Clin Endosc.
2022 Mar;55(2):197-207. 10.5946/ce.2021.079.
Confocal Laser Endomicroscopy in the Diagnosis of Biliary and Pancreatic Disorders: A Systematic Analysis
- Affiliations
-
- 1Universidad Francisco Marroquin, School of Medicine, Guatemala City, Guatemala
- 2Division of Gastroenterology, Hepatology, and Nutrition, The Ohio State University Wexner Medical Center, Columbus, Ohio, USA
- 3Division of Gastroenterology and Hepatology, MD Anderson Cancer Center, Houston, Texas, USA
- 4Division of Gastroenterology and Hepatology, Mayo Clinic, Jacksonville, Florida, USA
- 5Division of Gastroenterology and Hepatology, Presbyterian Health Services, Albuquerque, New Mexico, USA
- KMID: 2527561
- DOI: http://doi.org/10.5946/ce.2021.079
Abstract
- Background/Aims
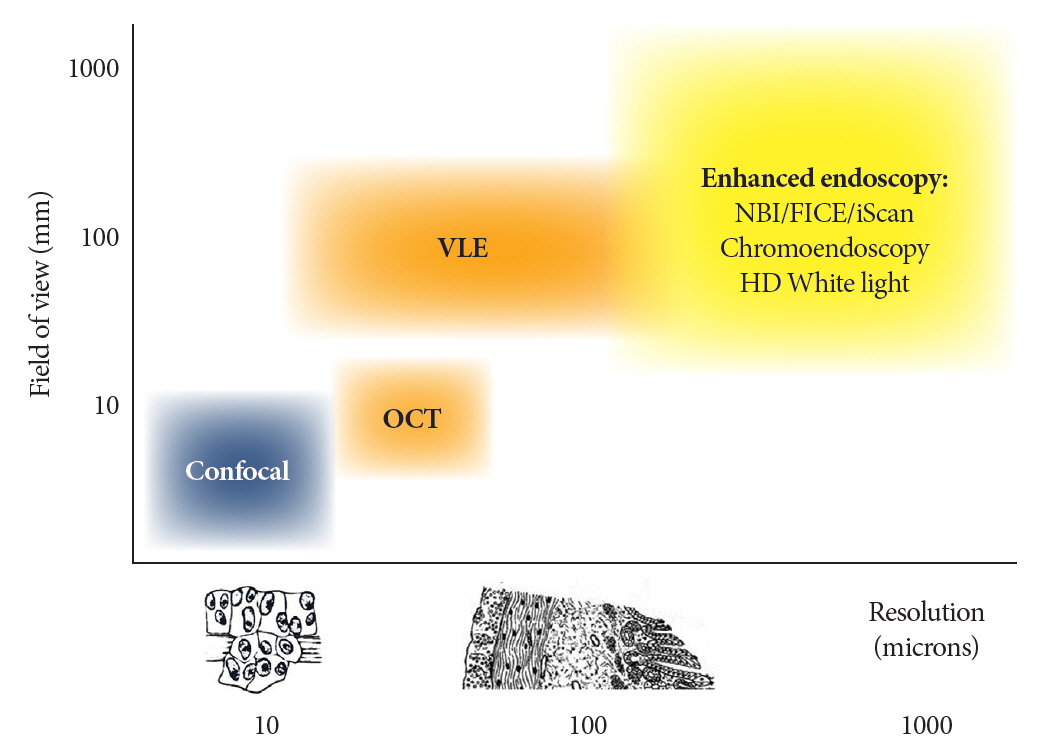
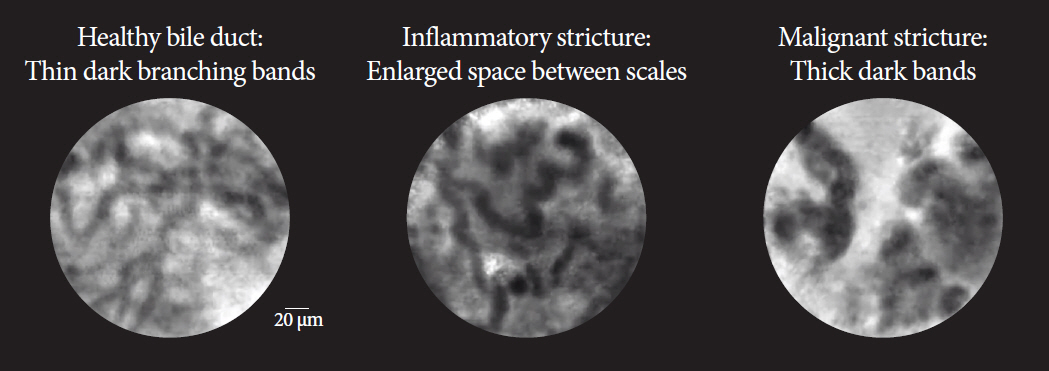
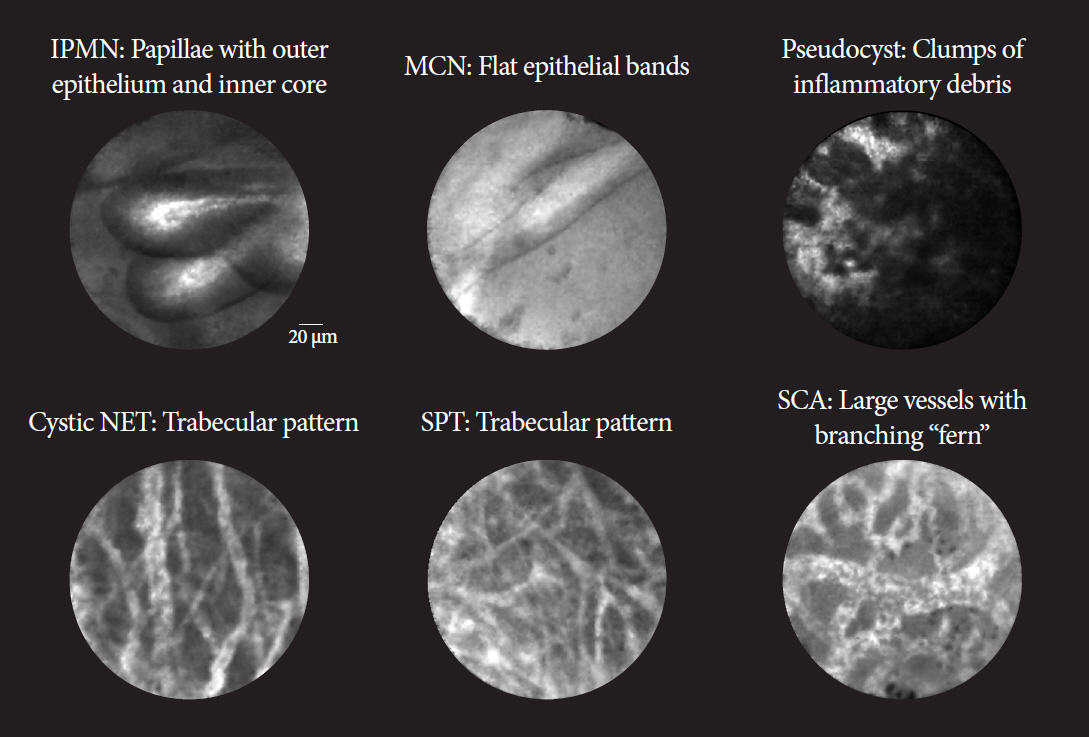
Endoscopic visualization of the microscopic anatomy can facilitate the real-time diagnosis of pancreatobiliary disorders and provide guidance for its treatment. This study aimed to review the technique, image classification, and diagnostic performance of confocal laser endomicroscopy (CLE).
