Clin Endosc.
2024 Sep;57(5):628-636. 10.5946/ce.2023.155.
Efficacy of hemostasis by gastroduodenal covered metal stent placement for hemorrhagic duodenal stenosis due to pancreatobiliary cancer invasion: a retrospective study
- Affiliations
-
- 1Department of Hepatobiliary and Pancreatic Oncology, National Cancer Center Hospital, Tokyo, Japan
- 2Department of Gastroenterology and Hepatology, International University of Health and Welfare Atami Hospital, Shizuoka, Japan
- 3Endoscopy Division, National Cancer Center Hospital, Tokyo, Japan
- 4Department of Hepatobiliary and Pancreatic Oncology, National Cancer Center Hospital East, Kashiwa, Japan
- 5Department of Diagnostic Radiology, National Cancer Center Hospital, Tokyo, Japan
- KMID: 2559214
- DOI: http://doi.org/10.5946/ce.2023.155
Abstract
- Background/Aims
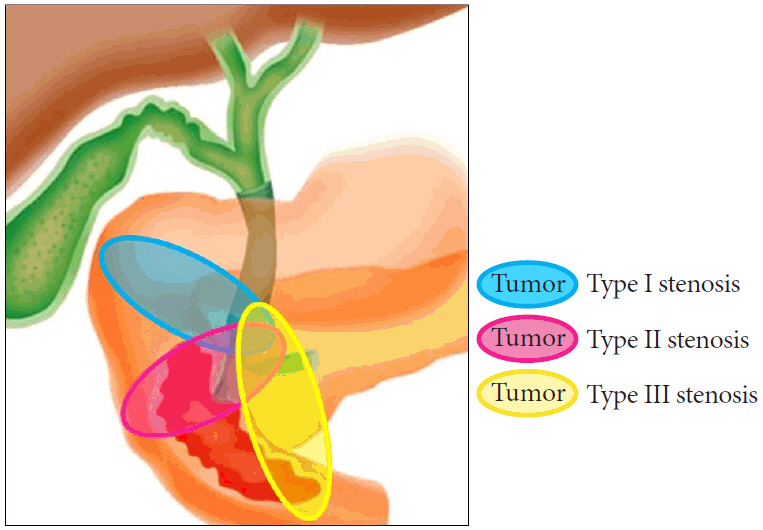
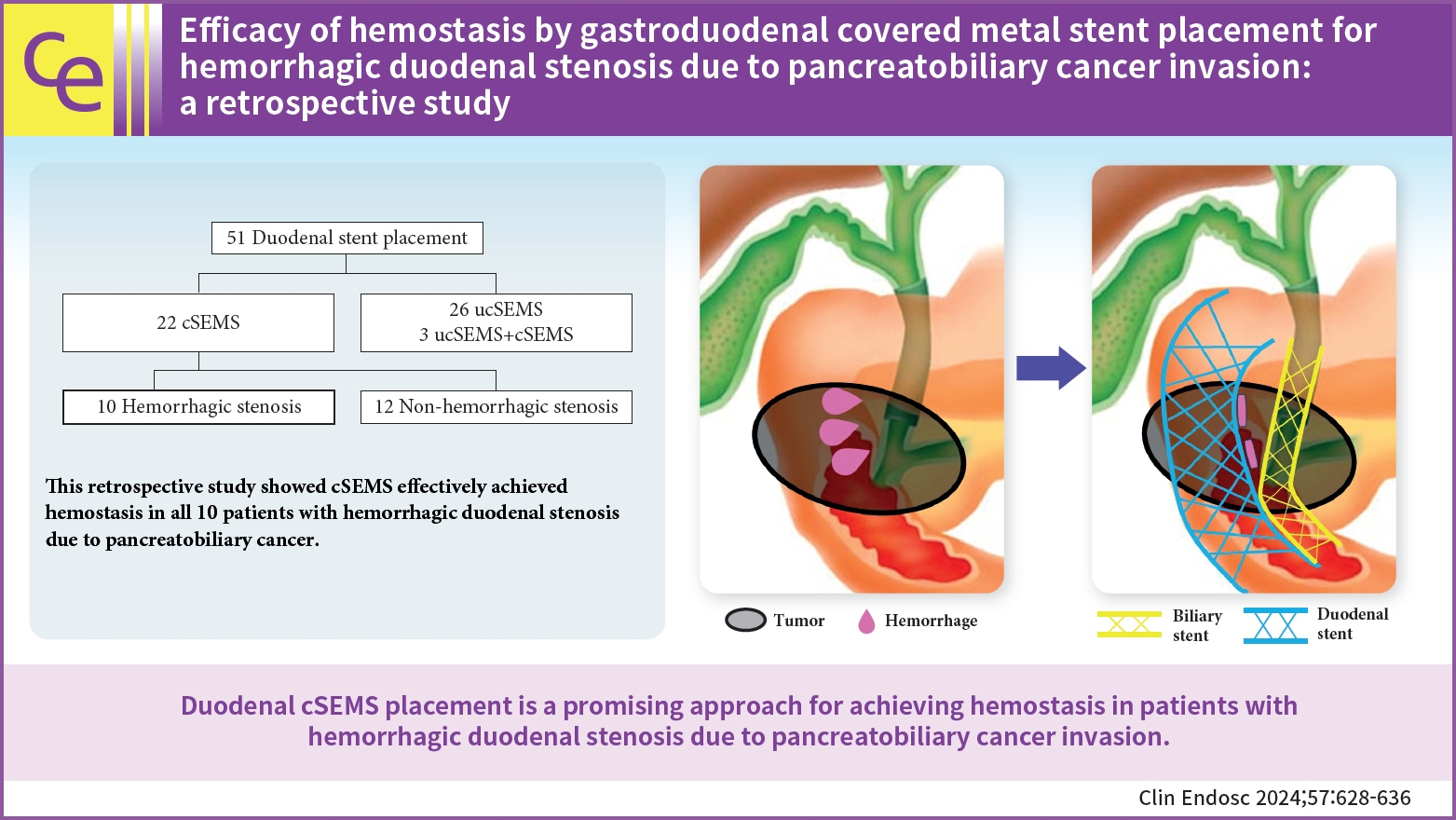
Advanced pancreatic and biliary tract cancers can invade the duodenum and cause duodenal hemorrhagic stenosis. This study aimed to evaluate the efficacy of covered self-expandable metal stents in the treatment of cancer-related duodenal hemorrhage with stenosis.
Methods
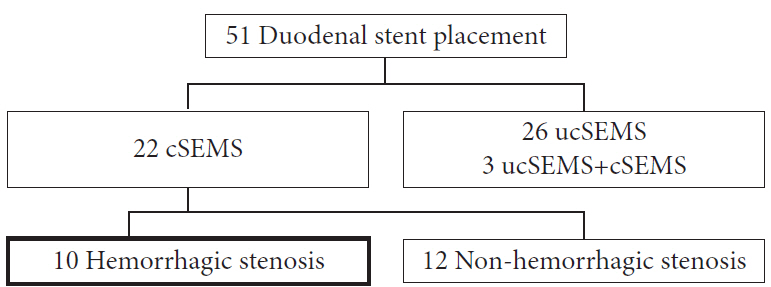
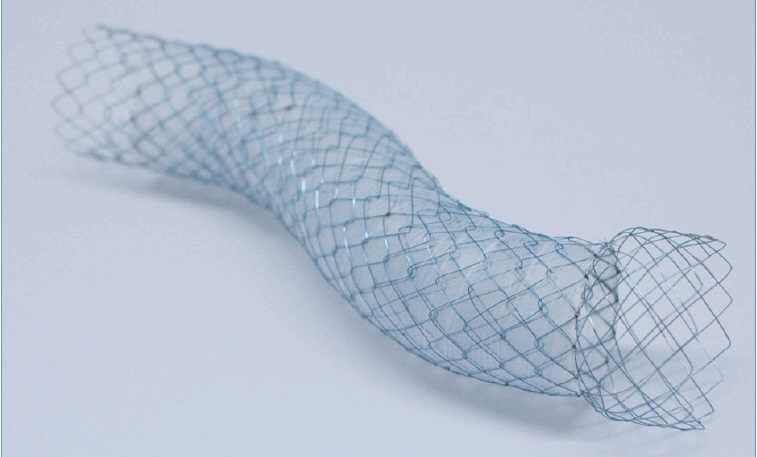
