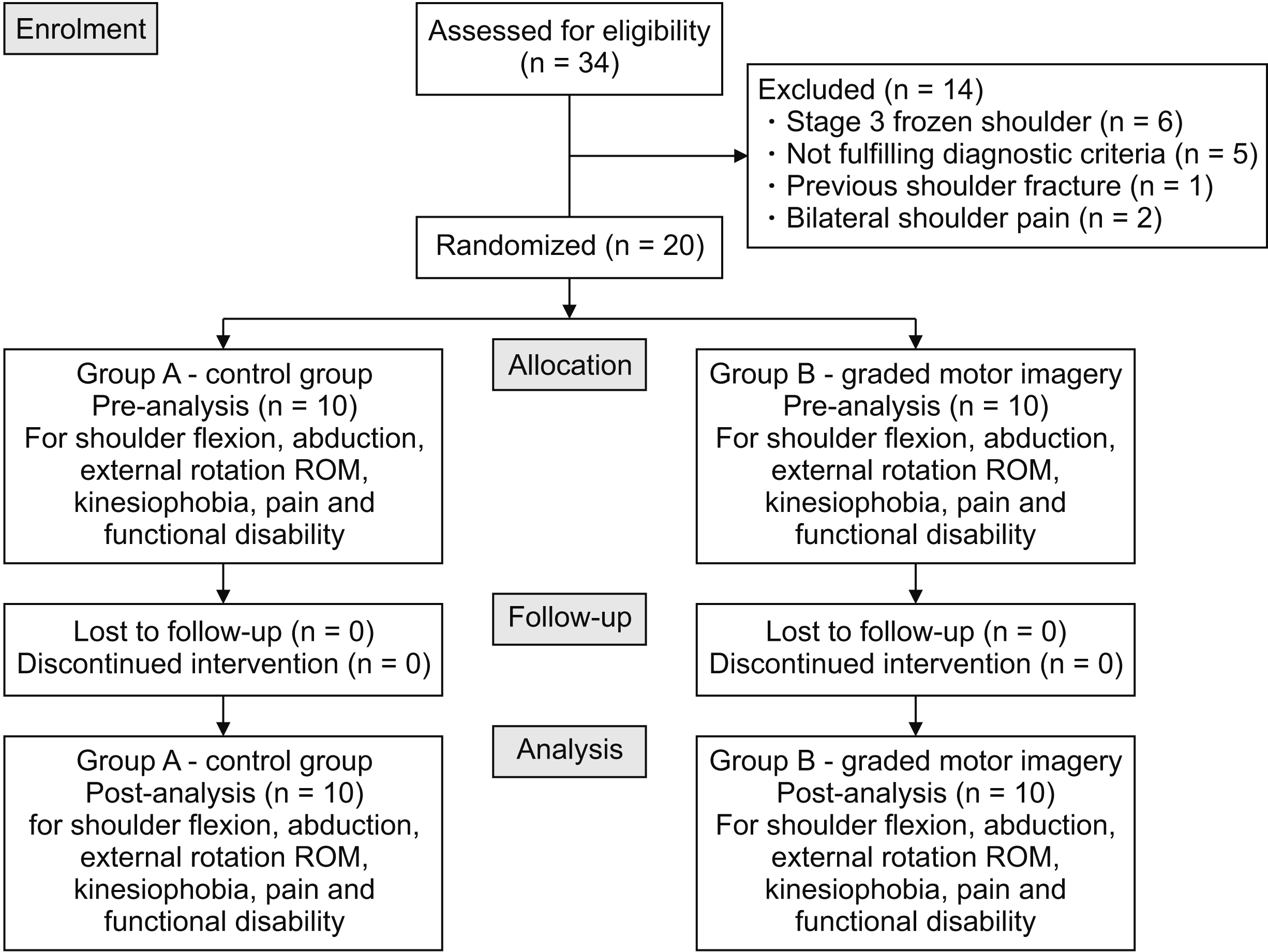
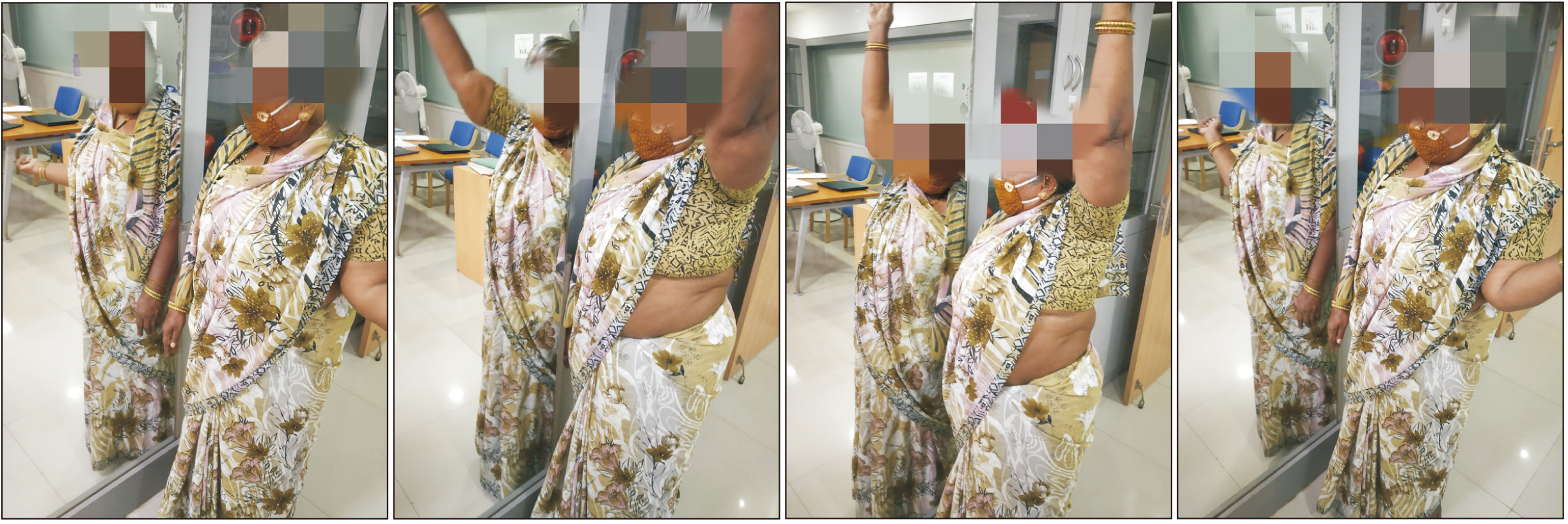
Twenty subjects aged 40–65 years having stage I and II of FS were randomly divided into two study groups. The conventional physiotherapy group (n = 10) received electrotherapy and exercises while the GMI group (n = 10) received GMI along with the conventional physiotherapy thrice a week for 3 weeks. Pre- (Session 1) and post- (Session 9) intervention analysis for flexion, abduction, and external rotation range of motion (ROM) using a universal goniometer, fear of movement using the fear avoidance belief questionnaire (FABQ), pain with the visual analogue scale, and functional disability using the shoulder pain and disability index (SPADI) was done by a blinded assessor.
Results
Statistically significant difference was seen within both the groups for all the outcomes. In terms of increasing abduction ROM as well as reducing fear of movement, pain, and functional disability, the GMI group was significantly better than control group. However, both groups were equally effective for improving flexion and external rotation ROM.
Conclusions
Addition of GMI to the conventional physiotherapy proved to be superior to conventional physiotherapy alone in terms of reducing pain, kinesiophobia, and improving shoulder function for stage I and II of FS.
Keyword
Figure
Cited by 1 articles
-
The effect of graded motor imagery training on pain, functional performance, motor imagery skills, and kinesiophobia after total knee arthroplasty: randomized controlled trial
Busra Candiri, Burcu Talu, Emre Guner, Metehan Ozen
Korean J Pain. 2023;36(3):369-381. doi: 10.3344/kjp.23020.
