Intest Res.
2022 Jan;20(1):53-63. 10.5217/ir.2020.00079.
The dietary practices and beliefs of British South Asian people living with inflammatory bowel disease: a multicenter study from the United Kingdom
- Affiliations
-
- 1Division of Diabetes, Endocrinology and Gastroenterology, Faculty of Biology, Medicine and Health, The University of Manchester, Manchester, UK
- 2Department of Gastroenterology, Salford Royal NHS Foundation Trust, Salford, UK
- 3Section of IBD, Division of Gastroenterology, The Pennine Acute Hospitals NHS Trust, Manchester, UK
- 4Department of IBD, St Mark’s Hospital and Imperial College, London, UK
- 5Gastroenterology Department, Barts Health NHS Trust, The Royal London Hospital, London, UK
- 6Gastroenterology Unit, Royal Wolverhampton NHS Trust, Wolverhampton, UK
- 7Research Institute in Healthcare Science (RIHS), University of Wolverhampton, Wolverhampton, UK
- KMID: 2525072
- DOI: http://doi.org/10.5217/ir.2020.00079
Abstract
- Background/Aims
Epidemiological associations have implicated factors associated with Westernization, including the Western diet, in the development of inflammatory bowel disease (IBD). The role of diet in IBD etiopathogenesis, disease control and symptom management remains incompletely understood. Few studies have collected data on the dietary habits of immigrant populations living with IBD. Our aim was to describe the dietary practices and beliefs of British South Asians with IBD.
Methods
A 30-item questionnaire was developed and consecutively administered to 255 British South Asians with IBD attending gastroenterology clinics in the United Kingdom.
Results
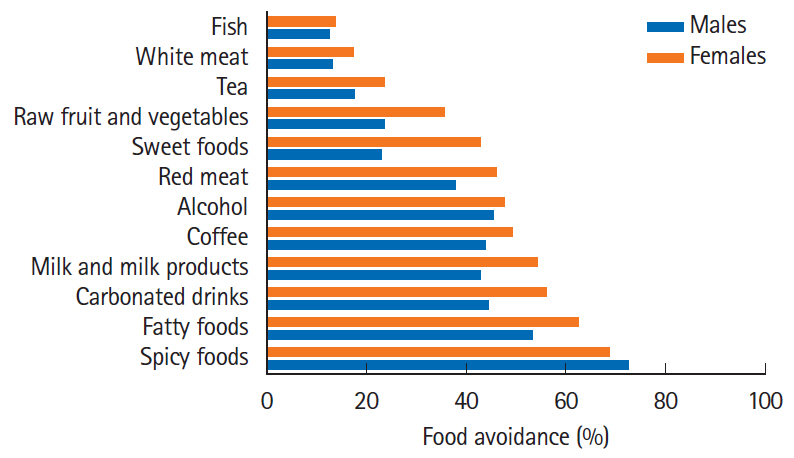
Fifty-one percent of participants believed diet was the initiating factor for their IBD and 63% felt diet had previously triggered disease relapse. Eighty-nine percent avoided certain dietary items in the belief that this would prevent relapse. The most commonly avoided foods and drinks were spicy and fatty foods, carbonated drinks, milk products, alcohol, coffee, and red meat. A third of patients had tried a whole food exclusion diet, most commonly lactose- or gluten-free, and this was most frequently reported amongst those with clinically active IBD (P= 0.02). Almost 60% of participants avoided eating the same menu as their family, or eating out, at least sometimes, to prevent IBD relapse.
Conclusions
British South Asians with IBD demonstrate significant dietary beliefs and food avoidance behaviors with increased frequency compared to those reported in Caucasian IBD populations. Studies in immigrant populations may offer valuable insights into the interaction between diet, Westernization and cultural drift in IBD pathogenesis and symptomatology.
Figure
Reference
-
1. Abraham C, Cho JH. Inflammatory bowel disease. N Engl J Med. 2009; 361:2066–2078.
Article2. Zhang YZ, Li YY. Inflammatory bowel disease: pathogenesis. World J Gastroenterol. 2014; 20:91–99.
Article3. Ananthakrishnan AN. Environmental risk factors for inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2013; 9:367–374.4. Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018; 390:2769–2778.
Article5. Misra R, Faiz O, Munkholm P, Burisch J, Arebi N. Epidemiology of inflammatory bowel disease in racial and ethnic migrant groups. World J Gastroenterol. 2018; 24:424–437.
