Prog Med Phys.
2021 Dec;32(4):99-106. 10.14316/pmp.2021.32.4.99.
Dosimetric Study Using Patient-Specific ThreeDimensional-Printed Head Phantom with Polymer Gel in Radiation Therapy
- Affiliations
-
- 1Research Team of Radiological Physics & Engineering, Korea Institute of Radiological and Medical Science, Seoul, Korea
- 2Department of Accelerator Science, Korea University, Sejong, Korea
- 3Divisions of Applied RI , Korea Institute of Radiological and Medical Science, Seoul, Korea
- 4Divisions of Applied Radiation Bioscience, Korea Institute of Radiological and Medical Science, Seoul, Korea
- KMID: 2524155
- DOI: http://doi.org/10.14316/pmp.2021.32.4.99
Abstract
- Purpose
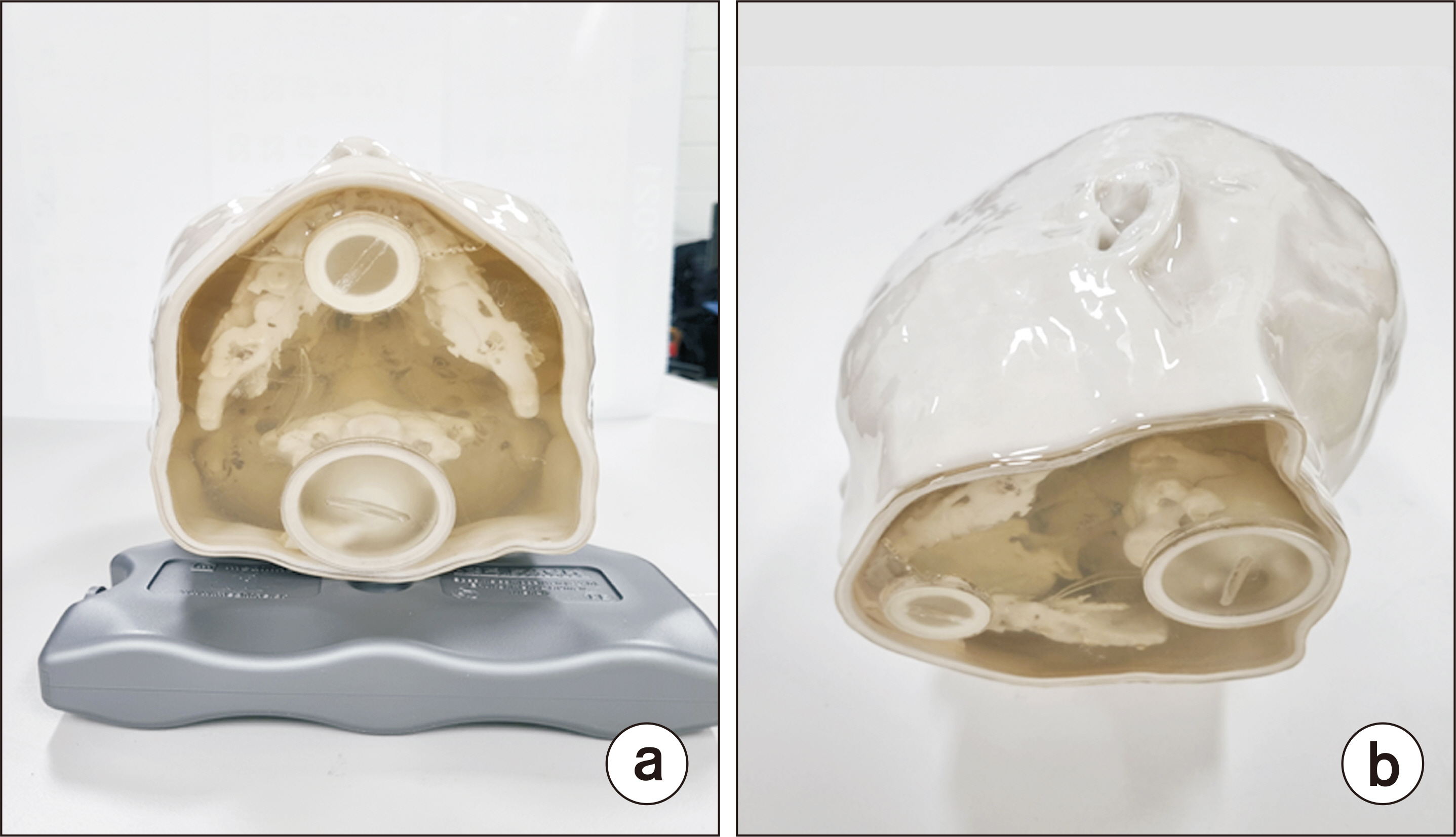
In this study, we aimed to manufacture a patient-specific gel phantom combining threedimensional (3D) printing and polymer gel and evaluate the radiation dose and dose profile using gel dosimetry.