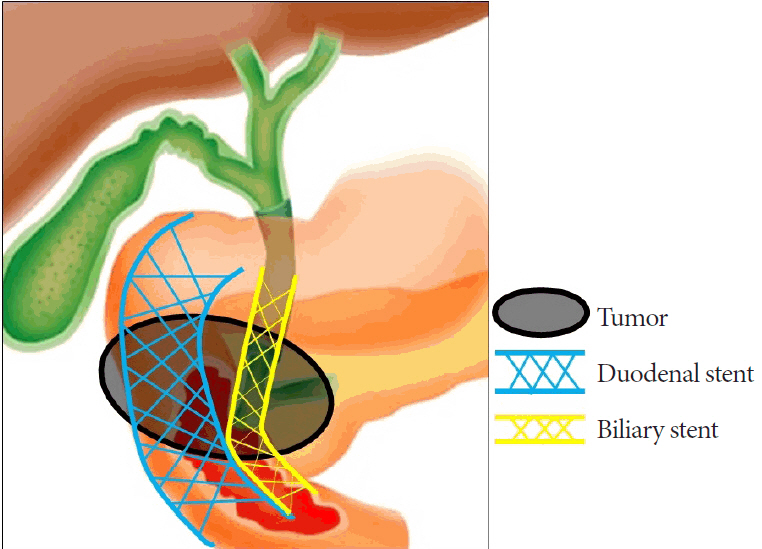
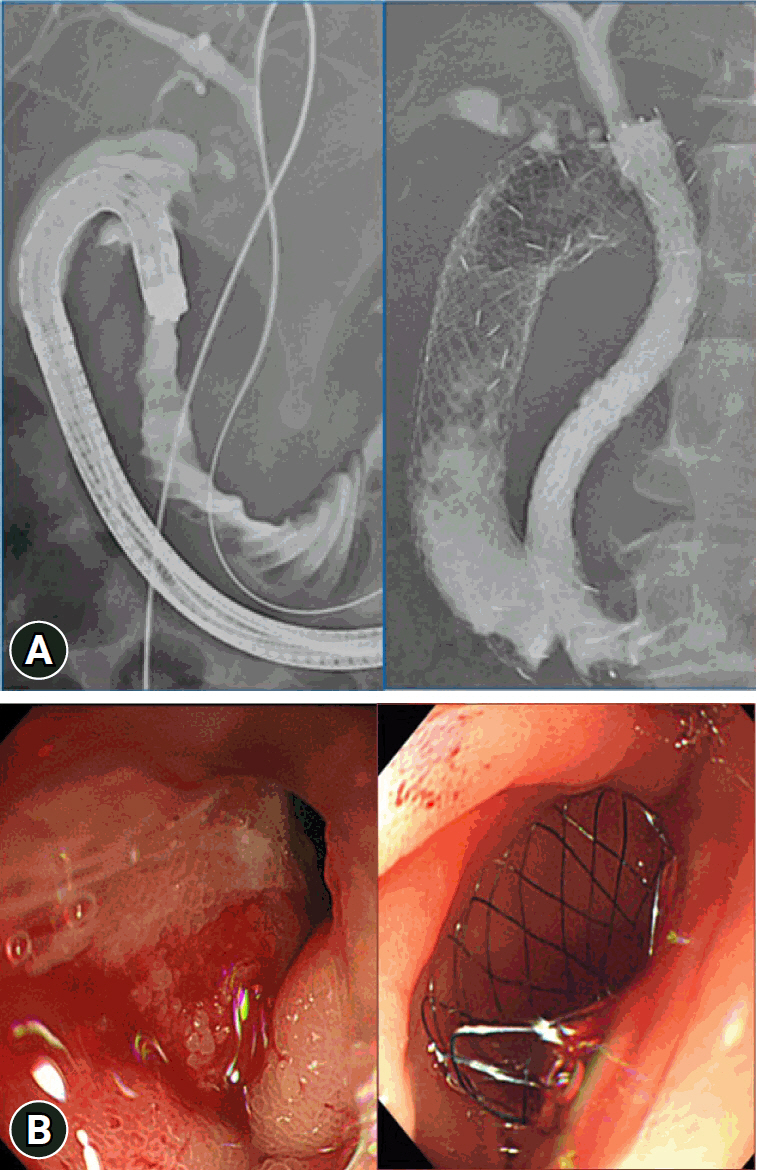
Between January 2014 and December 2016, metal stents were placed in 51 patients with duodenal stenosis. Among these patients, a self-expandable covered metal stent was endoscopically placed in 10 patients with hemorrhagic duodenal stenosis caused by pancreatobiliary cancer progression. We retrospectively analyzed the therapeutic efficacy of the stents by evaluating the technical and clinical success rates based on successful stent placement, degree of oral intake, hemostasis, stent patency, and overall survival.
