J Korean Med Sci.
2022 Mar;37(9):e74. 10.3346/jkms.2022.37.e74.
Burnout of Faculty Members of Medical Schools in Korea
- Affiliations
-
- 1Department of Pediatrics and Medical Education, Gyeongsang National University School of Medicine, Gyeongsang National University Hospital, Gyeongsang Institute of Health Sciences, Jinju, Korea
- 2Department of Social Welfare, Gyeongsang National University College of Social Sciences, Jinju, Korea
- 3Department of Psychiatry, Gyeongsang National University School of Medicine, Gyeongsang National University Hospital, Gyeongsang Institute of Health Sciences, Jinju, Korea
- 4Department of Parasitology, Hallym University College of Medicine, Chuncheon, Korea
- 5Department of Medical Education, Chosun University School of Medicine, Gwangju, Korea
- 6Department of Medical Education, Chungnam National University School of Medicine, Daejeon, Korea
- 7Department of Emergency Medicine, Chung-Ang University College of Medicine, Seoul, Korea
- 8Department of Medical Education, Pusan National University School of Medicine, Yangsan, Korea
- 9Department of Thoracic and Cardiovascular Surgery, Keimyung University School of Medicine, Daegu, Korea
- 10Department of Thoracic and Cardiovascular Surgery, Kangwon National University Medical School, Chuncheon, Korea
- 11Korea Association of Medical Colleges, Department of Physiology, Korea University College of Medicine, Seoul, Korea
- 12Department of Medical Education, Korea University College of Medicine, Seoul, Korea
- KMID: 2526974
- DOI: http://doi.org/10.3346/jkms.2022.37.e74
Abstract
- Background
There is no national survey on medical school faculty members’ burnout in Korea. This study aimed to investigate burnout levels and explore possible factors related to burnout among faculty members of Korean medical schools.
Methods
An anonymous online questionnaire was distributed to 40 Korean medical schools from October 2020 to December 2020. Burnout was measured by a modified and revalidated version of the Maslach Burnout Inventory-Human Service Survey.
Results
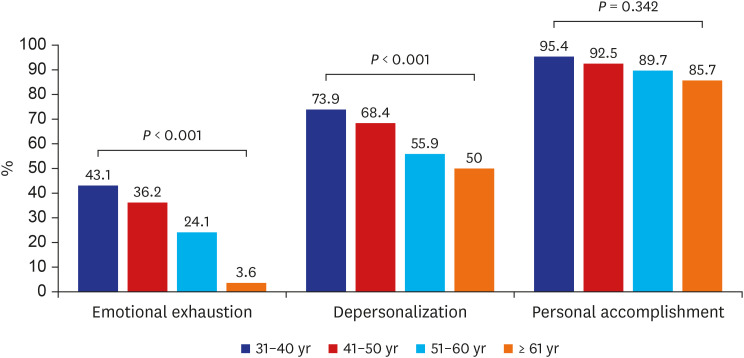
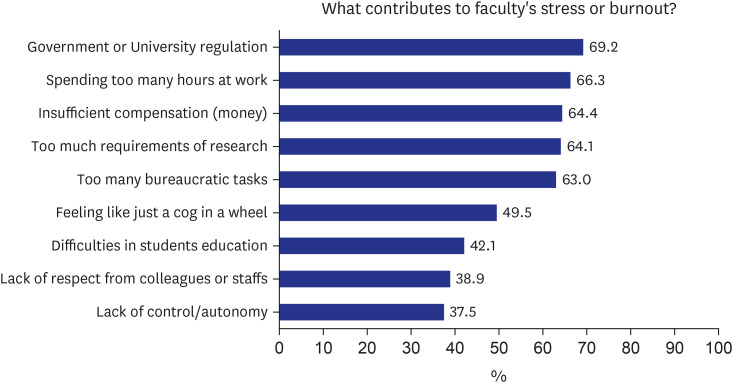
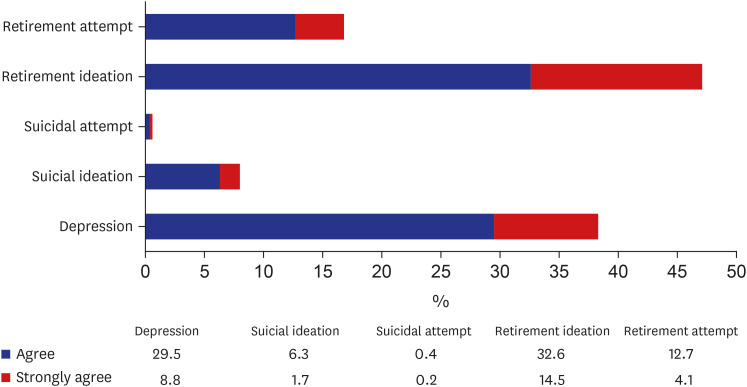
A total of 996 faculty members participated in the survey. Of them, 855 answered the burnout questions, and 829 completed all the questions in the questionnaire. A significant number of faculty members showed a high level of burnout in each sub-dimension: 34% in emotional exhaustion, 66.3% in depersonalization, and 92.4% in reduced personal accomplishment. A total of 31.5% of faculty members revealed a high level of burnout in two sub-dimensions, while 30.5% revealed a high level of burnout in all three sub-dimensions. Woman faculty members or those younger than 40 reported significantly higher emotional exhaustion and depersonalization. Long working hours (≥ 80 hours/week) showed the highest reduced personal accomplishment scores (F = 4.023, P = 0.018). The most significant stressor or burnout source was “excessive regulation by the government or university.” The research was the most exasperating task, but the education was the least stressful.