Methods
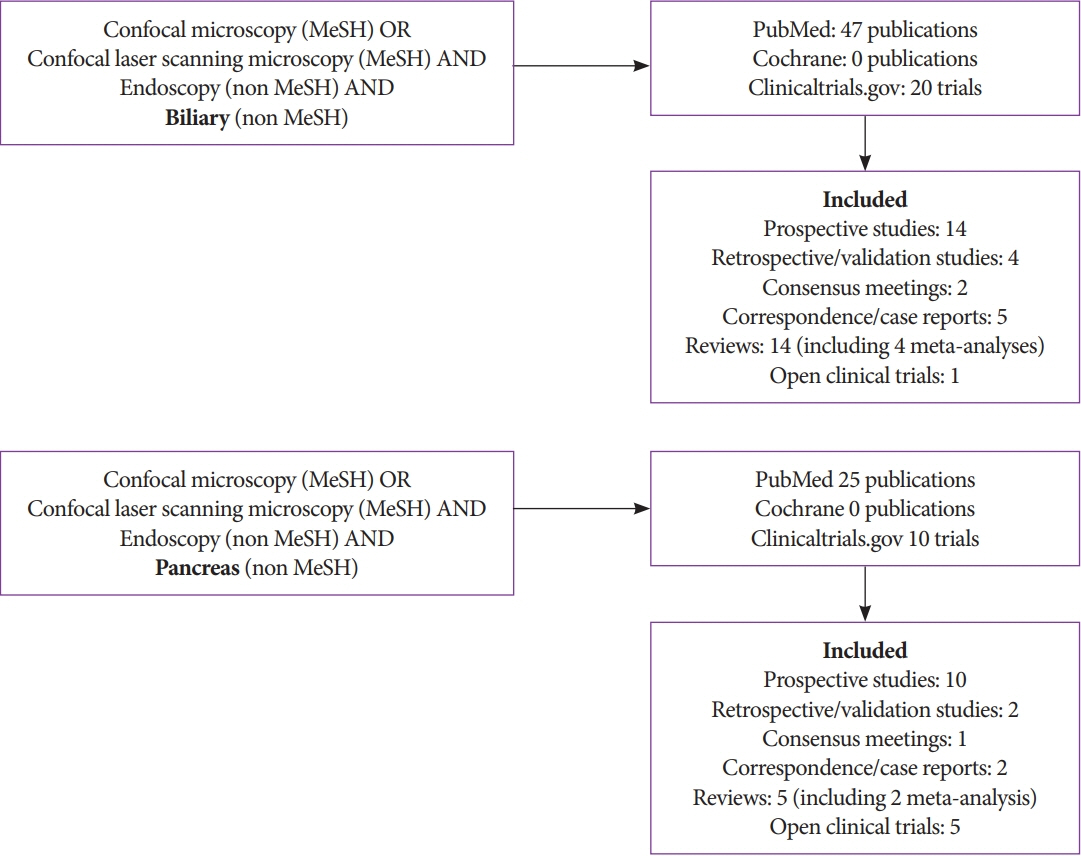
We conducted a systematic review of CLE in pancreatic and biliary ducts of humans, and have provided a narrative of the technique, image classification, diagnostic performance, ongoing research, and limitations.
Results
Probe-based CLE differentiates malignant from benign biliary strictures (sensitivity, ≥89%; specificity, ≥61%). Needlebased CLE differentiates mucinous from non-mucinous pancreatic cysts (sensitivity, 59%; specificity, ≥94%) and identifies dysplasia. Pancreatitis may develop in 2-7% of pancreatic cyst cases. Needle-based CLE has potential applications in adenocarcinoma, neuroendocrine tumors, and pancreatitis (chronic or autoimmune). Costs, catheter lifespan, endoscopist training, and interobserver variability are challenges for routine utilization.
Conclusions
CLE reveals microscopic pancreatobiliary system anatomy with adequate specificity and sensitivity. Reducing costs and simplifying image interpretation will promote utilization by advanced endoscopists.
