Clin Endosc.
2022 Jan;55(1):128-135. 10.5946/ce.2021.057.
Biliary Self-Expandable Metal Stent Could Be Recommended as a First Treatment Modality for Immediate Refractory Post-Endoscopic Retrograde Cholangiopancreatography Bleeding
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea
- 2School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2525059
- DOI: http://doi.org/10.5946/ce.2021.057
Abstract
- Background/Aims
Recent reports suggest that the biliary self-expandable metallic stent (SEMS) is highly effective for maintaining hemostasis when endoscopic hemostasis fails in endoscopic retrograde cholangiopancreatography (ERCP)-related bleeding. We compared whether temporary SEMS offers better efficacy than angioembolization for refractory immediate ERCP-related bleeding.
Methods
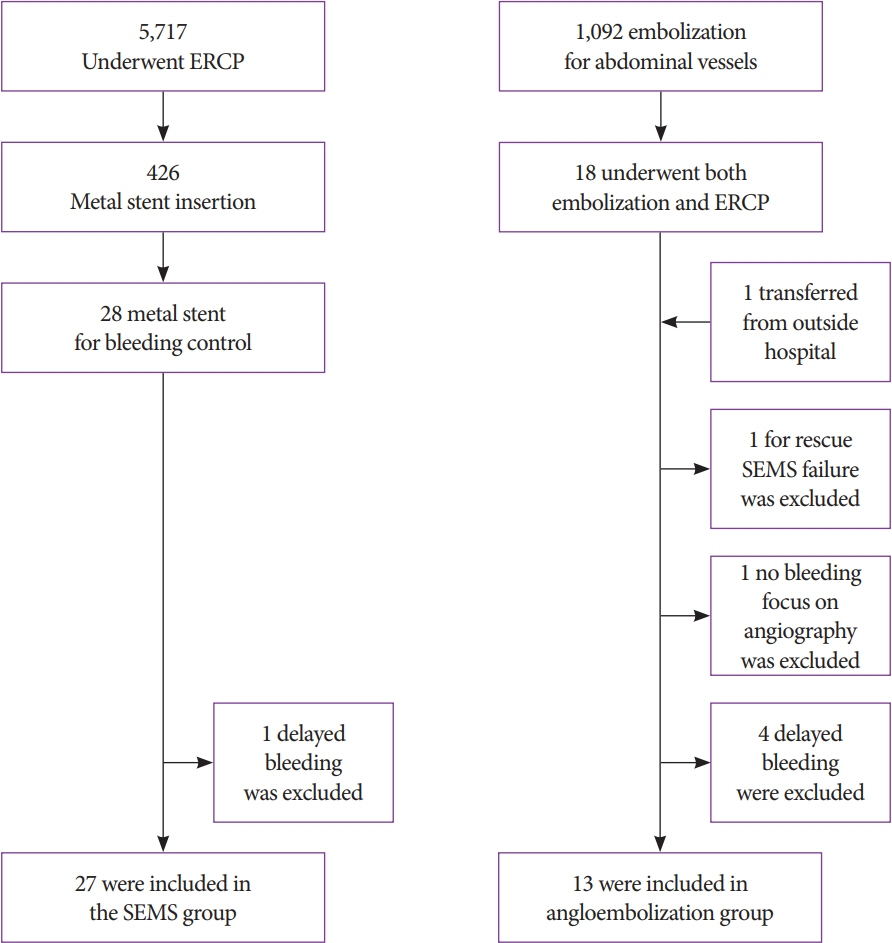
Patients who underwent SEMS placement or underwent angioembolization for bleeding control in refractory immediate ERCP-related bleeding were included in the retrospective analysis. We evaluated the hemostasis success rate, severity of bleeding, change in hemoglobin levels, amount of transfusion, and delay to the start of hemostasis.
Results
A total of 27 patients with SEMS and 13 patients who underwent angioembolization were enrolled. More transfusions were needed in the angioembolization group (1.0±1.4 units vs. 2.5±2.0 units; p=0.034). SEMS failure was successfully rescued by angioembolization. The partially covered SEMS (n=23, 85.1%) was generally used, and the median stent-indwelling time was 4 days. The mean delay to the start of angioembolization was 95.2±142.9 (range, 9–491) min.
