Clin Endosc.
2024 Jul;57(4):434-445. 10.5946/ce.2023.157.
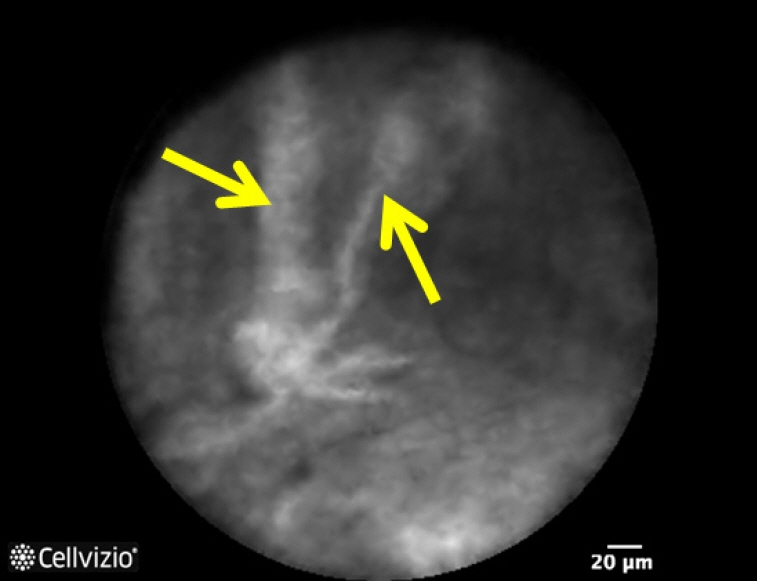
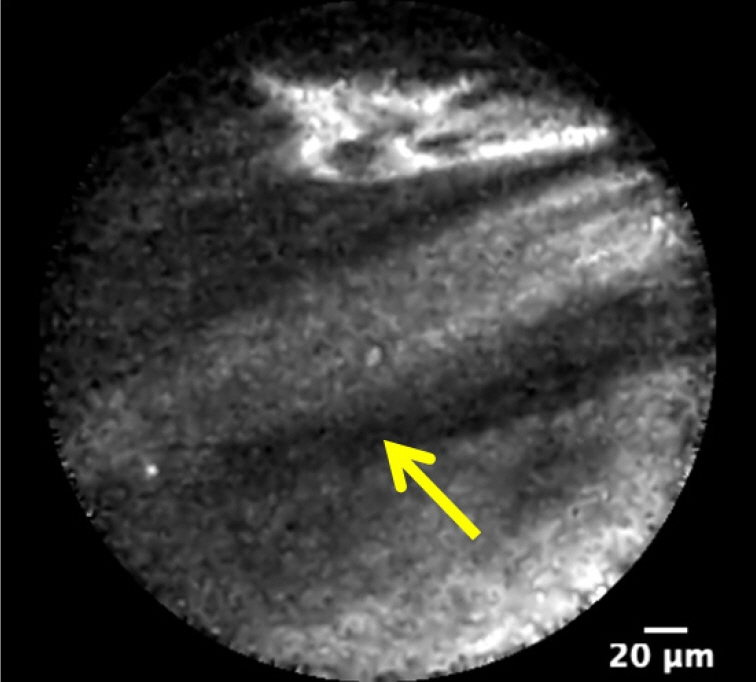
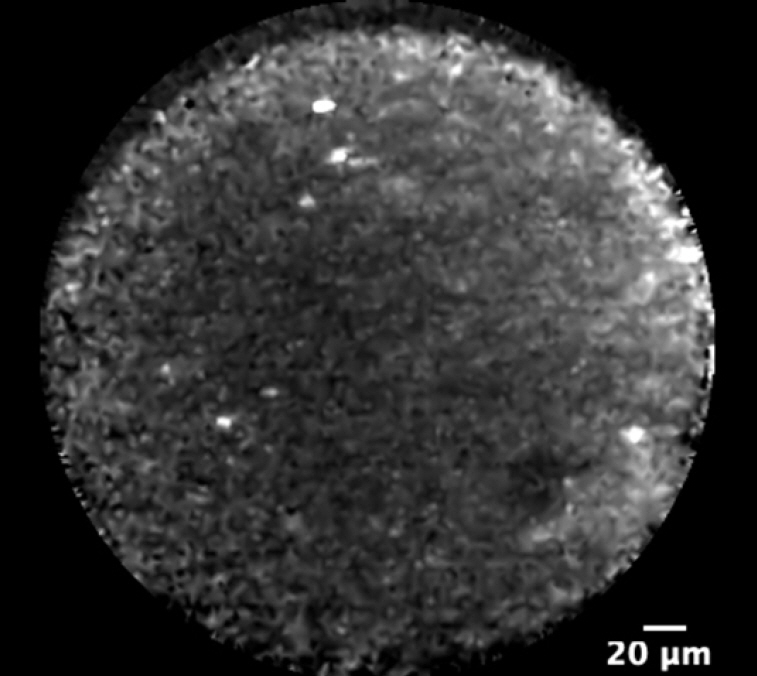
Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for pancreatic cystic lesions: current status and future prospects
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Singapore General Hospital, Singapore
- 2Medicine Academic Clinical Programme (MedACP), Duke-NUS Medical School, Singapore, Singapore
- KMID: 2558097
- DOI: http://doi.org/10.5946/ce.2023.157
Abstract
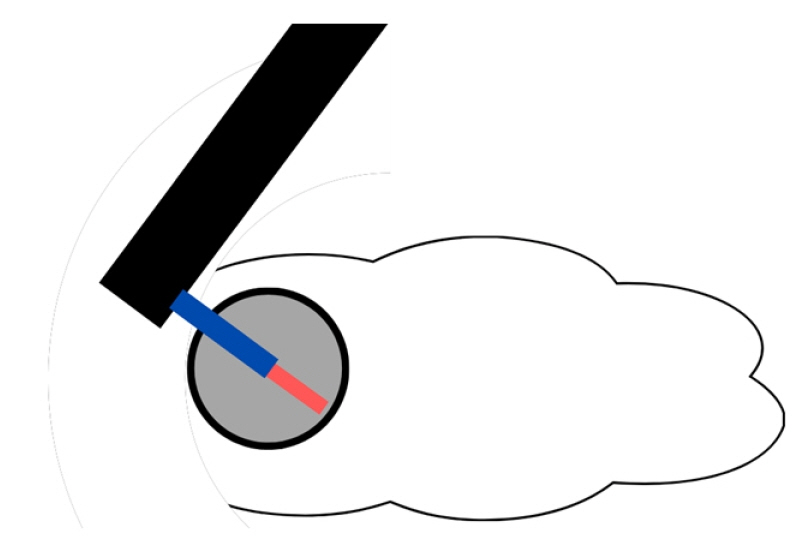
- Pancreatic cystic lesions (PCLs) have increased in prevalence due to the increased usage and advancements in cross-sectional abdominal imaging. Current diagnostic techniques cannot distinguish between PCLs requiring surgery, close surveillance, or expectant management. This has increased the morbidity and healthcare costs from inappropriately aggressive and conservative management strategies. Endoscopic ultrasound (EUS) needle-based confocal laser endomicroscopy (nCLE) allows for microscopic examination and delineation of the surface epithelium of PCLs. Landmark studies have identified characteristics distinguishing various types of PCLs, confirmed the high diagnostic yield of EUS-nCLE (especially for PCLs with an equivocal diagnosis), and shown that EUS-nCLE helps to change management and reduce healthcare costs. Refining procedure technique and reducing procedure length have improved the safety of EUS-nCLE. The utilization of artificial intelligence and its combination with other EUS-based advanced diagnostic techniques would further improve the results of EUS-based PCL diagnosis. A structured training program and device improvements to allow more complete mapping of the pancreas cyst epithelium will be crucial for the widespread adoption of this promising technology.
Keyword
Figure
Reference
-
1. Park J, Park J, Lee YS, et al. Increased incidence of indeterminate pancreatic cysts and changes of management pattern: evidence from nationwide data. Hepatobiliary Pancreat Dis Int. 2023; 22:294–301.2. Moris M, Bridges MD, Pooley RA, et al. Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014. Clin Gastroenterol Hepatol. 2016; 14:585–593.