Reference
-
1. Chan HBY, Pua PY, How CH. 2017; Physical therapy in the management of frozen shoulder. Singapore Med J. 58:685–9. DOI: 10.11622/smedj.2017107. PMID: 29242941. PMCID: PMC5917053.
Article2. Uppal HS, Evans JP, Smith C. 2015; Frozen shoulder: a systematic review of therapeutic options. World J Orthop. 6:263–8. DOI: 10.5312/wjo.v6.i2.263. PMID: 25793166. PMCID: PMC4363808.
Article3. Cho CH, Bae KC, Kim DH. 2019; Treatment strategy for frozen shoulder. Clin Orthop Surg. 11:249–57. DOI: 10.4055/cios.2019.11.3.249. PMID: 31475043. PMCID: PMC6695331.
Article4. Kelley MJ, McClure PW, Leggin BG. 2009; Frozen shoulder: evidence and a proposed model guiding rehabilitation. J Orthop Sports Phys Ther. 39:135–48. DOI: 10.2519/jospt.2009.2916. PMID: 19194024.
Article5. Brue S, Valentin A, Forssblad M, Werner S, Mikkelsen C, Cerulli G. 2007; Idiopathic adhesive capsulitis of the shoulder: a review. Knee Surg Sports Traumatol Arthrosc. 15:1048–54. DOI: 10.1007/s00167-007-0291-2. PMID: 17333122.
Article6. Page P, Labbe A. 2010; Adhesive capsulitis: use the evidence to integrate your interventions. N Am J Sports Phys Ther. 5:266–73. PMID: 21655385. PMCID: PMC3096148.7. Dias R, Cutts S, Massoud S. 2005; Frozen shoulder. BMJ. 331:1453–6. DOI: 10.1136/bmj.331.7530.1453. PMID: 16356983. PMCID: PMC1315655.
Article8. Kelley MJ, Shaffer MA, Kuhn JE, Michener LA, Seitz AL, Uhl TL, et al. 2013; Shoulder pain and mobility deficits: adhesive capsulitis. J Orthop Sports Phys Ther. 43:A1–31. DOI: 10.2519/jospt.2013.0302. PMID: 23636125.
Article9. Hannafin JA, Chiaia TA. 2000; Adhesive capsulitis. A treatment approach. Clin Orthop Relat Res. 372:95–109. DOI: 10.1097/00003086-200003000-00012. PMID: 10738419.10. Jain TK, Sharma NK. 2014; The effectiveness of physiotherapeutic interventions in treatment of frozen shoulder/adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. 27:247–73. DOI: 10.3233/BMR-130443. PMID: 24284277.
Article11. Louw A, Puentedura EJ, Reese D, Parker P, Miller T, Mintken PE. 2017; Immediate effects of mirror therapy in patients with shoulder pain and decreased range of motion. Arch Phys Med Rehabil. 98:1941–7. DOI: 10.1016/j.apmr.2017.03.031. PMID: 28483657.
Article12. Sawyer EE, McDevitt AW, Louw A, Puentedura EJ, Mintken PE. 2018; Use of pain neuroscience education, tactile discrimination, and graded motor imagery in an individual with frozen shoulder. J Orthop Sports Phys Ther. 48:174–84. DOI: 10.2519/jospt.2018.7716. PMID: 29257926.
Article13. Manisha U, Kumar SP, Manu G. 2014; Graded motor imagery program - a review. Indian J Med Health Sci. 1:59–66. https://rfppl.co.in/view_abstract.php?jid=41&art_id=1811.14. Moseley GL. 2006; Graded motor imagery for pathologic pain: a randomized controlled trial. Neurology. 67:2129–34. DOI: 10.1212/01.wnl.0000249112.56935.32. PMID: 17082465.
Article15. Bowering KJ, O'Connell NE, Tabor A, Catley MJ, Leake HB, Moseley GL, et al. 2013; The effects of graded motor imagery and its components on chronic pain: a systematic review and meta-analysis. J Pain. 14:3–13. DOI: 10.1016/j.jpain.2012.09.007. PMID: 23158879.