Conclusions
Temporary SEMS had similar results to those of angioembolization (96.3% vs. 92.3%; p=0.588). Immediate SEMS insertion is considered a bridge treatment modality for immediate refractory ERCP-related bleeding. Angioembolization still has a role as rescue therapy when SEMS does not work effectively.
Keyword
Figure
Reference
-
1. Dumonceau JM, Kapral C, Aabakken L, et al. ERCP-related adverse events: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2020; 52:127–149.2. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.3. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393.4. Ferreira LE, Baron TH. Post-sphincterotomy bleeding: who, what, when, and how. Am J Gastroenterol. 2007; 102:2850–2858.5. Wilcox CM, Canakis J, Mönkemüller KE, Bondora AW, Geels W. Patterns of bleeding after endoscopic sphincterotomy, the subsequent risk of bleeding, and the role of epinephrine injection. Am J Gastroenterol. 2004; 99:244–248.6. Rustagi T, Jamidar PA. Endoscopic retrograde cholangiopancreatography-related adverse events: general overview. Gastrointest Endosc Clin N Am. 2015; 25:97–106.7. Canena J, Liberato M, Horta D, Romão C, Coutinho A. Short-term stenting using fully covered self-expandable metal stents for treatment of refractory biliary leaks, postsphincterotomy bleeding, and perforations. Surg Endosc. 2013; 27:313–324.8. So YH, Choi YH, Chung JW, Jae HJ, Song SY, Park JH. Selective embolization for post-endoscopic sphincterotomy bleeding: technical aspects and clinical efficacy. Korean J Radiol. 2012; 13:73–81.9. Dunne R, McCarthy E, Joyce E, et al. Post-endoscopic biliary sphincterotomy bleeding: an interventional radiology approach. Acta Radiol. 2013; 54:1159–1164.10. Maleux G, Bielen J, Laenen A, et al. Embolization of post-biliary sphincterotomy bleeding refractory to medical and endoscopic therapy: technical results, clinical efficacy and predictors of outcome. Eur Radiol. 2014; 24:2779–2786.11. Shah JN, Marson F, Binmoeller KF. Temporary self-expandable metal stent placement for treatment of post-sphincterotomy bleeding. Gastrointest Endosc. 2010; 72:1274–1278.12. Itoi T, Yasuda I, Doi S, Mukai T, Kurihara T, Sofuni A. Endoscopic hemostasis using covered metallic stent placement for uncontrolled post-endoscopic sphincterotomy bleeding. Endoscopy. 2011; 43:369–372.13. Chandrasekhara V, Khashab MA, Muthusamy VR, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017; 85:32–47.14. Behm B, Brock A, Clarke BW, et al. Partially covered self-expandable metallic stents for benign biliary strictures due to chronic pancreatitis. Endoscopy. 2009; 41:547–551.15. Schmidt A, Pickartz T, Lerch MM, et al. Effective treatment of benign biliary strictures with a removable, fully covered, self-expandable metal stent: a prospective, multicenter European study. United European Gastroenterol J. 2017; 5:398–407.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Successful Treatment of Chronic Cholecystitis with SpyGlass Cholangioscopy-Assisted Gallbladder Drainage and Irrigation through Self-Expandable Metal Stents
- Practical Experiences of Unsuccessful Hemostasis with Covered Self-Expandable Metal Stent Placement for Post-Endoscopic Sphincterotomy Bleeding
- Mechanisms of Biliary Plastic Stent Occlusion and Efforts at Prevention
- Can Endoscopic Ultrasonography-guided Biliary Drainage Using Self-expandable Metal Stents in Malignant Distal Biliary Obstruction Be a Substitute When Endoscopic Retrograde Cholangiopancreatography Has Failed?
- Spontaneous Common Bile Duct Perforation Treated with Placement of Metal Stent