Article3. Farrell JJ. Prevalence, diagnosis and management of pancreatic cystic neoplasms: current status and future directions. Gut Liver. 2015; 9:571–589.
Article4. Laffan TA, Horton KM, Klein AP, et al. Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol. 2008; 191:802–807.
Article5. Ishikawa T, Takeda K, Itoh M, et al. Prevalence of pancreatic cystic lesions including intraductal papillary mucinous neoplasms in patients with end-stage renal disease on hemodialysis. Pancreas. 2009; 38:175–179.
Article6. Crippa S, Salvia R, Warshaw AL, et al. Mucinous cystic neoplasm of the pancreas is not an aggressive entity: lessons from 163 resected patients. Ann Surg. 2008; 247:571–579.7. Salvia R, Fernández-del Castillo C, Bassi C, et al. Main-duct intraductal papillary mucinous neoplasms of the pancreas: clinical predictors of malignancy and long-term survival following resection. Ann Surg. 2004; 239:678–687.8. Chari ST, Kelly K, Hollingsworth MA, et al. Early detection of sporadic pancreatic cancer: summative review. Pancreas. 2015; 44:693–712.9. Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014; 74:2913–2921.
Article10. Scheiman JM, Hwang JH, Moayyedi P. American Gastroenterological Association technical review on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015; 148:824–848.
Article11. Elta GH, Enestvedt BK, Sauer BG, et al. ACG clinical guideline: diagnosis and management of pancreatic cysts. Am J Gastroenterol. 2018; 113:464–479.12. Brugge WR, Lewandrowski K, Lee-Lewandrowski E, et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004; 126:1330–1336.
Article13. Brandwein SL, Farrell JJ, Centeno BA, et al. Detection and tumor staging of malignancy in cystic, intraductal, and solid tumors of the pancreas by EUS. Gastrointest Endosc. 2001; 53:722–727.
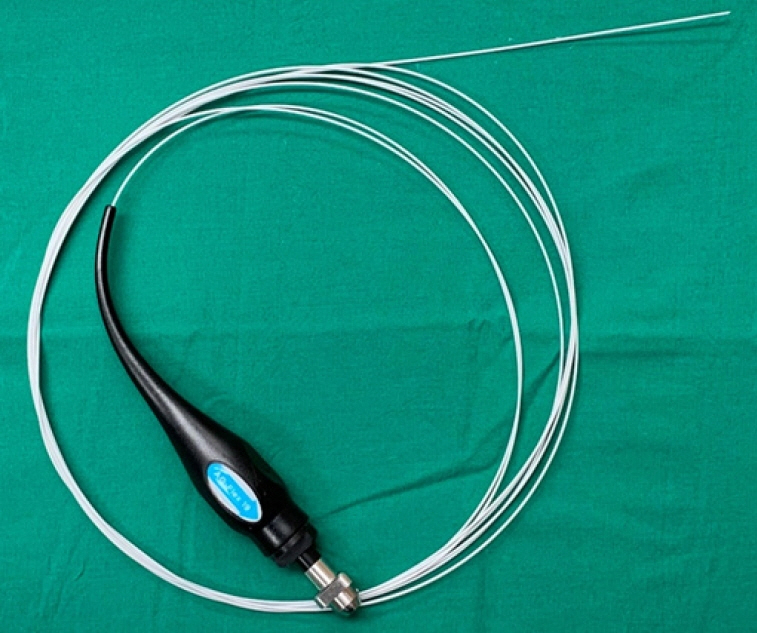
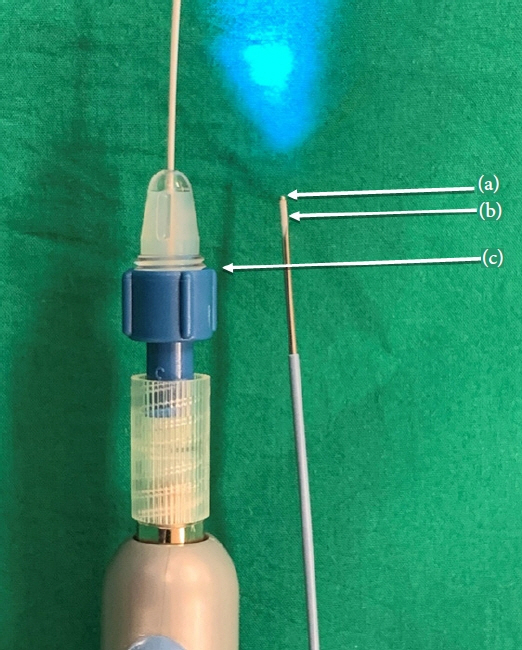
Article14. Mauna Kea Technologies. List of EUS-FNA needles successfully used with AQ-Flex 19 confocal miniprobes. Mauna Kea Technologies; 2020.15. Konda VJ, Aslanian HR, Wallace MB, et al. First assessment of needle-based confocal laser endomicroscopy during EUS-FNA procedures of the pancreas (with videos). Gastrointest Endosc. 2011; 74:1049–1060.