Conclusion
This first nationwide study alerts that a significant number of faculty members in Korean medical schools seem to suffer from a high level of burnout. Further studies are necessary for identifying the burnout rate, related factors, and strategies to overcome physician burnout.
Keyword
Figure
Cited by 1 articles
-
Specialty impact on residents’ perceived quality of life, stress, and job satisfaction: a comparative study
Bo Young Kim, Inah Yoon, Seong John Han, Suk-Kyung Hong, Sehoon Choi, Hyo-Jin Kwon, Eun Key Kim
Ann Surg Treat Res. 2023;105(4):188-197. doi: 10.4174/astr.2023.105.4.188.
Reference
-
1. World Health Organization. Burn-out an ‘occupational phenomenon’: International Classification of Disease. Updated 2019. Accessed January 31, 2021. https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases .2. Witkoski A, Dickson VV. Hospital staff nurses’ work hours, meal periods, and rest breaks. A review from an occupational health nurse perspective. AAOHN J. 2010; 58(11):489–497. PMID: 21053797.
Article3. Price G, Norbeck T, Ray W, Libby R, Jones P. 2018 survey of America’s physicians practice patterns & perspectives. Updated 2018. Accessed December 7, 2021. https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/Pdf/MerrittHawkins_PhysiciansFoundation_Survey2018.pdf .4. British Medical Association. The state of medical education and practice in the UK. The workforce report. 2019. Updated 2019. Accessed December 7, 2021. https://www.bma.org.uk/collective-voice/policy-and-research/education-training-and-workforce/supporting-the-mental-health-of-doctors-in-the-workforce .5. Gabbay RA, Barrett AM. Endocrinologist burnout: we need to tackle it and bring joy to work. J Clin Endocrinol Metab. 2020; 105(7):e2652–e2656.
Article6. Panagioti M, Geraghty K, Johnson J, Zhou A, Panagopoulou E, Chew-Graham C, et al. Association between physician burnout and patient safety, professionalism, and patient satisfaction: a systematic review and meta-analysis. JAMA Intern Med. 2018; 178(10):1317–1331. PMID: 30193239.
Article7. Seo JH, Kim BK, Bae HO, Im SJ, Kim KH. Burnout among medical school faculty members: incidence and demographic characteristics at three medical schools in the Busan and Gyeongnam area of Korea. Korean Med Educ Rev. 2014; 16(2):67–76.
Article8. Park YH, Yoon HB. Research on the factors influencing professional satisfaction of professors in medical colleges. Korean J Med Educ. 2005; 17(1):59–71.
