Clin Endosc.
2022 Jan;55(1):150-155. 10.5946/ce.2020.217.
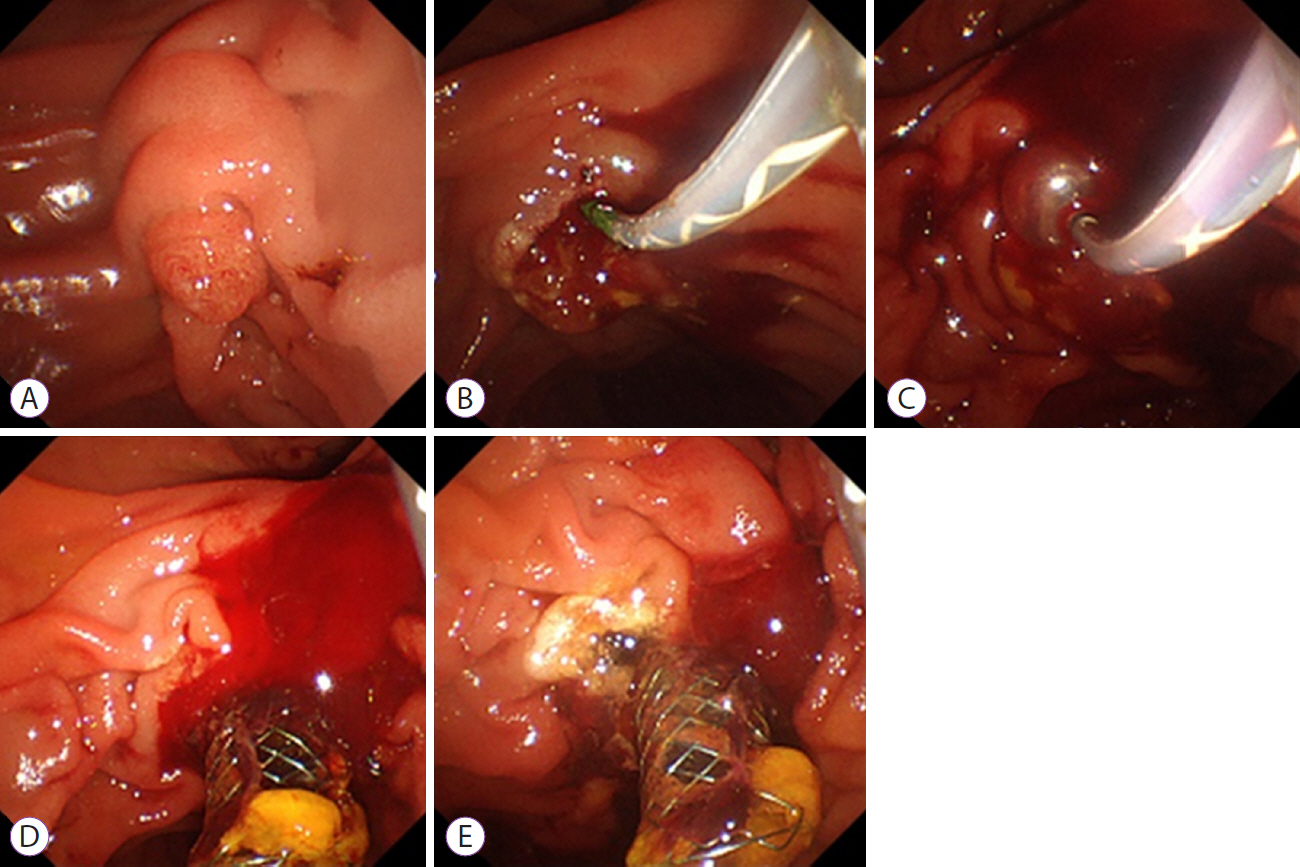
Practical Experiences of Unsuccessful Hemostasis with Covered Self-Expandable Metal Stent Placement for Post-Endoscopic Sphincterotomy Bleeding
- Affiliations
-
- 1Department of Gastroenterology and Metabolism, Nagoya City University Graduate School of Medical Sciences, Nagoya, Japan
- 2Department of Gastroenterology, Aichi Medical University, Nagakute, Japan
- KMID: 2525063
- DOI: http://doi.org/10.5946/ce.2020.217
Abstract
- We reviewed 7 patients with unsuccessful endoscopic hemostasis using covered self-expandable metal stent (CSEMS) placement for post-endoscopic sphincterotomy (ES) bleeding. ES with a medium incision was performed in 6 and with a large incision in 1 patient. All but 1 of them (86%) showed delayed bleeding, warranting second endoscopic therapies followed by CSEMS placement 1–5 days after the initial ES. Subsequent CSEMS placement did not achieve complete hemostasis in any of the patients. Lateral-side incision lines (3 or 9 o’clock) had more frequent bleeding points (71%) than oral-side incision lines (11–12 o’clock; 29%). Additional endoscopic hemostatic procedures with hemostatic forceps, hypertonic saline epinephrine, or hemoclip achieved excellent hemostasis, resulting in complete hemostasis in all patients. These experiences provide an alert: CSEMS placement is not an ultimate treatment for post-ES bleeding, despite its effectiveness. The lateral-side of the incision line, as well as the oral-most side, should be carefully examined for bleeding points, even after the CSEMS placement.
Keyword
Figure
Reference
-
1. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918.2. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998; 48:1–10.3. Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001; 96:417–423.4. ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017; 85:32–47.5. Itoi T, Yasuda I, Doi S, Mukai T, Kurihara T, Sofuni A. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011; 43:369–372.6. Canena J, Liberato M, Horta D, Romão C, Coutinho A. Short-term stenting using fully covered self-expandable metal stents for treatment of refractory biliary leaks, postsphincterotomy bleeding, and perforations. Surg Endosc. 2013; 27:313–324.7. Cochrane J, Schlepp G. Comparing endoscopic intervention against fully covered self-expanding metal stent placement for post-endoscopic sphincterotomy bleed (CEASE Study). Endosc Int Open. 2016; 4:E1261–E1264.8. Inoue T, Ibusuki M, Kitano R, et al. Early covered self-expandable metal stent placement is effective for massive post-endoscopic sphincterotomy bleeding. Dig Dis Sci. 2020; 65:3324–3331.9. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.10. Iwasaki E, Itoi T, Kanai T. Metal stent for refractory post-ES bleeding: is this the ultimate treatment modality? Endosc Int Open. 2016; 4:E1265–E1266.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Temporary Placement of a Newly Designed, Fully Covered, Self-Expandable Metal Stent for Refractory Bile Leaks
- Role of Fully Covered Self-Expandable Metal Stent for Treatment of Benign Biliary Strictures and Bile Leaks
- Biliary Self-Expandable Metal Stent Could Be Recommended as a First Treatment Modality for Immediate Refractory Post-Endoscopic Retrograde Cholangiopancreatography Bleeding
- Efficacy of hemostasis by gastroduodenal covered metal stent placement for hemorrhagic duodenal stenosis due to pancreatobiliary cancer invasion: a retrospective study
- Management of Occluded Biliary Uncovered Metal Stents: Covered Self Expandable Metallic Stent vs. Uncovered Self Expandable Metallic Stent