Clin Endosc.
2021 Jan;54(1):38-47. 10.5946/ce.2019.200-IDEN.
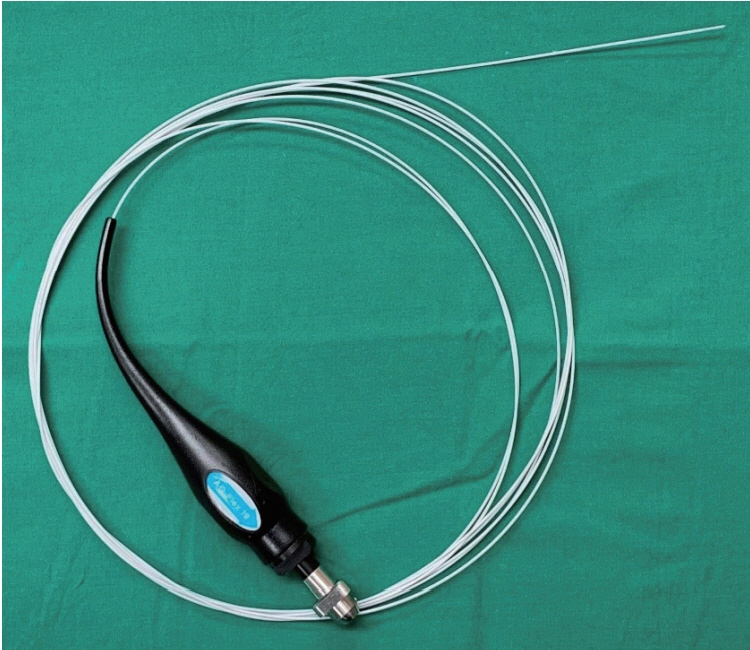
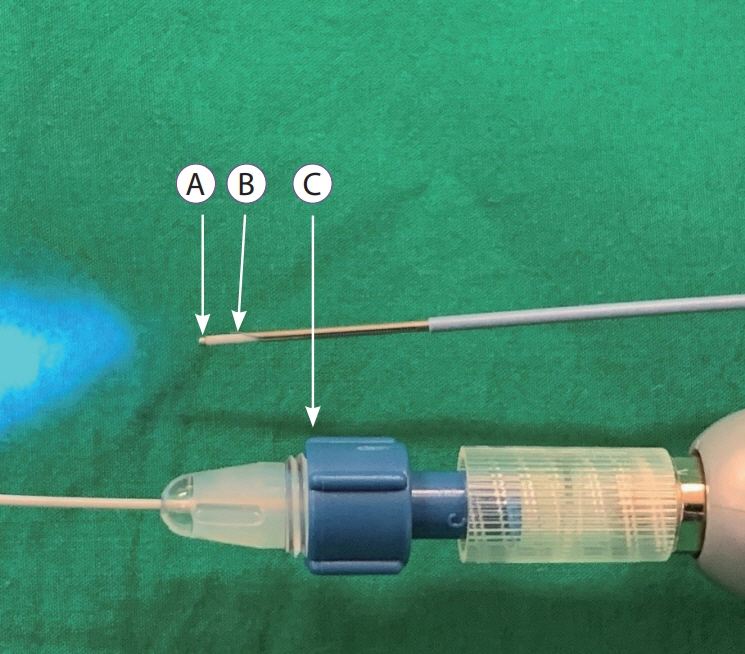
The Role of Needle-Based Confocal Laser Endomicroscopy in the Evaluation of Pancreatic Cystic Lesions: A Systematic Review
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore
- 2Duke-NUS Medical School, Singapore, Singapore
- KMID: 2512308
- DOI: http://doi.org/10.5946/ce.2019.200-IDEN
Abstract
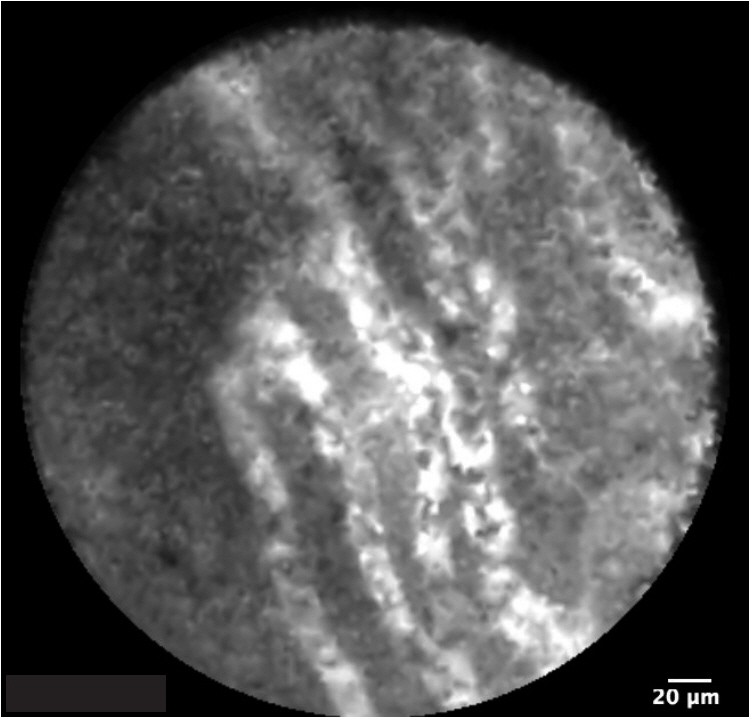
- The prevalence of pancreatic cystic lesions (PCLs) has increased recently due to the increased use of cross-sectional abdominal imaging and the ageing global population. Current diagnostic techniques are inadequate to distinguish between PCLs that require surgery, close surveillance, or expectant management. This has resulted in increased morbidity from both inappropriately aggressive and conservative management strategies. Needle-based confocal laser endomicroscopy (nCLE) has allowed microscopic examination and visual delineation of the surface epithelium of PCLs. Landmark studies in this decade have correlated nCLE and histological findings and identified characteristics differentiating various types of PCLs. Subsequent studies have confirmed the high diagnostic yield of nCLE and its diagnostic utility in PCLs with an equivocal diagnosis. Moreover, nCLE has been shown to improve the diagnostic yield of PCLs. This will help avoid unnecessary pancreatic surgery, which carries significant morbidity and mortality risks. The early detection of high-grade dysplasia in PCLs will provide early surgical treatment and improve outcomes for pancreatic cancer. Despite the high upfront cost of nCLE, the improved diagnostic accuracy and resultant appropriate management have resulted in improved cost effectiveness. Refining the procedure technique and limiting the procedure length have significantly improved the safety of nCLE. A structured training program and device improvements to allow more complete mapping of the pancreatic cyst epithelium will be crucial for the widespread adoption of this promising technology.