Article9. Kim JW, Myung SJ, Yoon HB, Moon SH, Ryu H, Yim JJ. How medical education survives and evolves during COVID-19: our experience and future direction. PLoS One. 2020; 15(12):e0243958. PMID: 33338045.
Article10. Lee YM, Park KD, Seo JH. New paradigm of pediatric clinical clerkship during the epidemic of COVID-19. J Korean Med Sci. 2020; 35(38):e344. PMID: 32989936.
Article11. Kang YJ, Kim DH. Pre-clerkship students’ perception and learning behavior of online classes during coronavirus disease 2019 pandemic. Korean J Med Educ. 2021; 33(2):125–131. PMID: 34062644.
Article12. Lee YM, Park H, Pyun SB, Yoon YW. Enforced format change to medical education webinar during the coronavirus disease 2019 pandemic. Korean J Med Educ. 2020; 32(2):101–102. PMID: 32486619.
Article13. Medifonews. Top 10 medical news in 2020. Updated 2020. Accessed April 15, 2021. https://medifonews.com/mobile/article.html?no=157595 .14. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA, USA: Consulting Psychologists Press;1996.15. Linacre JM. What do infit and outfit, mean-square and standardized mean? Rasch Meas Trans. 2002; 16(2):878.16. Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. New York, NY, USA: McGraw-Hill;1994.17. Gugiu C, Gugiu MR. Determining the minimum reliability standard based on a decision criterion. J Exp Educ. 2018; 86(3):458–472.
Article18. Del Carmen MG, Herman J, Rao S, Hidrue MK, Ting D, Lehrhoff SR, et al. Trends and factors associated with physician burnout at a multispecialty academic faculty practice organization. JAMA Netw Open. 2019; 2(3):e190554. PMID: 30874776.
Article19. McKinley N, McCain RS, Convie L, Clarke M, Dempster M, Campbell WJ, et al. Resilience, burnout and coping mechanisms in UK doctors: a cross-sectional study. BMJ Open. 2020; 10(1):e031765.
Article20. Dandar VM, Grigsby RK, Bunton SA, Bunton SA. Burnout among faculty in academic medicine. AAMC Anal Brief. 2019; 19(1):1–3.21. Templeton K, Bernstein CA, Sukhera J, Nora LM, Newman C, Burstin H, et al. Gender-based differences in burnout: issues faced by women physicians. NAM Perspect. 2019; 1–16.
Article22. Choi J, Lee JE, Choi B, Kim J, Lee SE. Experiences and perceptions of gender discrimination and equality among Korean surgeons: results of a survey of the Korean Surgery Society. J Korean Med Sci. 2021; 36(48):e323. PMID: 34904405.
Article23. Kane L. Medscape national physician burnout & suicidal report 2020: the generation divide. Updated 2020. Accessed January 15, 2021. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460#350% .24. Southwick FS, Southwick SM. The loss of a sense of control as a major contributor to physician burnout: a neuropsychiatric pathway to prevention and recovery. JAMA Psychiatry. 2018; 75(7):665–666. PMID: 29799941.
Article25. Kane L. “Death by 1000 cuts”: Medscape national physician burnout & suicidal report 2021: the generation divide. Updated 2021. Accessed April 20, 2021. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456 .26. Shanafelt TD, Boone S, Tan L, Dyrbye LN, Sotile W, Satele D, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012; 172(18):1377–1385. PMID: 22911330.
Article27. Seo DJ, Kim S, Kim HT, Park WK, Park JH, Yang EB, et al. A Study on the Present State of Medical Education in Korea: The White Book. Seoul, Korea: Research Institute for Healthcare Policy;2014.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Job stress and burnout affecting the mental health of Korean medical faculty members: constructing causality among latent variables
- The meaning of medical professionalism for the faculty members of medical school and university hospitals in Korea
- Prevalence of burnout and related factors in nursing faculty members: a systematic review
- Evaluation of medical school faculty members’ educational performance in Korea in 2022 through analysis of the promotion regulations: a mixed methods study
- Faculty Development for Medical Faculty: Importance and Strategies