Clin Endosc.
2022 Mar;55(2):287-291. 10.5946/ce.2020.272.
Acute Liver Failure Secondary to Hepatic Infiltration of Malignant Melanoma
- Affiliations
-
- 1Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea
- KMID: 2527574
- DOI: http://doi.org/10.5946/ce.2020.272
Abstract
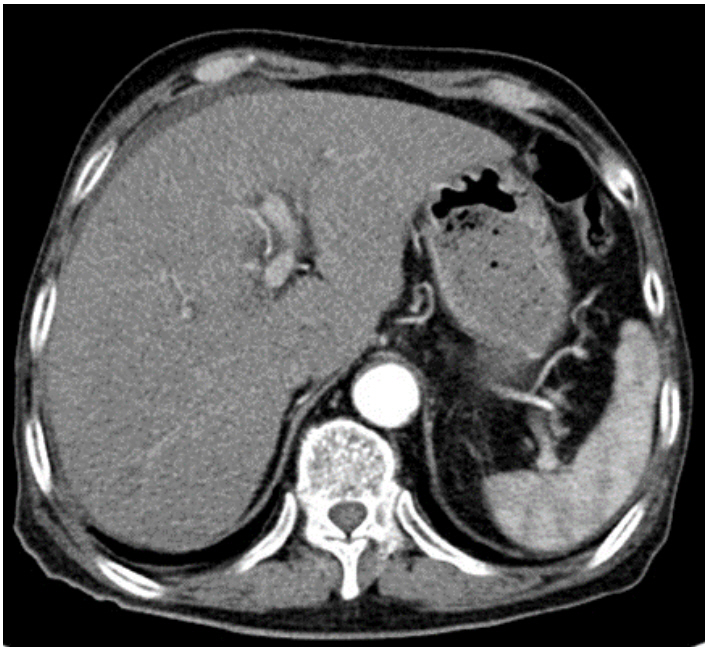
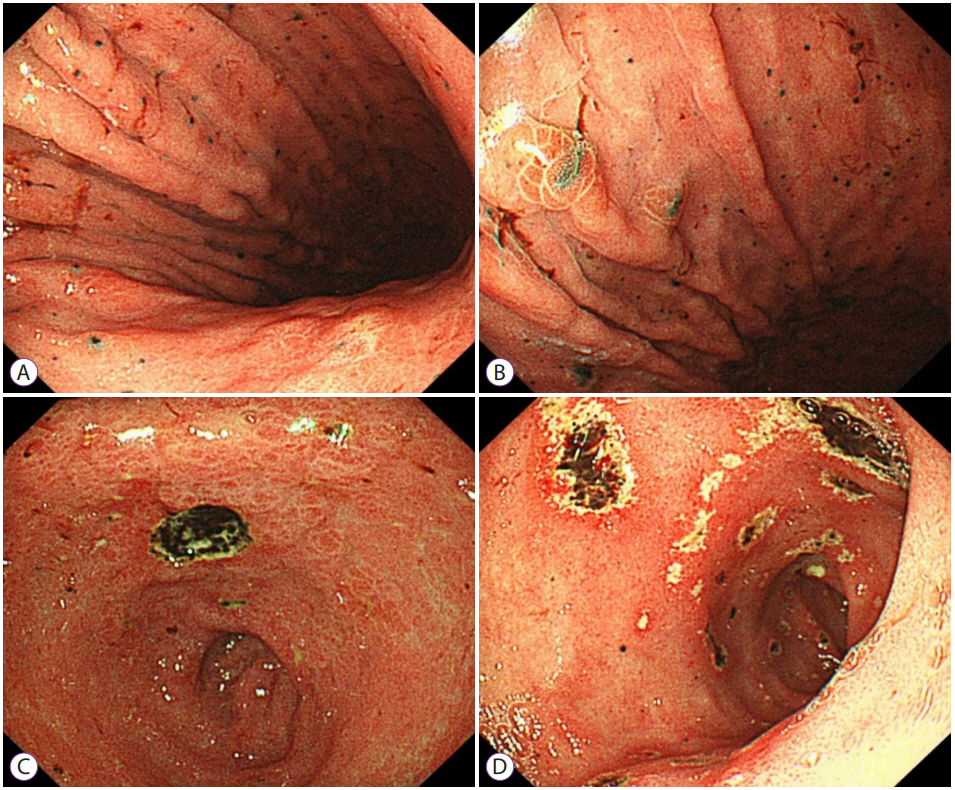
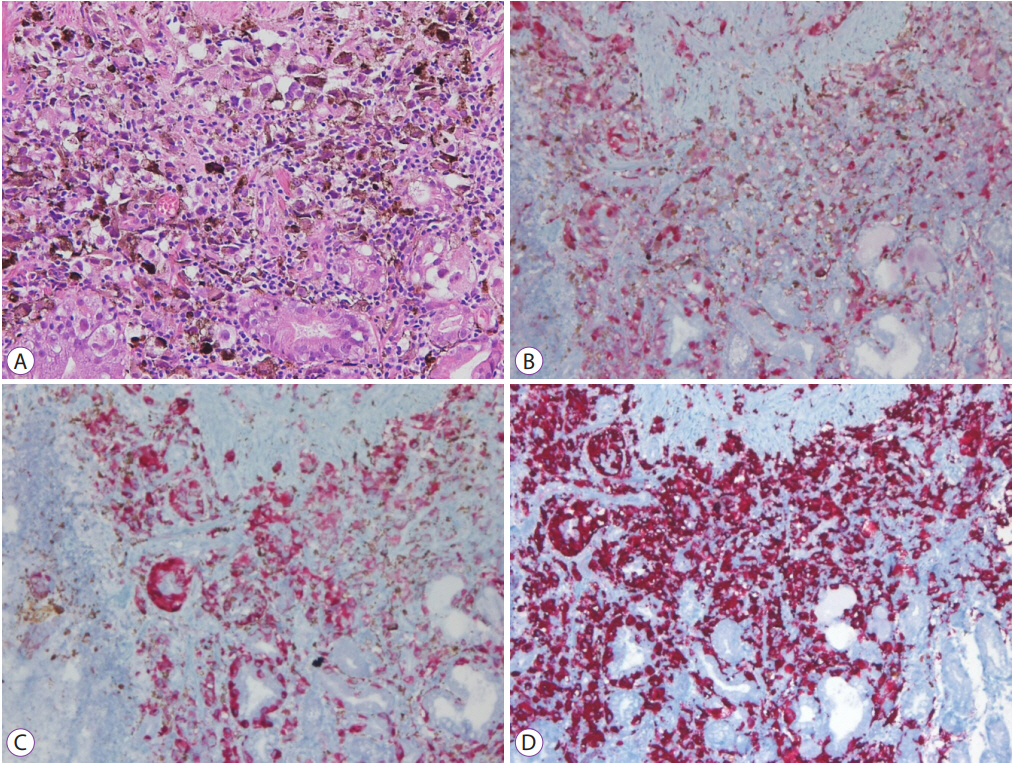
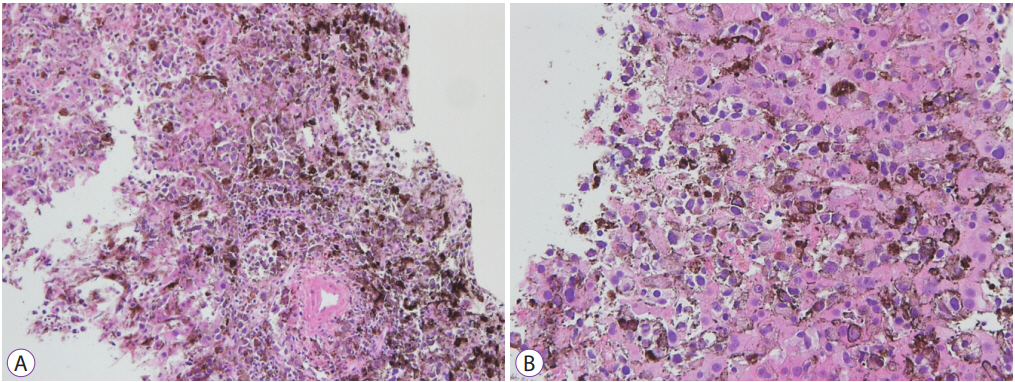
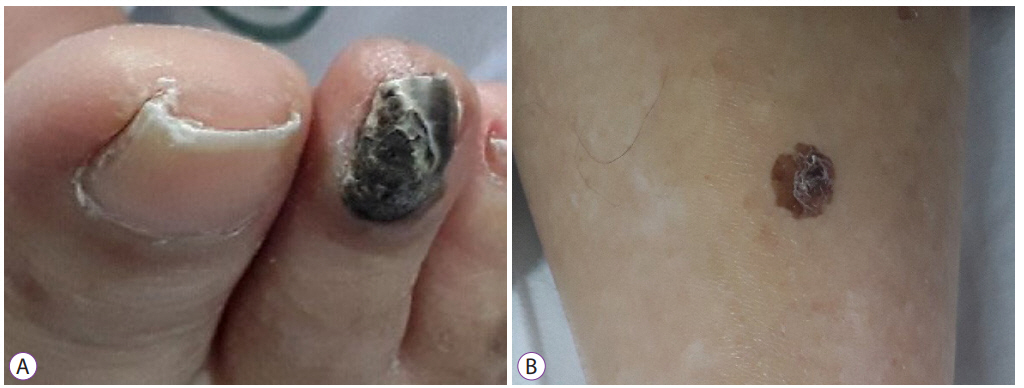
- Acute liver failure due to malignant melanoma is uncommon. We presents a case of acute liver failure secondary to hepatic infiltration of a malignant melanoma. An 86-year-old man was admitted with elevated liver enzymes and an increased lactate dehydrogenase level. His condition progressed to acute liver failure, but the etiology of liver failure was unclear. Esophagogastroduodenoscopy was performed to evaluate dyspepsia, which showed signs indicative of malignant melanoma. Based on the endoscopy findings and elevated liver enzyme levels, liver