Korean J Sports Med.
2022 Mar;40(1):49-53. 10.5763/kjsm.2022.40.1.49.
Distraction Arthroplasty Combined with Lateral Meniscal Allograft Transplantation in an Athlete with Advanced Lateral Osteoarthritis: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Konkuk University Medical Center, Seoul, Korea
- 2Department of Orthopaedic Surgery, Hanyang University Myongji Hospital, Goyang, Korea
- KMID: 2526688
- DOI: http://doi.org/10.5763/kjsm.2022.40.1.49
Abstract
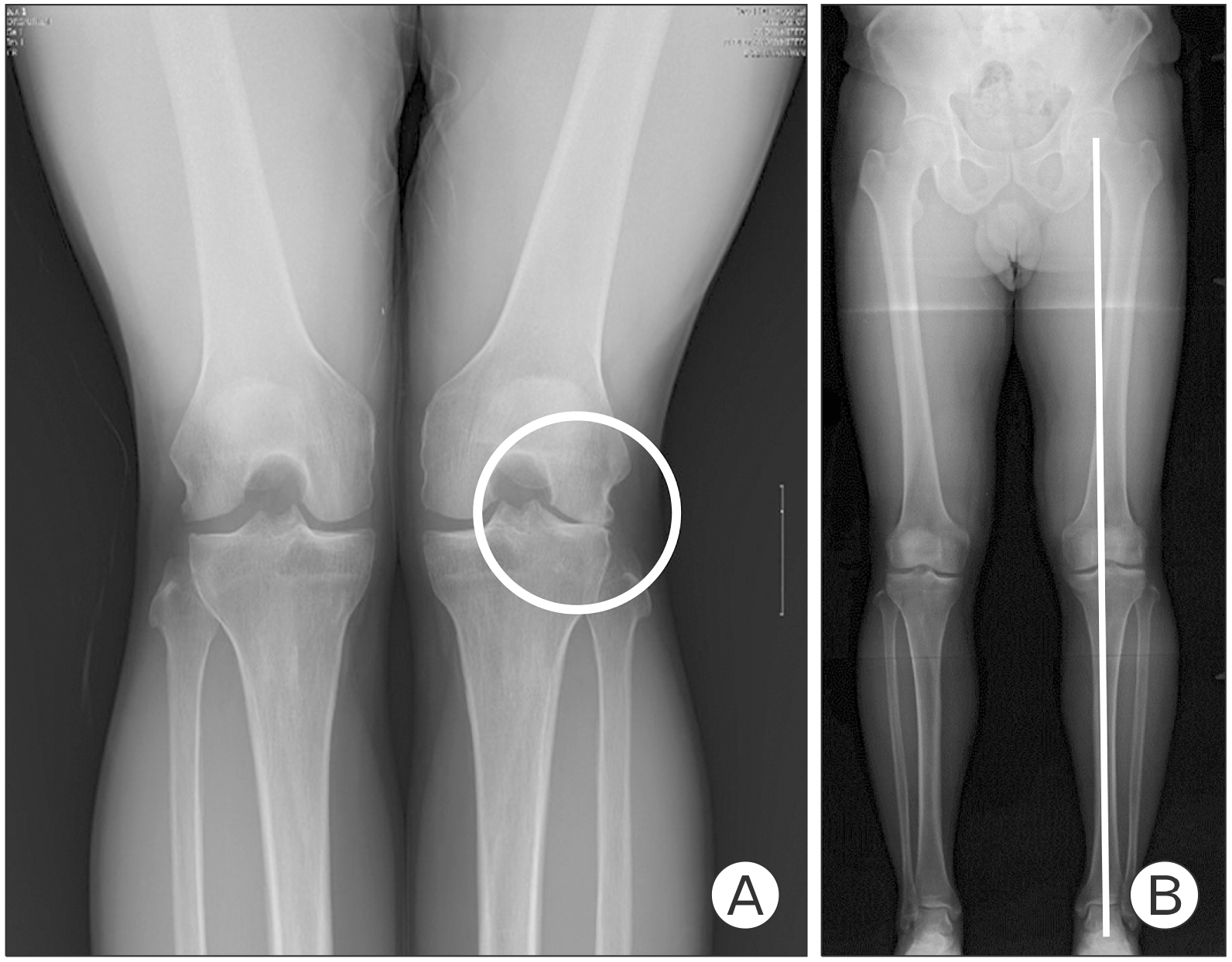
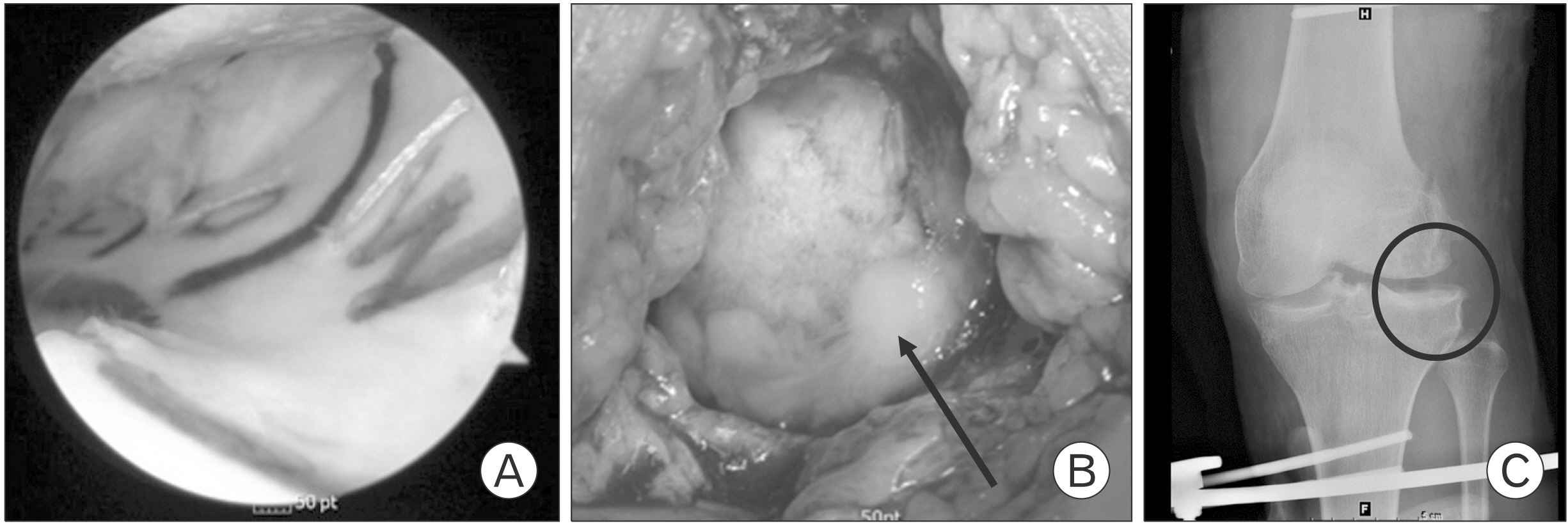
- The knee function of young and active patients with advanced osteoarthritis is unavoidably reduced and they are trapped in “treatment gap” without surgical treatment. In recent years, distraction arthroplasty (DA) has emerged as a viable alternative in the treatment of advanced osteoarthritis in young and active patients to delay knee arthroplasty. However, outcomes after DA are very rare in young and active patients. We present a case of a 36-year-old man (a professional skier) who had lateral meniscus deficiency and severe joint space narrowing. He underwent DA plus lateral meniscal allograft transplantation combined with cartilage repair. The patient showed excellent result 9 years postoperatively with return to high level of sport activity.
Keyword
Figure
Reference
-
1. Khan M, Adili A, Winemaker M, Bhandari M. 2018; Management of osteoarthritis of the knee in younger patients. CMAJ. 190:E72–9. DOI: 10.1503/cmaj.170696. PMID: 29358201. PMCID: PMC5780266.
Article2. Rensing N, Prabhakar G, Kusnezov N, Zarkadis NJ, Waterman BR, Pallis M. 2019; Distal femoral osteotomy in a young symptomatic population: outcomes correlate to concomitant pathology. J Orthop. 16:283–8. DOI: 10.1016/j.jor.2019.04.016. PMID: 31193264. PMCID: PMC6522751.
Article3. Hoorntje A, Kuijer PP, Koenraadt KL, et al. Return to sport and work after randomization for knee distraction versus high tibial osteotomy: is there a difference? J Knee Surg 2020 Nov 23 [Epub]. https://doi.org/10.1055/s-0040-1721027. DOI: 10.1055/s-0040-1721027. PMID: 33853157.