Article16. Konda VJ, Meining A, Jamil LH, et al. A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance. Endoscopy. 2013; 45:1006–1013.
Article17. Nakai Y, Iwashita T, Park DH, et al. Diagnosis of pancreatic cysts: EUS-guided, through-the-needle confocal laser-induced endomicroscopy and cystoscopy trial: DETECT study. Gastrointest Endosc. 2015; 81:1204–1214.
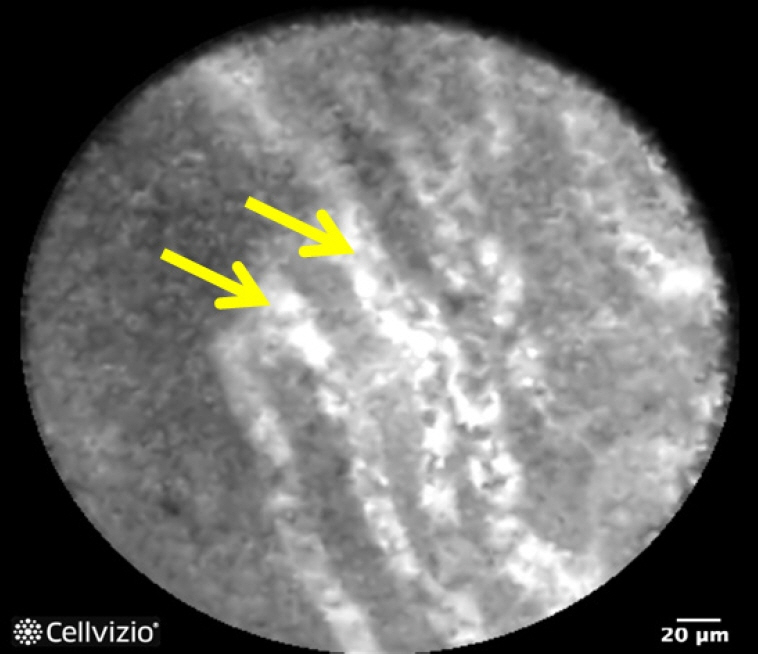
Article18. Napoleon B, Lemaistre AI, Pujol B, et al. In vivo characterization of pancreatic cystic lesions by needle-based confocal laser endomicroscopy (nCLE): proposition of a comprehensive nCLE classification confirmed by an external retrospective evaluation. Surg Endosc. 2016; 30:2603–2612.
Article19. Chin YK, Khor CJ, Goh BK, et al. The clinical evaluation of needle-based confocal laser endomicroscopy in the assessment of pancreatic cystic lesion: a pilot study. Proc Singap Healthc. 2018; 27:96–102.
Article20. Napoleon B, Palazzo M, Lemaistre AI, et al. Needle-based confocal laser endomicroscopy of pancreatic cystic lesions: a prospective multicenter validation study in patients with definite diagnosis. Endoscopy. 2019; 51:825–835.
Article21. Keane MG, Wehnert N, Perez-Machado M, et al. A prospective trial of CONfocal endomicroscopy in CYSTic lesions of the pancreas: CONCYST-01. Endosc Int Open. 2019; 7:E1117–E1122.