Figure
Reference
-
1. Kochhar G, Wallace MB. Virtual histology in everyday gastrointestinal endoscopy. Clin Gastroenterol Hepatol. 2018; 16:1556–1561.2. Trindade AJ, Leggett CL, Chang KJ. Volumetric laser endomicroscopy in the management of Barrett’s esophagus. Curr Opin Gastroenterol. 2017; 33:254–260.3. Al-Mansour MR, Caycedo-Marulanda A, Davis BR, et al. SAGES TAVAC safety and efficacy analysis confocal laser endomicroscopy. Surg Endosc. 2021; 35:2091–2103.4. Glover B, Teare J, Patel N. The status of advanced imaging techniques for optical biopsy of colonic polyps. Clin Transl Gastroenterol. 2020; 11:e00130.5. Ruff S, Curtin B, Quezado M, et al. Evaluation of confocal endoscopic microscopy for detection of early-stage gastric cancer in hereditary diffuse gastric cancer (HDGC) syndrome. J Gastrointest Oncol. 2019; 10:407–411.6. Su P, Liu Y, Lin S, et al. Efficacy of confocal laser endomicroscopy for discriminating colorectal neoplasms from non-neoplasms: a systematic review and meta-analysis. Colorectal Dis. 2013; 15:e1–e12.7. Yu X, Chen J, Zheng L, Song J, Lin R, Hou X. Quantitative diagnosis of atrophic gastritis by probe-based confocal laser endomicroscopy. Biomed Res Int. 2020; 2020:9847591.8. Buchner AM. Confocal laser endomicroscopy in the evaluation of inflammatory bowel disease. Inflamm Bowel Dis. 2019; 25:1302–1312.9. Zhang MM, Zhong N, Wang X, et al. Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for diagnosis of gastric subepithelial tumors: a pilot study. Endoscopy. 2019; 51:560–565.10. Pohl H, Tanczos BT, Rudolph B, et al. Probe-based confocal laser microscopy identifies criteria predictive of active celiac sprue. Dig Dis Sci. 2012; 57:451–457.11. Cellvizio® Gastrointestinal Brochure - International [Internet]. Paris: Mauna Kea Technologies; c2016 [cited 2021 June 25]. Available from: https://www.maunakeatech.com/en/researchers/32-brochure.12. Saadi M, Yu C, Othman MO. A review of the challenges associated with the diagnosis and therapy of primary sclerosing cholangitis. J Clin Transl Hepatol. 2014; 2:45–52.13. Hutchins GF, Draganov PV. Cystic neoplasms of the pancreas: a diagnostic challenge. World J Gastroenterol. 2009; 15:48–54.14. Gao YD, Qu YW, Liu HF. Comparison of diagnostic efficacy between CLE, tissue sampling, and CLE combined with tissue sampling for undetermined pancreaticobiliary strictures: a meta-analysis. Scand J Gastroenterol. 2018; 53:482–489.15. Facciorusso A, Buccino VR, Sacco R. Needle-based confocal laser endomicroscopy in pancreatic cysts: a meta-analysis. Eur J Gastroenterol Hepatol. 2020; 32:1084–1090.16. Njei B, McCarty TR, Varadarajulu S, Navaneethan U. Systematic review with meta-analysis: endoscopic retrograde cholangiopancreatography-based modalities for the diagnosis of cholangiocarcinoma in primary sclerosing cholangitis. Aliment Pharmacol Ther. 2016; 44:1139–1151.17. Liu Y, Lu Y, Sun B, et al. Probe-based confocal laser endomicroscopy for the diagnosis of undetermined biliary stenoses: a meta-analysis. Clin Res Hepatol Gastroenterol. 2016; 40:666–673.18. Fugazza A, Gaiani F, Carra MC, et al. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases: a systematic review and meta-analysis. Biomed Res Int. 2016; 2016:4638683.19. Konjeti VR, McCarty TR, Rustagi T. Needle-based confocal laser endomicroscopy (nCLE) for evaluation of pancreatic cystic lesions: a systematic review and meta-analysis. J Clin Gastroenterol. 