Child Kidney Dis.
2021 Dec;25(2):78-83. 10.3339/jkspn.2021.25.2.78.
Spot Urine Uric Acid to Creatinine Ratio used in the Estimation of Hyperuricosuria in the Young Korean Population
- Affiliations
-
- 1Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Ganwon-do, Republic of Korea
- KMID: 2524509
- DOI: http://doi.org/10.3339/jkspn.2021.25.2.78
Abstract
- Background
Uric acid levels in urine are measured using urine specimens 24 hours or by uric acid glomerular filtration rate (UAGFR) with spot urine, which additionally requires a blood sample. This study aimed to investigate whether urinary uric acid creatinine ratio (UUACr) obtained by spot urine alone could be recognized as a substitute for UAGFR value, and hyperuricosuria can be screened by UUACr. UUACr is known to vary with age and regional differences. This study focused on the reference value of each value in Korean young populations. Method: We enrolled Korean subjects 1–20 years with normal kidney function, from a single hospital, classified into 5 age groups, 1–5 years, 6–8 years, 9–12 years, 13–15 years, and 16–20 years. We checked spot urine uric acid, creatinine and serum uric acid, creatinine levels on the same day from February 2014 to December 2018. We measured the average of UAGFR and UUACr in each groups. The UUACr cut-off value of the upper 2 standard deviation (SD) of UAGFR were taken.
Results
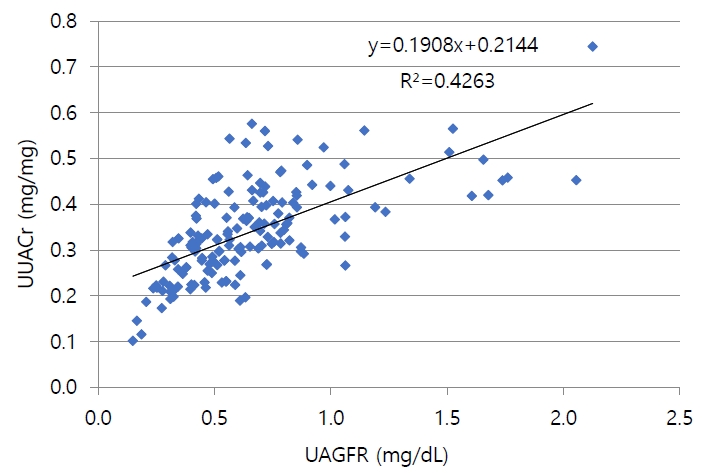
The upper 2 SD of UUACr (mg/mg) and UAGFR (mg/dL) were determined in all age groups. UUACr decreased with grown up (P=0.000), but UAGFR were not statistically different among the groups. UUACr and UAGFR were not significantly different by gender. UUACr and UAGFR were positively correlated; UUACr cut-off value of upper 2 SD UAGFR (0.54 mg/dL) was 0.65 mg/mg in total age.
Conclusions
UUACr could potentially be used to screen for hyperuricosuria.
Keyword
Figure
Reference
-
References
1. Arrabal-Polo MA, Cano-Garcia MDC, Arrabal-Martin M. Lithogenic activity as a factor to consider in the metabolic evaluation of patients with calcium lithiasis. Iran J Kidney Dis. 2015; 9:469–7.2. Cillo AC, Cattini H, Boim MA, Schor N. Evaluation of lithogenic elements in urine of healthy newborns. Pediatr Nephrol. 2001; 16:1080–3.
Article3. Hartung R. The significance of uric acid in calcium oxalate nephrolithiasis. MMW. 1975; 117:387–90.4. La Manna A, Polito C, Marte A, Iovene A, Di Toro R. Hyperuricosuria in children: clinical presentation and natural history. Pediatrics. 2001; 107:86–90.
Article5. Hodgkinson A. Uric acid disorders in patients with calcium stones. Br J Urol. 1976; 48:1–5.6. Stapleton FB. Hematuria associated with hypercalciuria and hyperuricosuria: a practical approach. Pediatr Nephrol. 1994; 8:756–61.
Article7. Stapleton FB, Linshaw MA, Hassanein K, Gruskin AB. Uric acid excretion in normal children. J Pediatr. 1978; 92:911–4.
Article8. Stapleton FB, Nash DA. A screening test for hyperuricosuria. J Pediatr. 1983; 102:88–90.
Article9. Chen YH, Lee AJ, Chen CH, Chesney RW, Stapleton FB, Roy S. Urinary mineral excretion among normal Taiwanese children. Pediatr Nephrol. 1994; 8:36–9.
