Blood Res.
2021 Dec;56(4):215-228. 10.5045/br.2021.2021094.
Effects and treatment applications of polymeric nanoparticles on improving plateletsÊ storage time: a review of the literature from 2010 to 2020
- Affiliations
-
- 1Blood Transfusion Research Center, High Institute for Research and Education in Transfusion Medicine, Tehran, Iran
- 2Pediatric Congenital Hematologic Disorders Research Center, Shahid Beheshti University of Medical Sciences and Iran Blood Transfusion Organization, Tehran, Iran
- KMID: 2524071
- DOI: http://doi.org/10.5045/br.2021.2021094
Abstract
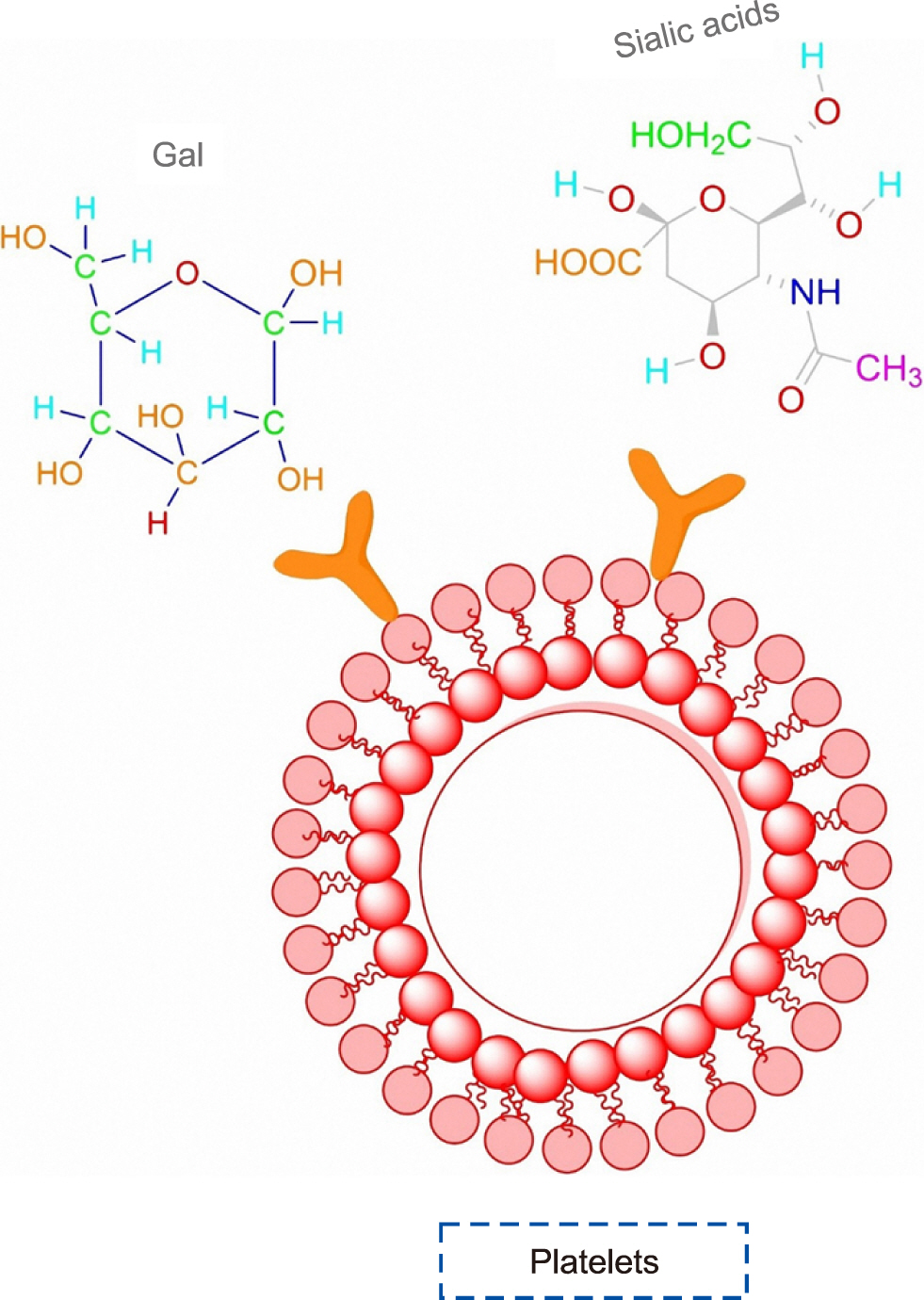
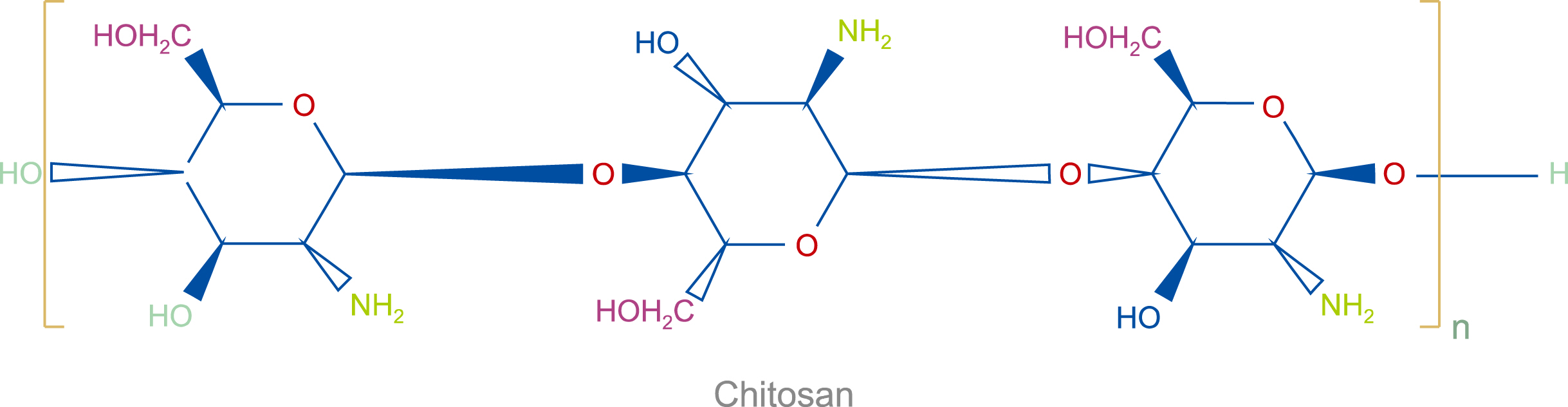
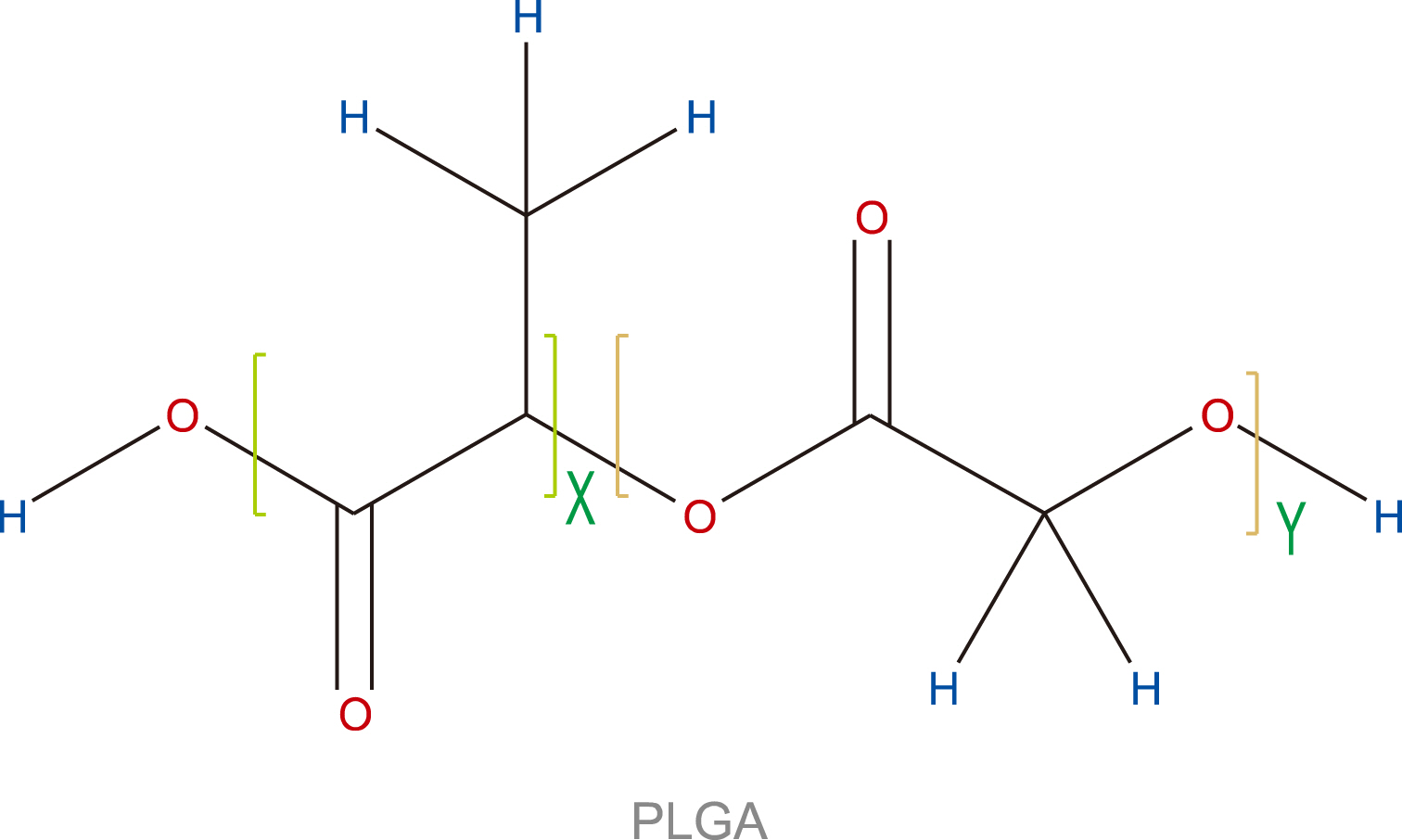
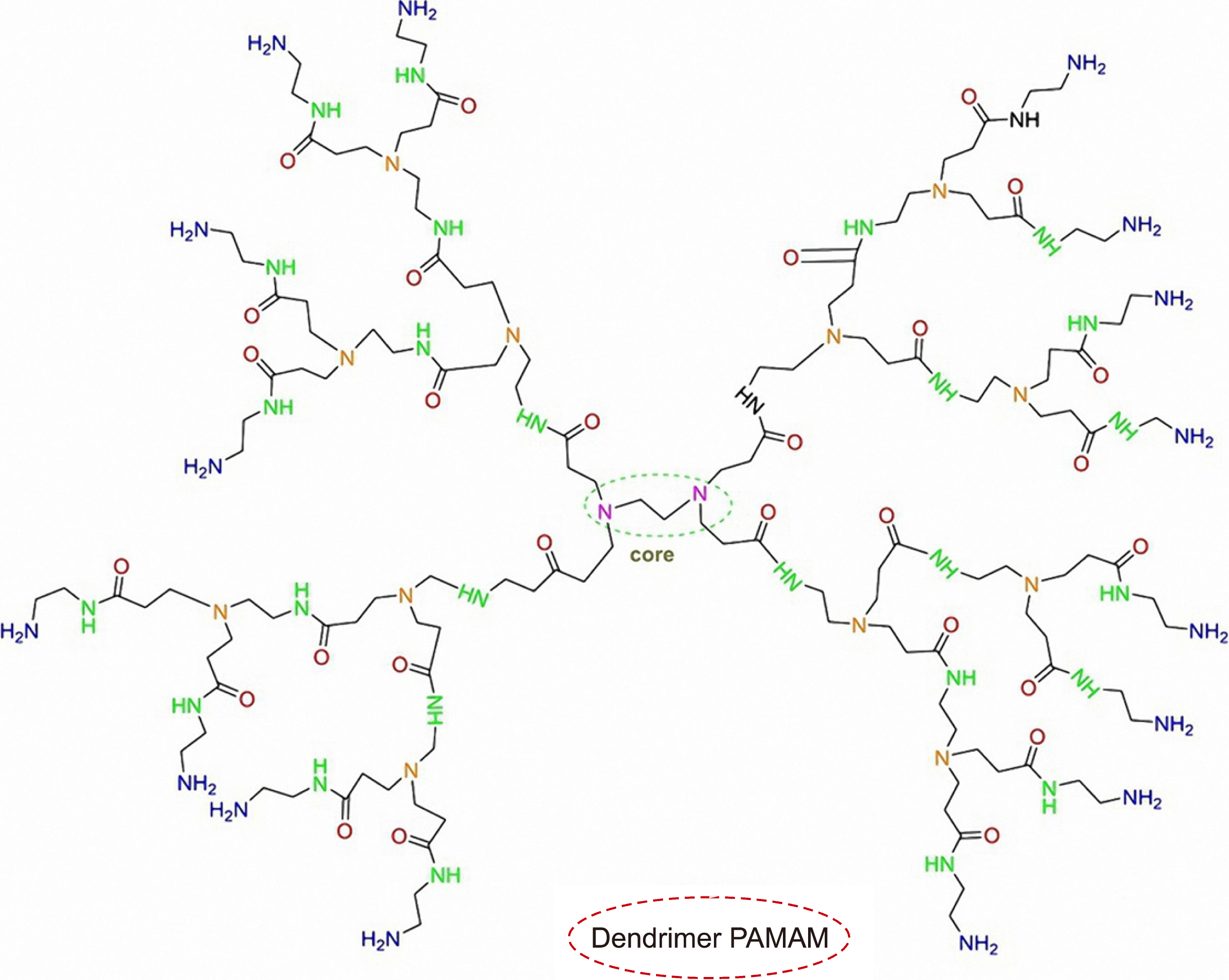
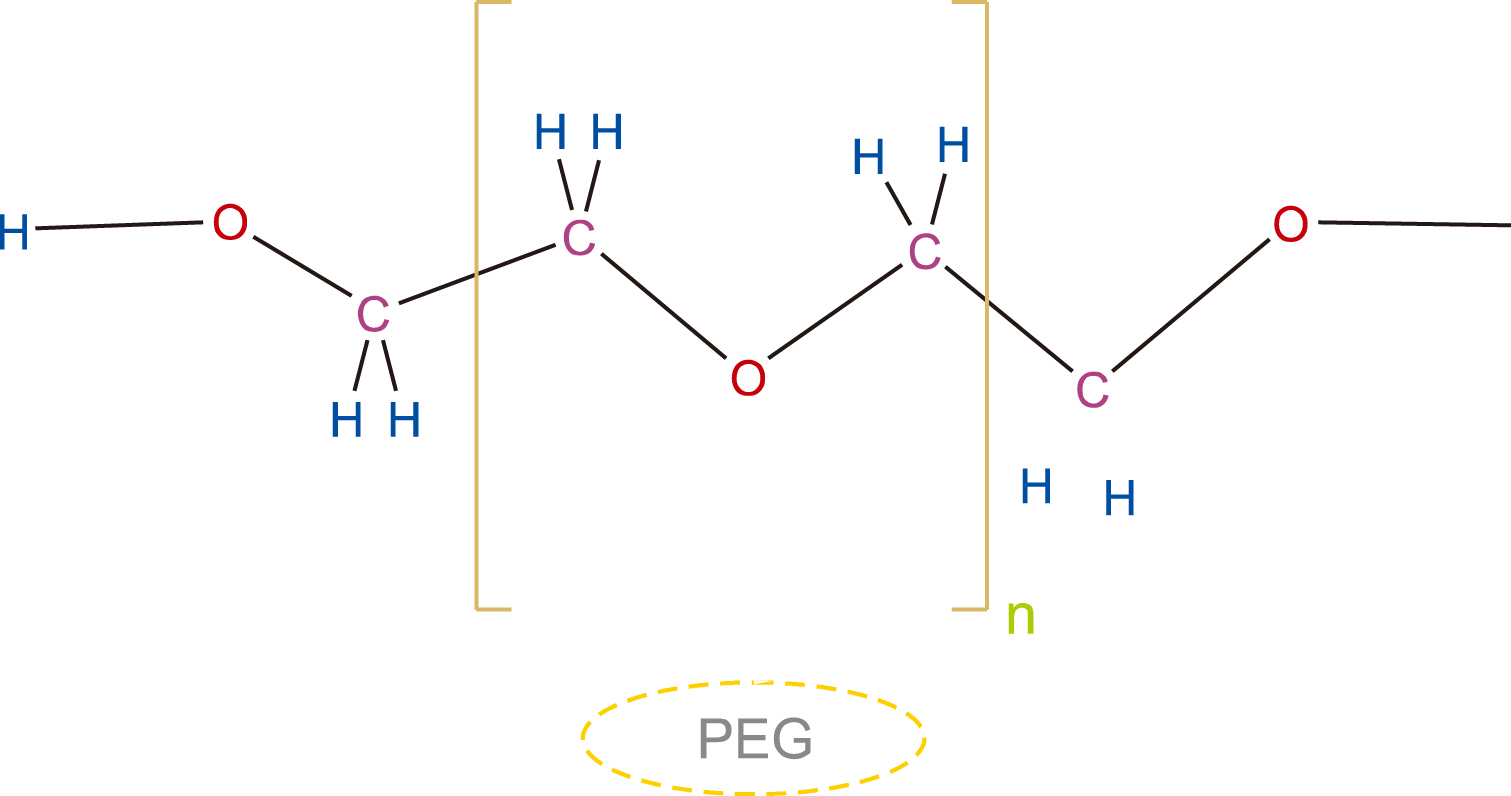