Results
The technical and clinical success rates were 100%. All 10 patients achieved a gastric outlet obstruction scoring system score of three within two weeks after the procedure and had no recurrence of melena. The median stent patency duration and overall survival after stent placement were 52 days (range, 20–220 days) and 66.5 days (range, 31–220 days), respectively.
Conclusions
Endoscopic placement of a covered metal stent for hemorrhagic duodenal stenosis associated with pancreatic or biliary tract cancer resulted in duodenal hemostasis, recanalization, and improved quality of life.
Keyword
Figure
Reference
-
1. Maire F, Hammel P, Ponsot P, et al. Long-term outcome of biliary and duodenal stents in palliative treatment of patients with unresectable adenocarcinoma of the head of pancreas. Am J Gastroenterol. 2006; 101:735–742.2. Maetani I, Nambu T, Omuta S, et al. Treating bilio-duodenal obstruction: combining new endoscopic technique with 6 Fr stent introducer. World J Gastroenterol. 2010; 16:2828–2831.3. Andtbacka RH, Evans DB, Pisters PW. Surgical and endoscopic palliation for pancreatic cancer. Minerva Chir. 2004; 59:123–136.4. National Comprehensive Cancer Network (NCCN). NCCN clinical plactice guidelines in oncology; pancreatic adenocarcinoma, version 1 [Internet]. NCCN;2023. [cited 2023 May 4]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf.5. D'Souza PM, Sandha GS, Teshima CW. Refractory bleeding from a malignant duodenal ulcer treated with placement of a fully-covered gastroduodenal stent. Dig Dis Sci. 2013; 58:3359–3361.6. Orii T, Karasawa Y, Kitahara H, et al. Efficacy of self-expandable metallic stent inserted for refractory hemorrhage of duodenal cancer. Case Rep Gastroenterol. 2016; 10:151–156.7. Daiku K, Ikezawa K, Maeda S, et al. A case of refractory tumor bleeding from an ampullary adenocarcinoma: compression hemostasis with a self-expandable metallic stent. DEN Open. 2022; 2:e23.8. Subramaniam S, Kandiah K, Chedgy F, et al. A novel self-assembling peptide for hemostasis during endoscopic submucosal dissection: a randomized controlled trial. Endoscopy. 2021; 53:27–35.9. Mutignani M, Tringali A, Shah SG, et al. Combined endoscopic stent insertion in malignant biliary and duodenal obstruction. Endoscopy. 2007; 39:440–447.10. Tonozuka R, Itoi T, Sofuni A, et al. Endoscopic double stenting for the treatment of malignant biliary and duodenal obstruction due to pancreatic cancer. Dig Endosc. 2013; 25 Suppl 2:100–108.11. Maetani I, Isayama H, Mizumoto Y. Palliation in patients with malignant gastric outlet obstruction with a newly designed enteral stent: a multicenter study. Gastrointest Endosc. 2007; 66:355–360.12. Maetani I, Ukita T, Nambu T, et al. Comparison of ultraflex and niti-s stents for palliation of unresectable malignant gastroduodenal obstruction. Dig Endosc. 2010; 22:83–89.13. Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002; 97:72–78.14. Division of Cancer Treatment and Diagnosis (DCTD)/National Cancer Institute (NCI)/National Institutes of Health (NIH)/U.S. Department of Health and Human Services (DHHS). Common toxicity criteria, version 2.0 [Internet]. DCTD/NCI/NIH/DHHS;1999. [cited 2023 Aug 28]. Available from: http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcv20_4-30-992.pdf.15. Itoi T, Yasuda I, Doi S, et al. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011; 43:369–372.16. Lim SG, Kim JH, Lee KM, et al. Conformable covered versus uncovered self-expandable metallic stents for palliation of malignant gastroduodenal obstruction: a randomized prospective study. Dig Liver Dis. 2014; 46:603–608.17. Maetani I, Mizumoto Y, Shigoka H, et al. Placement of a triple-layered covered versus uncovered metallic stent for palliation of malignant gastric outlet obstruction: a multicenter randomized trial. Dig Endosc. 