Article4. Goh EL, Lou WC, Chidambaram S, Ma S. 2019; The role of joint distraction in the treatment of knee osteoarthritis: a systematic review and quantitative analysis. Orthop Res Rev. 11:79–92. DOI: 10.2147/ORR.S211060. PMID: 31496838. PMCID: PMC6689796.5. Takahashi T, Baboolal TG, Lamb J, Hamilton TW, Pandit HG. 2019; Is knee joint distraction a viable treatment option for knee OA?: a literature review and meta-analysis. J Knee Surg. 32:788–95. DOI: 10.1055/s-0038-1669447. PMID: 30157528.
Article6. Rue JP, Yanke AB, Busam ML, McNickle AG, Cole BJ. 2008; Prospective evaluation of concurrent meniscus transplantation and articular cartilage repair: minimum 2-year follow-up. Am J Sports Med. 36:1770–8. DOI: 10.1177/0363546508317122. PMID: 18483199.
Article7. Besselink NJ, Vincken KL, Bartels LW, et al. 2020; Cartilage quality (dGEMRIC Index) following knee joint distraction or high tibial osteotomy. Cartilage. 11:19–31. DOI: 10.1177/1947603518777578. PMID: 29862834. PMCID: PMC6918034.8. van der Woude JA, Welsing PM, van Roermund PM, Custers RJ, Kuchuk NO, Lafeber FP. 2016; Prediction of cartilaginous tissue repair after knee joint distraction. Knee. 23:792–5. DOI: 10.1016/j.knee.2016.02.015. PMID: 27543178.
Article9. Lee DW, Park JH, Chung KS, Ha JK, Kim JG. 2017; Arthroscopic lateral meniscal allograft transplantation with the key-hole technique. Arthrosc Tech. 6:e1815–20. DOI: 10.1016/j.eats.2017.06.057. PMID: 29430389. PMCID: PMC5799489.
Article10. van der Woude JA, Wiegant K, van Roermund PM, et al. 2017; Five-year follow-up of knee joint distraction: clinical benefit and cartilaginous tissue repair in an open uncontrolled prospective study. Cartilage. 8:263–71. DOI: 10.1177/1947603516665442. PMID: 28618871. PMCID: PMC5625862.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Templating in Lateral Meniscal Allograft Transplantation
- Management of Meniscal Injury: Repair, Meniscectomy, and Transplantation
- MR Findings of Meniscal Cysts
- Measurement of Meniscal Slope Angles in Normal Korean using MRI
- Comparison of the Pollard Method and the MRI Dimensions for Meniscal Sizing in Koreans