- Maintaining the quality of platelet products and increasing their storage time are priorities for treatment applications. The formation of platelet storage lesions that limit the storage period and preservation temperature, which can prepare a decent environment for bacterial growth, are the most important challenges that researchers are dealing with in platelet preservation. Nanotechnology is an emerging field of science that has introduced novel solutions to resolve these problems. Here, we reviewed the reported effects of polymeric nanoparticles—including chitosan, dendrimers, polyethylene glycol (PEG), and liposome—on platelets in articles from 2010 to 2020. As a result, we concluded that the presence of dendrimer nanoparticles with a smaller size, negative charge, low molecular weight, and low concentration along with PEGylation can increase the stability and survival of platelets during storage. In addition, PEGylation of platelets can also be a promising approach to improve the quality of platelet bags during storage.
Figure
Reference
-
1. Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. 2009; Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 37:2259–72. DOI: 10.1177/0363546509349921. PMID: 19875361.2. Árnason NA, Sigurjónsson OE. 2017; New strategies to understand platelet storage lesion. ISBT Sci Ser. 12:496–500. DOI: 10.1111/voxs.12394.
Article3. Stohlawetz P, Horvath M, Pernerstorfer T, et al. 1999; Effects of nitric oxide on platelet activation during plateletpheresis and in vivo tracking of biotinylated platelets in humans. Transfusion. 