Methods
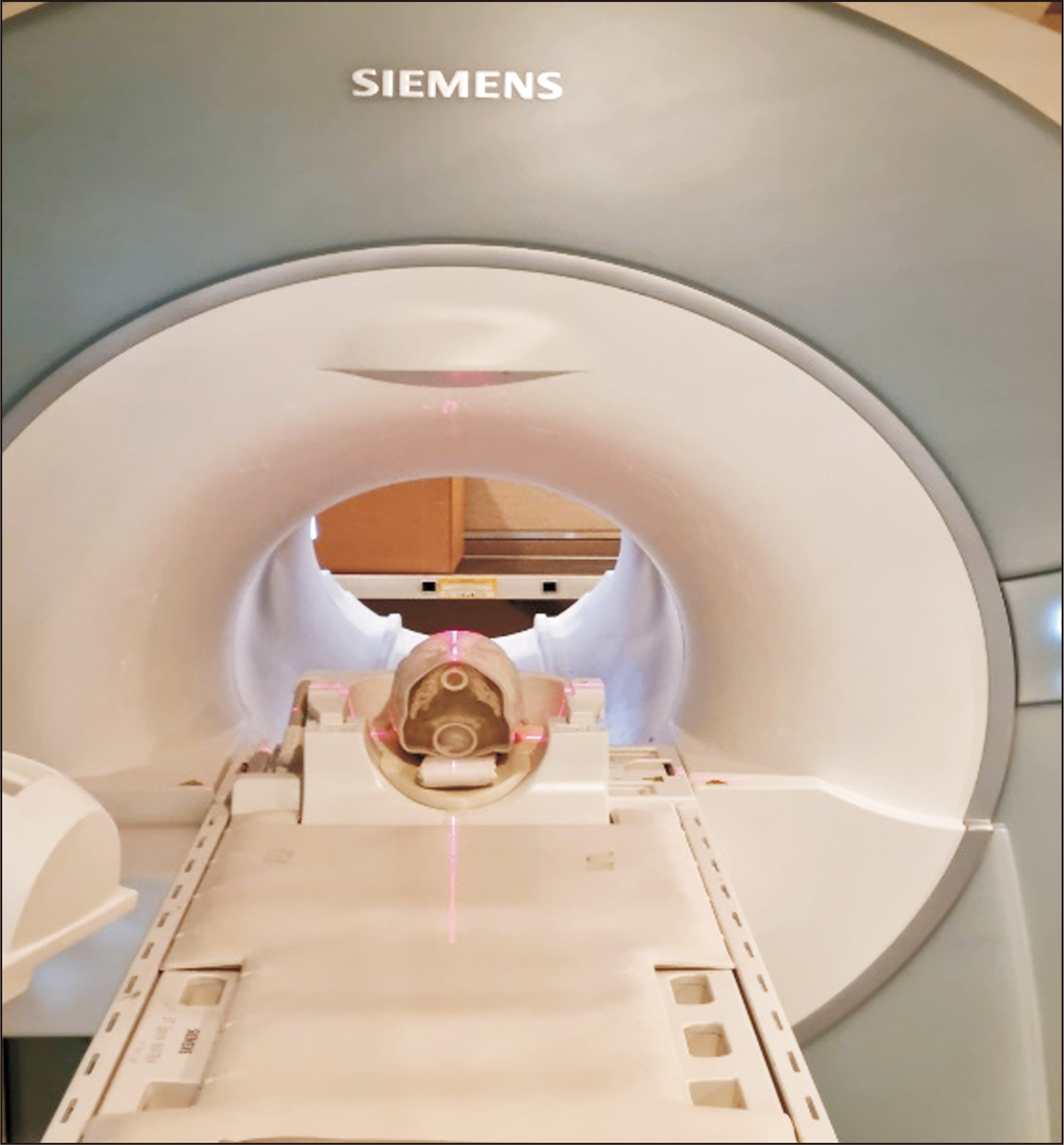
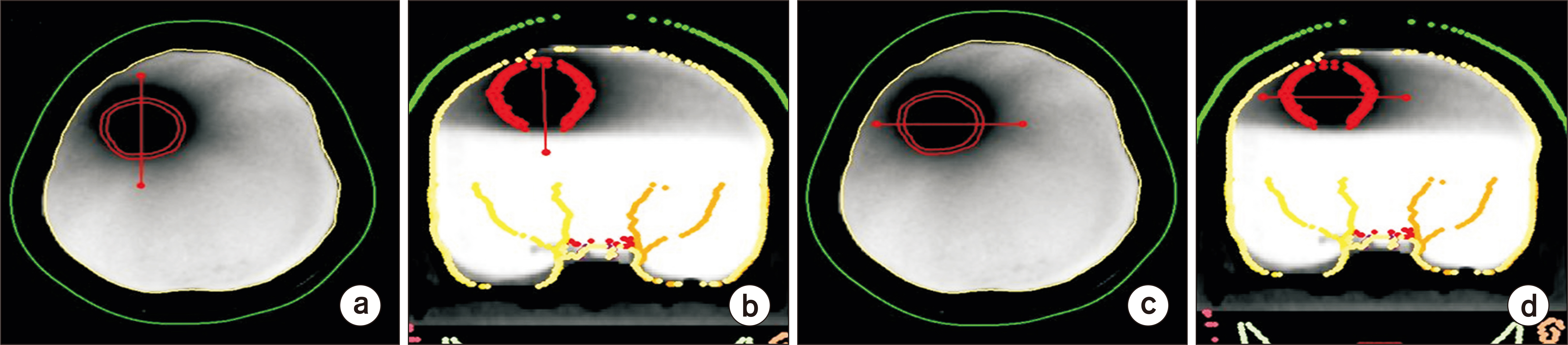
The patient-specific head phantom was manufactured based on the patient’s computed tomography (CT) scan data to create an anatomically replicated phantom; this was then produced using a ColorJet 3D printer. A 3D polymer gel dosimeter called RTgel-100 is contained inside the 3D printing head phantom, and irradiation was performed using a 6 MV LINAC (Varian Clinac) X-ray beam, a linear accelerator for treatment. The irradiated phantom was scanned using magnetic resonance imaging (Siemens) with a magnetic field of 3 Tesla (3T) of the Korea Institute of Nuclear Medicine, and then compared the irradiated head phantom with the dose calculated by the patient's treatment planning system (TPS).