2020; Nov. 25. [Epub]. https://doi.org/10.1097/MCG.0000000000001468.20. Peter S, Council L, Bang JY, et al. Poor agreement between endoscopists and gastrointestinal pathologists for the interpretation of probe-based confocal laser endomicroscopy findings. World J Gastroenterol. 2014; 20:17993–18000.21. Luthra AK, Pusateri AJ, Pfeil SA, et al. Confocal laser endomicroscopy interpretation and differentiation of pancreatic cysts: a randomized trial of teaching modalities. Techniques and Innovations in Gastrointestinal Endoscopy. 2021; 23:8–17.22. Gerhards MF, Vos P, van Gulik TM, Rauws EA, Bosma A, Gouma DJ. Incidence of benign lesions in patients resected for suspicious hilar obstruction. Br J Surg. 2001; 88:48–51.23. Shah RJ, Langer DA, Antillon MR, Chen YK. Cholangioscopy and cholangioscopic forceps biopsy in patients with indeterminate pancreaticobiliary pathology. Clin Gastroenterol Hepatol. 2006; 4:219–225.24. Meining A, Chen YK, Pleskow D, et al. Direct visualization of indeterminate pancreaticobiliary strictures with probe-based confocal laser endomicroscopy: a multicenter experience. Gastrointest Endosc. 2011; 74:961–968.25. Wallace M, Lauwers GY, Chen Y, et al. Miami classification for probebased confocal laser endomicroscopy. Endoscopy. 2011; 43:882–891.26. Caillol F, Filoche B, Gaidhane M, Kahaleh M. Refined probe-based confocal laser endomicroscopy classification for biliary strictures: the Paris Classification. Dig Dis Sci. 2013; 58:1784–1789.27. Wang KK, Carr-Locke DL, Singh SK, et al. Use of probe-based confocal laser endomicroscopy (pCLE) in gastrointestinal applications. A consensus report based on clinical evidence. United European Gastroenterol J. 2015; 3:230–254.28. ASGE Standards of Practice Committee, Chathadi KV, Chandrasekhara V, et al. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc. 2015; 81:795–803.29. Tringali A, Lemmers A, Meves V, et al. Intraductal biliopancreatic imaging: european society of gastrointestinal endoscopy (ESGE) technology review. Endoscopy. 2015; 47:739–753.30. Heif M, Yen RD, Shah RJ. ERCP with probe-based confocal laser endomicroscopy for the evaluation of dominant biliary stenoses in primary sclerosing cholangitis patients. Dig Dis Sci. 2013; 58:2068–2074.31. Caillol F, Bories E, Autret A, et al. Evaluation of pCLE in the bile duct: final results of EMID study : pCLE: impact in the management of bile duct strictures. Surg Endosc. 2015; 29:2661–2668.32. Slivka A, Gan I, Jamidar P, et al. Validation of the diagnostic accuracy of probe-based confocal laser endomicroscopy for the characterization of indeterminate biliary strictures: results of a prospective multicenter international study. Gastrointest Endosc. 2015; 81:282–290.33. Dubow M, Tatman PD, Shah RJ. Individual probe based confocal laser endomicroscopy criteria in the analysis of indeterminate biliary strictures. Scand J Gastroenterol. 2018; 53:1358–1363.34. Koda H, Hara K, Nozomi O, et al. High-resolution probe-based confocal laser endomicroscopy for diagnosing biliary diseases. Clin Endosc. 2021; Mar. 15. [Epub]. https://doi.org/doi: 10.5946/ce.2020.191.35. Konda VJA, Meining A, Jamil LH, et al. A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy. 2013; 45:1006–1013.36. Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 2015; 81:1204–1214.37. Napoléon B, Lemaistre A-I, Pujol B, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy. 2015; 47:26–32.38. Krishna SG, Hart PA, Malli A, et al. Endoscopic ultrasound-guided confocal laser endomicroscopy increases accuracy of differentiation of pancreatic cystic lesions. Clin Gastroenterol Hepatol. 