39:506–14. DOI: 10.1046/j.1537-2995.1999.39050506.x. PMID: 10336001.
Article4. Shrivastava M. 2009; The platelet storage lesion. Transfus Apher Sci. 41:105–13. DOI: 10.1016/j.transci.2009.07.002. PMID: 19683964.
Article5. Verma A, Agarwal P. 2009; Platelet utilization in the developing world: strategies to optimize platelet transfusion practices. Transfus Apher Sci. 41:145–9. DOI: 10.1016/j.transci.2009.07.005. PMID: 19716339.
Article6. Dobrovolskaia MA, McNeil SE. 2016; Handbook of immunological properties of engineered nanomaterials. Volume 2: haematoco-mpatibility of engineered nanomaterials. Singapore:. World Scientific,. 261–302. DOI: 10.1142/9677-vol2.7. Fröhlich E. 2016; Action of nanoparticles on platelet activation and plasmatic coagulation. Curr Med Chem. 23:408–30. DOI: 10.2174/0929867323666160106151428. PMID: 26063498. PMCID: PMC5403968.
Article8. Cicha I. 2015; Thrombosis: novel nanomedical concepts of diagnosis and treatment. World J Cardiol. 7:434–41. DOI: 10.4330/wjc.v7.i8.434. PMID: 26322182. PMCID: PMC4549776.
Article9. Wang L, You X, Dai C, Tong T, Wu J. 2020; Hemostatic nanote-chnologies for external and internal hemorrhage management. Biomater Sci. 8:4396–412. DOI: 10.1039/D0BM00781A. PMID: 32658944.
Article10. Zielińska A, Carreiró F, Oliveira AM, et al. 2020; Polymeric nanoparticles: production, characterization, toxicology and ecotoxicology. Molecules. 25:3731. DOI: 10.3390/molecules25163731. PMID: 32824172. PMCID: PMC7464532.