Article6. Farrukh A, Mayberry JF. Inflammatory bowel disease and the South Asian diaspora. JGH Open. 2019; 3:358–360.
Article7. Probert CS, Jayanthi V, Pinder D, Wicks AC, Mayberry JF. Epidemiological study of ulcerative proctocolitis in Indian migrants and the indigenous population of Leicestershire. Gut. 1992; 33:687–693.
Article8. Benchimol EI, Mack DR, Guttmann A, et al. Inflammatory bowel disease in immigrants to Canada and their children: a population-based cohort study. Am J Gastroenterol. 2015; 110:553–563.
Article9. Williams CN. Does the incidence of IBD increase when persons move from a low- to a high-risk area? Inflamm Bowel Dis. 2008; 14 Suppl 2:S41–S42.
Article10. Rizzello F, Spisni E, Giovanardi E, et al. Implications of the westernized diet in the onset and progression of IBD. Nutrients. 2019; 11:1033.
Article11. Limdi JK, Aggarwal D, McLaughlin JT. Dietary practices and beliefs in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2016; 22:164–170.
Article12. Hou JK, Lee D, Lewis J. Diet and inflammatory bowel disease: review of patient-targeted recommendations. Clin Gastroenterol Hepatol. 2014; 12:1592–1600.13. Jowett SL, Seal CJ, Phillips E, Gregory W, Barton JR, Welfare MR. Dietary beliefs of people with ulcerative colitis and their effect on relapse and nutrient intake. Clin Nutr. 2004; 23:161–170.
Article14. Casanova MJ, Chaparro M, Molina B, et al. Prevalence of malnutrition and nutritional characteristics of patients with inflammatory bowel disease. J Crohns Colitis. 2017; 11:1430–1439.15. Richman E, Rhodes JM. Review article: evidence-based dietary advice for patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013; 38:1156–1171.
Article16. Sasson AN, Ananthakrishnan AN, Raman M. Diet in treatment of inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2021; 19:425–435.
Article17. Lomer MC, Kodjabashia K, Hutchinson C, Greenfield SM, Thompson RP, Powell JJ. Intake of dietary iron is low in patients with Crohn’s disease: a case- control study. Br J Nutr. 2004; 91:141–148.
Article18. Hwang C, Ross V, Mahadevan U. Popular exclusionary diets for inflammatory bowel disease: the search for a dietary culprit. Inflamm Bowel Dis. 2014; 20:732–741.19. Lamb CA, Kennedy NA, Raine T, et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut. 2019; 68(Suppl 3):s1–s106.
Article20. Levine A, Rhodes JM, Lindsay JO, et al. Dietary guidance from the International Organization for the Study of Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2020; 18:1381–1392.
Article21. Holt DQ, Strauss BJ, Moore GT. Patients with inflammatory bowel disease and their treating clinicians have different views regarding diet. J Hum Nutr Diet. 2017; 30:66–72.
Article22. Limdi JK, Butcher RO. Information resources and inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:E89–E90.
Article23. Bernstein KI, Promislow S, Carr R, Rawsthorne P, Walker JR, Bernstein CN. Information needs and preferences of recently diagnosed patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:590–598.
Article24. Palant A, Koschack J, Rassmann S, Lucius-Hoene G, Karaus M, Himmel W. “And then you start to loose it because you think about Nutella”: the significance of food for people with inflammatory bowel disease - a qualitative study. BMC Gastroenterol. 2015; 15:93.
Article25. Czuber-Dochan W, Morgan M, Hughes LD, Lomer MCE, Lindsay JO, Whelan K. Perceptions and psychosocial impact of food, nutrition, eating and drinking in people with inflammatory bowel disease: a qualitative investigation of food-related quality of life. J Hum Nutr Diet. 2020; 33:115–127.
Article26. Zallot C, Quilliot D, Chevaux JB, et al. Dietary beliefs and behavior among inflammatory bowel disease patients. Inflamm Bowel Dis. 2013; 19:66–72.
Article27. Cohen AB, Lee D, Long MD, et al. Dietary patterns and self-reported associations of diet with symptoms of inflammatory bowel disease. Dig Dis Sci. 2013; 58:1322–1328.