2020; 18:432–440.e6.39. Keane MG, Wehnert N, Perez-Machado M, et al. A prospective trial of CONfocal endomicroscopy in CYSTic lesions of the pancreas: CONCYST-01. Endosc Int Open. 2019; 7:E1117–E1122.40. Krishna SG, Hart PA, DeWitt JM, et al. EUS-guided confocal laser endomicroscopy: prediction of dysplasia in intraductal papillary mucinous neoplasms (with video). Gastrointest Endosc. 2020; 91:551–563.e5.41. Hao S, Ding W, Jin Y, et al. Appraisal of EUS-guided needle-based confocal laser endomicroscopy in the diagnosis of pancreatic lesions: a single Chinese center experience. Endosc Ultrasound. 2020; 9:180–186.42. Chin YK, Wu CCH, Tan DMY. The role of needle-based confocal laser endomicroscopy in the evaluation of pancreatic cystic lesions: a systematic review. Clin Endosc. 2021; 54:38–47.43. Giovannini M, Caillol F, Monges G, et al. Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy in solid pancreatic masses. Endoscopy. 2016; 48:892–898.44. Orr J, Lockwood R, Roberts J, Shi C, Yachimski P. EUS and confocal endomicroscopic diagnosis of pancreatic acinar cell cystadenoma. Gastrointest Endosc. 2018; 88:769–770.45. ASGE Standards of Practice Committee, Muthusamy VR, Chandrasekhara V, et al. The role of endoscopy in the diagnosis and treatment of cystic pancreatic neoplasms. Gastrointest Endosc. 2016; 84:1–9.46. European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67:789–804.47. Larghi A, Crinò SF, Napoleon B. Pancreatic cystic lesions: time to move to 19-gauge needle with EUS-guided microforceps biopsy or needle-based confocal laser endomicroscopy. Gastrointest Endosc. 2020; 92:222.48. Bhutani MS, Koduru P, Joshi V, et al. EUS-guided needle-based confocal laser endomicroscopy: a novel technique with emerging applications. Gastroenterol Hepatol (N Y). 2015; 11:235–240.49. Yang D, Samarasena JB, Jamil LH, et al. Endoscopic ultrasound-guided through-the-needle microforceps biopsy in the evaluation of pancreatic cystic lesions: a multicenter study. Endosc Int Open. 2018; 6:E1423–E1430.50. Karia K, Waxman I, Konda VJ, et al. Needle-based confocal endomicroscopy for pancreatic cysts: the current agreement in interpretation. Gastrointest Endosc. 2016; 83:924–927.51. Talreja JP, Sethi A, Jamidar PA, et al. Interpretation of probe-based confocal laser endomicroscopy of indeterminate biliary strictures: is there any interobserver agreement? Dig Dis Sci. 2012; 57:3299–3302.52. Aubreville M, Stoeve M, Oetter N, et al. Deep learning-based detection of motion artifacts in probe-based confocal laser endomicroscopy images. Int J Comput Assist Radiol Surg. 2019; 14:31–42.53. Rasti P, Wolf C, Dorez H, et al. Machine learning-based classification of the health state of mice colon in cancer study from confocal laser endomicroscopy. Sci Rep. 2019; 9:20010.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Probe-Based Confocal Laser Endomicroscopy for Pancreaticobiliary Disease
- High-Resolution Probe-Based Confocal Laser Endomicroscopy for Diagnosing Biliary Diseases
- The Role of Needle-Based Confocal Laser Endomicroscopy in the Evaluation of Pancreatic Cystic Lesions: A Systematic Review
- The role of needle-based confocal laser endomicroscopy in the diagnosis of pancreatic neuroendocrine tumors
- Confocal Laser Endomicroscopy and Molecular Imaging in Barrett Esophagus and Stomach