Keyword
Figure
Reference
-
1. Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008; 191:802–807.
Article2. de Jong K, Bruno MJ, Fockens P. Epidemiology, diagnosis, and management of cystic lesions of the pancreas. Gastroenterol Res Pract. 2012; 2012:147465.
Article3. de Jong K, Nio CY, Hermans JJ, et al. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 2010; 8:806–811.
Article4. Nougaret S, Mannelli L, Pierredon MA, Schembri V, Guiu B. Cystic pancreatic lesions: from increased diagnosis rate to new dilemmas. Diagn Interv Imaging. 2016; 97:1275–1285.
Article5. Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology. 2006; 6:17–32.
Article6. Khalid A, Brugge W. ACG practice guidelines for the diagnosis and management of neoplastic pancreatic cysts. Am J Gastroenterol. 2007; 102:2339–2349.
Article7. Goh BK, Tan YM, Cheow PC, et al. Cystic lesions of the pancreas: an appraisal of an aggressive resectional policy adopted at a single institution during 15 years. Am J Surg. 2006; 192:148–154.
Article8. Karim SAM, Abdulla KS, Abdulkarim QH, Rahim FH. The outcomes and complications of pancreaticoduodenectomy (Whipple procedure): cross sectional study. Int J Surg. 2018; 52:383–387.
Article9. Wang J, Ma R, Churilov L, et al. The cost of perioperative complications following pancreaticoduodenectomy: a systematic review. Pancreatology. 2018; 18:208–220.
Article10. Elta GH, Enestvedt BK, Sauer BG, Lennon AM. ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 2018; 113:464–479.
Article11. Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.
Article12. European Study Group on Cystic Tumours of the PancreaM. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67:789–804.13. Hutchins GF, Draganov PV. Cystic neoplasms of the pancreas: a diagnostic challenge. World J Gastroenterol. 2009; 15:48–54.
Article14. Lee KH, Lee SJ, Lee JK, et al. Prediction of malignancy with endoscopic ultrasonography in patients with branch duct-type intraductal papillary mucinous neoplasm. Pancreas. 2014; 43:1306–1311.
Article15. Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004; 126:1330–1336.