biopsy was performed to confirm the presence of malignant melanoma. Hepatic infiltration of malignant melanoma was observed histologically. However, massive and diffuse liver metastasis is very rare and difficult to identify on imaging studies. If the etiology of liver failure is unclear, diffuse metastatic melanoma infiltration should be considered as differential diagnosis. Early liver biopsy can help to clarify the diagnosis.
Figure
Reference
-
1. Curti BD, Leachman S, Urba WJ. Cancer of the Skin. In: Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, eds. Harrison’s principles of internal medicine 20th ed. New York (NY): McGraw-Hill Education; 2018. p. 522-530.2. Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998; 83:1664–1678.3. Dasgupta T, Bowden L, Berg JW. Malignant melanoma of unknown primary origin. Surg Gynecol Obste. 1963; 117:341–345.4. Rose DM, Essner R, Hughes TM, et al. Surgical resection for metastatic melanoma to the liver: the John Wayne Cancer Institute and Sydney Melanoma Unit experience. Arch Surg. 2001; 136:950–955.5. Te HS, Schiano TD, Kahaleh M, et al. Fulminant hepatic failure secondary to malignant melanoma: case report and review of the literature. Am J Gastroenterol. 1999; 94:262–266.6. Montero JL, Muntané J, de las Heras S, Ortega R, Fraga E, De la Mata M. Acute liver failure caused by diffuse hepatic melanoma infiltration. J Hepatol. 2002; 37:540–541.7. Schlevogt B, Rehkämper J, Hild B, Schmidt HH. Hepatobiliary and pancreatic: fulminant liver failure from diffuse leukemoid hepatic infiltration of melanoma. J Gastroenterol Hepatol. 2017; 32:1795.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Fulminant Hepatic Failure Secondary to Hepatic Metastasis of Small Cell Lung Carcinoma
- A Case of Metastatic Malignant Melanoma of the Liver Resulting from Choroidal Melanoma
- Acute Hepatic Failure after Spinal Surgery in Patient with Liver Cirrhosis: A case report
- Primary malignant melanoma of the esophagus
- Three Cases of Fulminant Hepatic Failure due to Congestive Heart Failure