Article28. Principi M, Losurdo G, Iannone A, et al. Differences in dietary habits between patients with inflammatory bowel disease in clinical remission and a healthy population. Ann Gastroenterol. 2018; 31:469–473.
Article29. Crooks B, McLaughlin J, Matsuoka K, Kobayashi T, Yamazaki H, Limdi JK. The dietary practices and beliefs of people living with inactive ulcerative colitis. Eur J Gastroenterol Hepatol. [published online ahead of print September 17, 2020]. https://doi.org/10.1097/MEG.0000000000001911.
Article30. Tomar SK, Kedia S, Upadhyay AD, et al. Impact of dietary beliefs and practices on patients with inflammatory bowel disease: an observational study from India. JGH Open. 2017; 1:15–21.
Article31. Holmboe-Ottesen G, Wandel M. Changes in dietary habits after migration and consequences for health: a focus on South Asians in Europe. Food Nutr Res. 2012; 56:18891.
Article32. Mukherjee S, Beresford B, Atkin K, Sebastian S. The need for culturally competent care within gastroenterology services: evidence from research with adults of South Asian origin living with inflammatory bowel disease. J Crohns Colitis. [published online ahead of print June 23, 2020]. https://doi.org/10.1093/ecco-jcc/jjaa117.
Article33. Probert CS, Bhakta P, Bhamra B, Jayanthi V, Mayberry JF. Diet of South Asians with inflammatory bowel disease. Arq Gastroenterol. 1996; 33:132–135.34. Silverberg MS, Satsangi J, Ahmad T, et al. Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol. 2005; 19 Suppl A:5A–36A.
Article35. Jairath V, Khanna R, Zou GY, et al. Development of interim patient-reported outcome measures for the assessment of ulcerative colitis disease activity in clinical trials. Aliment Pharmacol Ther. 2015; 42:1200–1210.
Article36. Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980; 1:514.
Article37. Vagianos K, Clara I, Carr R, et al. What are adults with inflammatory bowel disease (IBD) eating? A closer look at the dietary habits of a population-based Canadian IBD cohort. JPEN J Parenter Enteral Nutr. 2016; 40:405–411.
Article38. 2011 Census aggregate data. UK data service. Office for National Statistics Web site. Updated 2011. Accessed November 30, 2020. https://www.ons.gov.uk/census/2011census/2011c ensusdata.39. Kinsey L, Burden S. A survey of people with inflammatory bowel disease to investigate their views of food and nutritional issues. Eur J Clin Nutr. 2016; 70:852–854.
Article40. Hayes P,, Corish C, O’Mahony E, Quigley EM. A dietary survey of patients with irritable bowel syndrome. J Hum Nutr Diet. 2014; Apr. 27 Suppl 2:36–47.
Article41. Cox SR, Prince AC, Myers CE, et al. Fermentable carbohydrates [FODMAPs] exacerbate functional gastrointestinal symptoms in patients with inflammatory bowel disease: a randomised, double-blind, placebo-controlled, cross-over, rechallenge trial. J Crohns Colitis. 2017; 11:1420–1429.
Article42. Malik TF, Panuganti KK. Lactose intolerance. Treasure Island: StatPearls Publishing;2020.43. Szilagyi A, Galiatsatos P, Xue X. Systematic review and meta-analysis of lactose digestion, its impact on intolerance and nutritional effects of dairy food restriction in inflammatory bowel diseases. Nutr J. 2016; 15:67.
Article44. Ananthakrishnan AN. Vitamin D and inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2016; 12:513–515.45. Lim HS, Kim SK, Hong SJ. Food elimination diet and nutritional deficiency in patients with inflammatory bowel disease. Clin Nutr Res. 2018; 7:48–55.
Article46. Reich J, Guo L, Groshek J, et al. Social media use and preferences in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2019; 25:587–591.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of the Histological Cell Types of Lung Cancer in Workers suffering from Asbestosis in the United Kingdom
- Beliefs about Tic Disorders and Tourette's Syndrome in South Korea: An Online Panel Survey
- Relationship of dietary self-efficacy and illness beliefs, perceived benefits and perceived barriers for the reduction of sodium intake in the elderly
- Cryotherapy versus radiofrequency ablation in the treatment of post-chemoradiotherapy patients with recurrence of Barrett’s dysplasia
- Nutritional Support in Patients with Inflammatory Bowel Diseases