Article16. Meining A. Confocal endomicroscopy. Gastrointest Endosc Clin N Am. 2009; 19:629–635.
Article17. Konda VJ, Aslanian HR, Wallace MB, Siddiqui UD, Hart J, Waxman I. First assessment of needle-based confocal laser endomicroscopy during EUS-FNA procedures of the pancreas (with videos). Gastrointest Endosc. 2011; 74:1049–1060.
Article18. Konda VJ, Meining A, Jamil LH, et al. A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy. 2013; 45:1006–1013.19. Nakai Y, Iwashita T, Park DH, Samarasena JB, Lee JG, Chang KJ. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 2015; 81:1204–1214.
Article20. Napoléon B, Lemaistre AI, Pujol B, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy. 2015; 47:26–32.
Article21. Napoleon B, Lemaistre AI, Pujol B, et al. In vivo characterization of pancreatic cystic lesions by needle-based confocal laser endomicroscopy (nCLE): proposition of a comprehensive nCLE classification confirmed by an external retrospective evaluation. Surg Endosc. 2016; 30:2603–2612.
Article22. Chin YK, Khor CJL, Goh BKP, Lim TKH, Tan DMY. The clinical evaluation of needle-based confocal laser endomicroscopy in the assessment of pancreatic cystic lesion: a pilot study. Proceedings of Singapore Healthcare. 2018; 27:96–102.
Article23. Napoleon B, Palazzo M, Lemaistre AI, et al. Needle-based confocal laser endomicroscopy of pancreatic cystic lesions: a prospective multicenter validation study in patients with definite diagnosis. Endoscopy. 2019; 51:825–835.
Article24. Keane MG, Wehnert N, Perez-Machado M, et al. A prospective trial of CONfocal endomicroscopy in CYSTic lesions of the pancreas: CONCYST-01. Endosc Int Open. 2019; 7:E1117–E1122.
Article25. Karia K, Waxman I, Konda VJ, et al. Needle-based confocal endomicroscopy for pancreatic cysts: the current agreement in interpretation. Gastrointest Endosc. 2016; 83:924–927.
Article26. Kadayifci A, Atar M, Basar O, Forcione DG, Brugge WR. Needle-based confocal laser endomicroscopy for evaluation of cystic neoplasms of the pancreas. Dig Dis Sci. 2017; 62:1346–1353.
Article27. Krishna SG, Swanson B, Hart PA, et al. Validation of diagnostic characteristics of needle based confocal laser endomicroscopy in differentiation of pancreatic cystic lesions. Endosc Int Open. 2016; 4:E1124–E1135.
Article28. Krishna SG, Brugge WR, Dewitt JM, et al. Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions: an international external interobserver and intraobserver study (with videos). Gastrointest Endosc. 2017; 86:644–654.e2.
Article29. Krishna SG, Hart PA, DeWitt JM, et al. EUS-guided confocal laser endomicroscopy: prediction of dysplasia in intraductal papillary mucinous neoplasms (with video). Gastrointest Endosc. 2020; 91:551–563.e5.
Article30. Palazzo M, Sauvanet A, Gincul R, et al. Impact of needle-based confocal laser endomicroscopy on the therapeutic management of single pancreatic cystic lesions. Surg Endosc. 2019; Aug. 13. [Epub]. https://doi.org/10.1007/s00464-019-07062-9.
Article31. Alvarez-Sánchez MV, Napoléon B. New horizons in the endoscopic ultrasonography-based diagnosis of pancreatic cystic lesions. World J Gastroenterol. 2018; 24:2853–2866.
Article32. Le Pen C, Palazzo L, Napoléon B. A health economic evaluation of needle- based confocal laser endomicroscopy for the diagnosis of pancreatic cysts. Endosc Int Open. 2017; 5:E987–E995.33. Krishna SG, Swanson B, Conwell DL, Muscarella P 2nd. In vivo and ex vivo needle-based confocal endomicroscopy of intraductal papillary mucinous neoplasm of the pancreas. Gastrointest Endosc. 2015; 82:571–572.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Review of Probe-Based Confocal Laser Endomicroscopy for Pancreaticobiliary Disease
- Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for pancreatic cystic lesions: current status and future prospects
- Endoscopic Ultrasound-Based Evaluation of Pancreatic Cysts: New Invasive Modalities
- Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for diagnosis of solid pancreatic lesions
- The role of needle-based confocal laser endomicroscopy in the diagnosis of pancreatic neuroendocrine tumors