Results
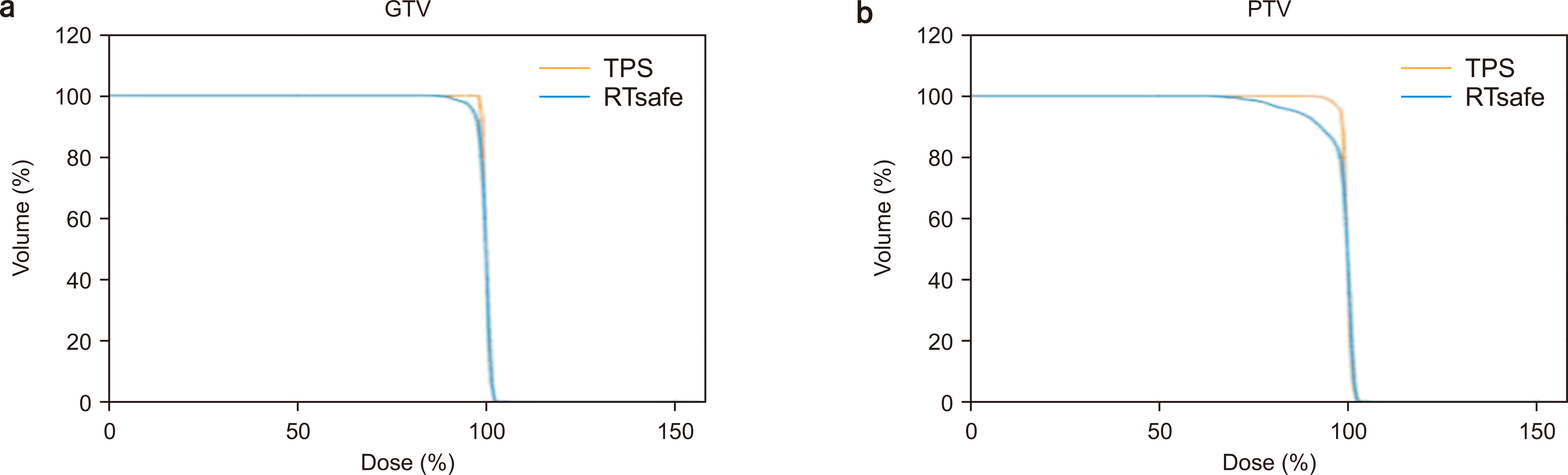
The comparison between the Hounsfield unit (HU) values of the CT image of the patient and those of the phantom revealed that they were almost similar. The electron density value of the patient’s bone and brain was 996±167 HU and 58±15 HU, respectively, and that of the head phantom bone and brain material was 986±25 HU and 45±17 HU, respectively. The comparison of the data of TPS and 3D gel revealed that the difference in gamma index was 2%/2 mm and the passing rate was within 95%.
Conclusions
3D printing allows us to manufacture variable density phantoms for patient-specific dosimetric quality assurance (DQA), develop a customized body phantom of the patient in the future, and perform a patient-specific dosimetry with film, ion chamber, gel, and so on.
Keyword
Figure
Reference
-
References
1. Ezzell GA, Galvin JM, Low D, Palta JR, Rosen I, Sharpe MB, et al. 2003; Guidance document on delivery, treatment planning, and clinical implementation of IMRT: report of the IMRT Subcommittee of the AAPM Radiation Therapy Committee. Med Phys. 30:2089–2115. DOI: 10.1118/1.1591194. PMID: 12945975.
Article2. Chin LS, Regine WF. 2010. Principles and practice of stereotactic radiosurgery. Springer Science+Business Media;New York:3. Park HJ, Griffin RJ, Hui S, Levitt SH, Song CW. 2012; Radiation-induced vascular damage in tumors: implications of vascular damage in ablative hypofractionated radiotherapy (SBRT and SRS). Radiat Res. 177:311–327. DOI: 10.1667/RR2773.1. PMID: 22229487.
Article4. Gigliotti MJ, Hasan S, Liang Y, Chen D, Fuhrer R, Wegner RE. 2018; A 10-year experience of linear accelerator-based stereotactic radiosurgery/radiotherapy (SRS/SRT) for paraganglioma: a single institution experience and review of the literature. J Radiosurg SBRT. 5:183–190.5. Kry SF, Molineu A, Kerns JR, Faught AM, Huang JY, Pulliam KB, et al. 2014; Institutional patient-specific IMRT QA does not predict unacceptable plan delivery. Int J Radiat Oncol Biol Phys. 90:1195–1201. DOI: 10.1016/j.ijrobp.2014.08.334. PMID: 25442044. PMCID: PMC4276500.