Article10. Safarinejad MR. Urinary mineral excretion in healthy Iranian children. Pediatr Nephrol. 2003; 18:140–4.
Article11. Kompani F, Gaedi Z, Ahmadzadeh A, Seyedzadeh A, Bahadoram M. Values of urinary mineral excretion in healthy Iranian. J Ped Nephrol. 2015; 3:26–30.12. Marco RH, Gómez FN, Costa CM, Moreno JF, Vidal AP, Solanes JB. Excreción urinaria de calcio, magnesio, ácido úrico y ácido oxálico en niños normales [Urinary excretion of calcium, magnesium, uric acid and oxalic acid in normal children]. An Esp Pediatr. 1988; 29:99–104.13. Matos V, Van Melle G, Werner D, Bardy D, Guignard JP. Urinary oxalate and urate to creatinine ratios in a healthy pediatric population. Am J Kidney Dis. 1999; 34:e1.
Article14. Öner A, Erdogan Ö, Çamurdanoglu D, Demircin G, Bülbül M, Delibas A. Reference values for urinary calcium and uric acid excretion in healthy Turkish children. Int Pediatr. 2004; 19:154–7.15. Poyrazoğlu HM, Düşünsel R, Yazici C, Durmaz H, Dursun I, Şahin H, et al. Urinary uric acid : Creatinine ratios in healthy Turkish children. Pediatr Int. 2009; 51:526–9.
Article16. Sweid HA, Bagga A, Vaswani M, Vasudev V, Ahuja RK, Srivastava RN. Urinary excretion of minerals, oxalate, and uric acid in north Indian children. Pediatr Nephrol. 1997; 11:189–92.
Article17. Moriwaki Y, Yamamoto T, Takahashi S, Yamakita J, Tsutsumi Z, Hada T. Spot urine uric acid to creatinine ratio used in the estimation of uric acid excretion in primary gout. J Rheumatol. 2001; 28:1306–10.18. Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, et al. Standard 6: age groups for pediatric trials. Pediatrics. 2012; 129:S153–60.
Article19. Baldree LA, Stapleton FB. Uric Acid Metabolism in Children. Pediatr Clin North Am. 1990; 37:391–418.
Article20. Mantani N, Hoshino A, Ito K, Kogure T, Moridaira K, Sakamoto H, et al. Relationships among urine pH, serum uric acid and pyuria in hospitalized elderly patients. Nihon Ronen Igakkai Zasshi. 2004; 41:542–555.
Article21. Grivna M, Průsa R, Janda J. Urinary uric acid excretion in healthy male infants. Pediatr Nephrol. 1997; 11:623–4.
Article22. Penido MG, Diniz JS, Guimarães MM, Cardoso RB, Souto MF, Penido MG. Urinary excretion of calcium, uric acid and citrate in healthy children and adolescents. J Pediatr (Rio J). 2002; 78:153–60.
Article23. Hasday JD. Noctural increase of urinary uric acid:creatinine ratio. A biochemical correlate of sleep-associated hypoxemia. Am Rev Respir Dis. 1987; 134:534–8.24. Kaufman JM, Greene ML, Seegmiller JE. Urine uric acid to creatinine ratio-a screening test for inherited disorders of purine metabolism. Phosphoribosyltransferase (PRT) deficiency in X-linked cerebral palsy and in a variant of gout. J Pediatr. 1968; 73:583–92.25. Zöllner N. Influence of various purines on uric acid metabolism. Bibl Nutr Dieta. 1973; 34:43.
Article26. Daniel CR, Cross AJ, Koebnick C, Sinha R. Trends in meat consumption in the USA. Public Health Nutr. 2011; 14:575–83.
Article27. Welfare MoHa. The Korean Nutrition Society. Dietary reference intakes for Koreans 2020. In : . Sejong: 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Update on pathogenesis of uric acid nephrolithiasis
- The Utility of the Random Urine Uric Acid-to-Creatinine Ratio for Patients with Gout Who Need Uricosuric Agents: Retrospective Cross-Sectional Study
- Clinical Usefulness of Uric Acid as a Biomarker for Knee Osteoarthritis: A Comparative Analysis With Plain Radiography and Musculoskeletal Ultrasound
- Cloudy urine developed during total intravenous anesthesia with 2% propofol in the patient taking hydroxyurea: A case report
- A Study on the Validity of Filter Paper Method in Estimation of the Amount of Daily Salt Intake