Article22. Kadayifci A, Atar M, Basar O, et al. Needle-based confocal laser endomicroscopy for evaluation of cystic neoplasms of the pancreas. Dig Dis Sci. 2017; 62:1346–1353.23. Karia K, Waxman I, Konda VJ, et al. Needle-based confocal endomicroscopy for pancreatic cysts: the current agreement in interpretation. Gastrointest Endosc. 2016; 83:924–927.
Article24. Krishna SG, Swanson B, Hart PA, et al. Validation of diagnostic characteristics of needle based confocal laser endomicroscopy in differentiation of pancreatic cystic lesions. Endosc Int Open. 2016; 4:E1124–E1135.
Article25. Krishna SG, Brugge WR, Dewitt JM, et al. Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions: an international external interobserver and intraobserver study (with videos). Gastrointest Endosc. 2017; 86:644–654.
Article26. Palazzo M, Sauvanet A, Gincul R, et al. Impact of needle-based confocal laser endomicroscopy on the therapeutic management of single pancreatic cystic lesions. Surg Endosc. 2020; 34:2532–2540.
Article27. Cheesman AR, Zhu H, Liao X, et al. Impact of EUS-guided microforceps biopsy sampling and needle-based confocal laser endomicroscopy on the diagnostic yield and clinical management of pancreatic cystic lesions. Gastrointest Endosc. 2020; 91:1095–1104.
Article28. Napoléon B, Lemaistre AI, Pujol B, et al. A novel approach to the diagnosis of pancreatic serous cystadenoma: needle-based confocal laser endomicroscopy. Endoscopy. 2015; 47:26–32.
Article29. Krishna SG, Hart PA, DeWitt JM, et al. EUS-guided confocal laser endomicroscopy: prediction of dysplasia in intraductal papillary mucinous neoplasms (with video). Gastrointest Endosc. 2020; 91:551–563.
Article30. Krishna SG, Swanson B, Conwell DL, et al. In vivo and ex vivo needle-based confocal endomicroscopy of intraductal papillary mucinous neoplasm of the pancreas. Gastrointest Endosc. 2015; 82:571–572.
Article31. Machicado JD, Napoleon B, Lennon AM, et al. Accuracy and agreement of a large panel of endosonographers for endomicroscopy-guided virtual biopsy of pancreatic cystic lesions. Pancreatology. 2022; 22:994–1002.
Article32. Le Pen C, Palazzo L, Napoléon B. A health economic evaluation of needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cysts. Endosc Int Open. 2017; 5:E987–E995.
Article33. Machicado JD, Chao WL, Carlyn DE, et al. High performance in risk stratification of intraductal papillary mucinous neoplasms by confocal laser endomicroscopy image analysis with convolutional neural networks (with video). Gastrointest Endosc. 2021; 94:78–87.
Article34. European Study Group on Cystic Tumours of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018; 67:789–804.35. Tanaka M, Fernández-Del Castillo C, Kamisawa T, et al. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017; 17:738–753.
Article36. Helms MM, Nixon J. Exploring SWOT analysis: where are we now?: a review of academic research from the last decade. J Strategy Manag. 2010; 3:215–251.37. Keane MG, Afghani E. A review of the diagnosis and management of premalignant pancreatic cystic lesions. J Clin Med. 2021; 10:1284.
Article38. Durkin C, Krishna SG. Advanced diagnostics for pancreatic cysts: confocal endomicroscopy and molecular analysis. World J Gastroenterol. 2019; 25:2734–2742.
Article39. McCarty TR, Garg R, Rustagi T. Pancreatic cyst fluid glucose in differentiating mucinous from nonmucinous pancreatic cysts: a systematic review and meta-analysis. Gastrointest Endosc. 2021; 94:698–712.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-guided needle-based confocal laser endomicroscopy for diagnosis of solid pancreatic lesions
- A Review of Probe-Based Confocal Laser Endomicroscopy for Pancreaticobiliary Disease
- Recent developments in endoscopic ultrasound-guided diagnosis and therapy of pancreatic cystic neoplasms
- The Role of Needle-Based Confocal Laser Endomicroscopy in the Evaluation of Pancreatic Cystic Lesions: A Systematic Review
- Endoscopic Ultrasound-Guided Fine Needle Aspiration in Cystic Pancreatic Lesions