Article6. Hillman Y, Kim J, Chetty I, Wen N. 2018; Refinement of MLC modeling improves commercial QA dosimetry system for SRS and SBRT patient-specific QA. Med Phys. 45:1351–1359. DOI: 10.1002/mp.12808. PMID: 29431865.
Article7. Kim JS, Park BR, Yoo J, Ha WH, Jang S, Jang WI, et al. 2021; Measurement uncertainty analysis of radiophotoluminescent glass dosimeter reader system based on GD-352M for estimation of protection quantity. Nucl Eng Technol. DOI: 10.1016/j.net.2021.08.016.
Article8. Molazadeh M, Robatjazi M, Geraily G, Rezaeejam H, Zeinali A, Shirazi A. 2021; Three-dimensional IMRT QA of Monte Carlo and full scatter convolution algorithms based on 3D film dosimetry. Radiat Phys Chem. 186:109528. DOI: 10.1016/j.radphyschem.2021.109528.
Article9. Choi JW, Choi JY, Kim BC, Joo KK. 2021; Feasibility study of a portable and fast spatial dosimeter using an alcohol-based liquid scintillator and a digital camera. J Korean Phys Soc. 79:810–817. DOI: 10.1007/s40042-021-00306-9.
Article10. Eidi T, Aghamiri SMR, Jaberi R, Baghani HR. 2022; On measuring the 3D dose distribution for notched and circular Ru-106 plaque shapes through Gafchromic film dosimetry approach. Radiat Phys Chem. 190:109792. DOI: 10.1016/j.radphyschem.2021.109792.
Article11. Silveira MA, Pavoni JF, Baffa O. 2017; Three-dimensional quality assurance of IMRT prostate plans using gel dosimetry. Phys Med. 34:1–6. DOI: 10.1016/j.ejmp.2016.12.007. PMID: 28108100.
Article12. Lee M, Noh S, Yoon KJ, Lee SW, Yoon SM, Jung J, et al. 2020; Feasibility study of polymer gel dosimetry using a 3D printed phantom for liver cancer radiotherapy. J Korean Phys Soc. 76:453–457. DOI: 10.3938/jkps.76.453.
Article13. Matrosic CK, Holmes S, Bednarz B, Culberson W. 2019; Evaluation of a clinical dose accumulation algorithm using deformable gel dosimetry. J Phys Conf Ser. 1305:012002. DOI: 10.1088/1742-6596/1305/1/012002.
Article14. Baldock C, De Deene Y, Doran S, Ibbott G, Jirasek A, Lepage M, et al. 2010; Polymer gel dosimetry. Phys Med Biol. 55:R1–R63. DOI: 10.1088/0031-9155/55/5/R01. PMID: 20150687. PMCID: PMC3031873.
Article15. Pérez P, Torres PR, Bruna A, Brunetto M, Aon E, Franco D, et al. 2021; Fricke gel xylenol orange dosimeter layers for stereotactic radiosurgery: a preliminary approach. Appl Radiat Isot. 178:109936. DOI: 10.1016/j.apradiso.2021.109936. PMID: 34592691.
Article16. Hebb AO, Poliakov AV. 2009; Imaging of deep brain stimulation leads using extended Hounsfield unit CT. Stereotact Funct Neurosurg. 87:155–160. DOI: 10.1159/000209296. PMID: 19321968.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three-Dimensional Dosimetry Using Magnetic Resonance Imaging of Polymer Gel
- Characteristics of CCD Based Optical CT Scanner for Therapeutic Radiation Dosimetry
- Dosimetric Accuracy of CyberKnife Stereotactic Radiosurgery for Perioptic Lesions
- 3-Dimensional Dosimetry of Small Field Photon Beam
- Preliminary Study for Dosimetry of Boron Neutron Capture Therapy with Polymer Gel