2014; 26:192–199.18. Waidmann O, Trojan J, Friedrich-Rust M, et al. SEMS vs cSEMS in duodenal and small bowel obstruction: high risk of migration in the covered stent group. World J Gastroenterol. 2013; 19:6199–6206.19. Takahara N, Isayama H, Nakai Y, et al. A novel partially covered self-expandable metallic stent with proximal flare in patients with malignant gastric outlet obstruction. Gut Liver. 2017; 11:481–488.20. Yamao K, Kitano M, Chiba Y, et al. Endoscopic placement of covered versus uncovered self-expandable metal stents for palliation of malignant gastric outlet obstruction. Gut. 2021; 70:1244–1252.21. Kim CG, Choi IJ, Lee JY, et al. Covered versus uncovered self-expandable metallic stents for palliation of malignant pyloric obstruction in gastric cancer patients: a randomized, prospective study. Gastrointest Endosc. 2010; 72:25–32.22. Oh D, Lee SS, Song TJ, et al. Efficacy and safety of a partially covered duodenal stent for malignant gastroduodenal obstruction: a pilot study. Gastrointest Endosc. 2015; 82:32–36.23. Woo SM, Kim DH, Lee WJ, et al. Comparison of uncovered and covered stents for the treatment of malignant duodenal obstruction caused by pancreaticobiliary cancer. Surg Endosc. 2013; 27:2031–2039.24. Kim JW, Jeong JB, Lee KL, et al. Comparison between uncovered and covered self-expandable metal stent placement in malignant duodenal obstruction. World J Gastroenterol. 2015; 21:1580–1587.25. Kaw M, Singh S, Gagneja H. Clinical outcome of simultaneous self-expandable metal stents for palliation of malignant biliary and duodenal obstruction. Surg Endosc. 2003; 17:457–461.26. Kim KO, Kim TN, Lee HC. Effectiveness of combined biliary and duodenal stenting in patients with malignant biliary and duodenal obstruction. Scand J Gastroenterol. 2012; 47:962–967.27. Maetani I, Ogawa S, Hoshi H, et al. Self-expanding metal stents for palliative treatment of malignant biliary and duodenal stenoses. Endoscopy. 1994; 26:701–704.28. Profili S, Feo CF, Meloni GB, et al. Combined biliary and duodenal stenting for palliation of pancreatic cancer. Scand J Gastroenterol. 2003; 38:1099–1102.29. Moon JH, Choi HJ, Ko BM, et al. Combined endoscopic stent-in-stent placement for malignant biliary and duodenal obstruction by using a new duodenal metal stent (with videos). Gastrointest Endosc. 2009; 70:772–777.30. Kim ET, Gwon DI, Kim JW, et al. Acute pancreatitis after percutaneous insertion of metallic biliary stents in patients with unresectable pancreatic cancer. Clin Radiol. 2020; 75:57–63.31. Sugawara S, Arai Y, Sone M, et al. Frequency, severity, and risk factors for acute pancreatitis after percutaneous transhepatic biliary stent placement across the papilla of vater. Cardiovasc Intervent Radiol. 2017; 40:1904–1910.32. Yang Y, Liu RB, Liu Y, et al. Incidence and risk factors of pancreatitis in obstructive jaundice patients after percutaneous placement of self-expandable metallic stents. Hepatobiliary Pancreat Dis Int. 2020; 19:473–477.33. Zu QQ, Zhang JX, Wang B, et al. Percutaneous transpapillary biliary stent placement for distal malignant biliary obstruction: outcomes and survival analysis. Turk J Gastroenterol. 2019; 30:714–721.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Simultaneous Duodenal Metal Stent Placement and EUS-Guided Choledochoduodenostomy for Unresectable Pancreatic Cancer
- Biliary Stent Placement for the Management of Acute Obstructive Jaundice after Uncovered Gastroduodenal Stent Placement
- Practical Experiences of Unsuccessful Hemostasis with Covered Self-Expandable Metal Stent Placement for Post-Endoscopic Sphincterotomy Bleeding
- Percutaneous Transgastric Stent Placement for Malignant Gastroduodenal Obstruction
- Treatment of Malignant Gastroduodenal Obstruction with Using a Newly Designed Complex Expandable Nitinol Stent: Initial Experiences