Article16. Dilek B, Ayhan C, Yagci G, Yakut Y. 2018; Effectiveness of the graded motor imagery to improve hand function in patients with distal radius fracture: a randomized controlled trial. J Hand Ther. 31:2–9.e1. DOI: 10.1016/j.jht.2017.09.004. PMID: 29122370.
Article17. Anderson B, Meyster V. 2018; Treatment of a patient with central pain sensitization using graded motor imagery principles: a case report. J Chiropr Med. 17:264–7. DOI: 10.1016/j.jcm.2018.05.004. PMID: 30846919. PMCID: PMC6391225.
Article18. Hayes K, Walton JR, Szomor ZR, Murrell GA. 2001; Reliability of five methods for assessing shoulder range of motion. Aust J Physiother. 47:289–94. DOI: 10.1016/S0004-9514(14)60274-9. PMID: 11722295.
Article19. Norkin CC, White DJ. 2016. Measurement of joint motion: a guide to goniometry. 5th ed. FA Davis;Philadelphia: p. 45–56. https://www.worldcat.org/title/measurement-of-joint-motion-a-guide-to-goniometry/oclc/965327541?referer=br&ht=edition.20. Hawker GA, Mian S, Kendzerska T, French M. 2011; Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 63 Suppl 11:S240–52. DOI: 10.1002/acr.20543. PMID: 22588748.21. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. 2008; Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res. 31:165–9. DOI: 10.1097/MRR.0b013e3282fc0f93. PMID: 18467932.
Article22. Tveitå EK, Ekeberg OM, Juel NG, Bautz-Holter E. 2008; Responsiveness of the shoulder pain and disability index in patients with adhesive capsulitis. BMC Musculoskelet Disord. 9:161. DOI: 10.1186/1471-2474-9-161. PMID: 19055757. PMCID: PMC2633286.
Article23. Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. 1991; Development of a shoulder pain and disability index. Arthritis Care Res. 4:143–9. DOI: 10.1002/art.1790040403. PMID: 11188601.
Article24. Panchal DN, Eapen C. 2015; Effectiveness of end-range mobilization and interferential current or stretching exercise and moist heat in treatment of frozen shoulder- a randomized clinical trial. Int J Curr Res Rev. 7:21–6. http://eprints.manipal.edu/143690/.25. Kumar A, Kumar S, Aggarwal A, Kumar R, Das PG. 2012; Effectiveness of Maitland techniques in idiopathic shoulder adhesive capsulitis. ISRN Rehabil. 2012:710235. https://www.hindawi.com/journals/isrn/2012/710235/. DOI: 10.5402/2012/710235.
Article26. Gurudut P, Jaiswal R. 2020; Comparative effect of graded motor imagery and progressive muscle relaxation on mobility and function in patients with knee osteoarthritis: a pilot study. Altern Ther Health Med. AT6436. PMID: 33128533.27. Priganc VW, Stralka SW. 2011; Graded motor imagery. J Hand Ther. 24:164–8. DOI: 10.1016/j.jht.2010.11.002. PMID: 21306870.
Article28. Luque-Suarez A, Martinez-Calderon J, Navarro-Ledesma S, Morales-Asencio JM, Meeus M, Struyf F. 2020; Kinesiophobia is associated with pain intensity and disability in chronic shoulder pain: a cross-sectional study. J Manipulative Physiol Ther. 43:791–8. DOI: 10.1016/j.jmpt.2019.12.009. PMID: 32829946.
Article29. Yap BWD, Lim ECW. 2019; The effects of motor imagery on pain and range of motion in musculoskeletal disorders: a systematic review using meta-analysis. Clin J Pain. 35:87–99. DOI: 10.1097/AJP.0000000000000648. PMID: 30222613.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effect of graded motor imagery training on pain, functional performance, motor imagery skills, and kinesiophobia after total knee arthroplasty: randomized controlled trial
- Motor Imagery and Action Observation
- Efficacy of Low Frequency Stimulator in Patients with Frozen Shoulder
- Facilitation of Corticospinal Excitability According to Motor Imagery and Mirror Therapy in Healthy Subjects and Stroke Patients
- Comparison of Suprascapular Nerve Block and Shoulder Joint Injection for Treatment of Frozen Shoulder