Article11. Braddock M. 2016. Nanomedicines: design, delivery and detection. Royal Society of Chemistry;London, UK: DOI: 10.1039/9781782622536.12. Chambers P, McCarthy HO, Dunne NJ. 2019; Emerging areas of bone repair materials: nucleic acid therapy and drug delivery. In: Pawelec KM, Planell JA, eds. Bone repair biomaterials. 2nd ed. Cambridge, UK:. Woodhead Publishing,. 411–46. DOI: 10.1016/B978-0-08-102451-5.00016-0. PMID: 30991987. PMCID: PMC6469206.13. Fortunati E, Luzi F, Yang W, Kenny J, Torre L, Puglia D. 2018; Bio-based nanocomposites in food packaging. In: Cerqueira MAPR, Lagaron JM, Pastrana Castro LM, de Oliveira Soares Vicente AAM, eds. Nanomaterials for food packaging. Philadelphia, PA:. Elsevier Inc,. 71–110. DOI: 10.1016/B978-0-323-51271-8.00004-8.14. Zadeh Mehrizi T, Mosaffa N, Haji Molla Hoseini M, et al. 2018; In vivo therapeutic effects of four synthesized antileishmanial nanodrugs in the treatment of Leishmaniasis. Arch Clin Infect Dis. 13:e80314. DOI: 10.5812/archcid.80314.
Article15. Zadeh Mehrizi T, Pirali Hamedani M, Ebrahimi Shahmabadi H, et al. 2020; Effective materials of medicinal plants for leishmania treatment in vivo environment. J Med Plants. 19:39–62. DOI: 10.29252/jmp.19.74.39.
Article16. Zadeh Mehrizi T, Shafiee Ardestani M, Haji Molla Hoseini M, Khamesipour A, Mosaffa N, Ramezani A. 2018; Novel nanosized chitosan-betulinic acid against resistant leishmania major and first clinical observation of such parasite in kidney. Sci Rep. 8:11759. DOI: 10.1038/s41598-018-30103-7. PMID: 30082741. PMCID: PMC6078985.
Article17. Mehrizi TZ, Ardestani MS, Molla Hoseini MH, Khamesipour A, Mosaffa N, Ramezani A. 2018; Novel nano-sized chitosan amphotericin B formulation with considerable improvement against Leishmania major. Nanomedicine (Lond). 13:3129–47. DOI: 10.2217/nnm-2018-0063. PMID: 30463469.
Article18. Wang YW, Liu CC, Cherng JH, et al. 2019; Biological effects of chitosan-based dressing on hemostasis mechanism. Polymers (Basel). 11:1906. DOI: 10.3390/polym11111906. PMID: 31752424. PMCID: PMC6918334.
Article19. Chan LW, Kim CH, Wang X, Pun SH, White NJ, Kim TH. 2016; PolySTAT-modified chitosan gauzes for improved hemostasis in external hemorrhage. Acta Biomater. 31:178–85. DOI: 10.1016/j.actbio.2015.11.017. PMID: 26593785. PMCID: PMC4728046.
Article20. Hu Z, Zhang DY, Lu ST, Li PW, Li SD. 2018; Chitosan-based composite materials for prospective hemostatic applications. Mar Drugs. 16:273. DOI: 10.3390/md16080273. PMID: 30081571. PMCID: PMC6117657.
Article21. Liu H, Wang C, Li C, et al. 2018; A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing. RSC Adv. 8:7533–49. DOI: 10.1039/C7RA13510F.
Article22. Pourshahrestani S, Zeimaran E, Adib Kadri N, et al. 2016; Gallium-containing mesoporous bioactive glass with potent hemostatic activity and antibacterial efficacy. J Mater Chem B. 4:71–86. DOI: 10.1039/C5TB02062J. PMID: 32262810.
Article23. Shi X, Fang Q, Ding M, et al. 2016; Microspheres of carboxymethyl chitosan, sodium alginate and collagen for a novel hemostatic in vitro study. J Biomater Appl. 30:1092–102. DOI: 10.1177/0885328215618354. PMID: 26611230.
Article24. Gu R, Sun W, Zhou H, et al. 2010; The performance of a fly-larva shell-derived chitosan sponge as an absorbable surgical hemostatic agent. Biomaterials. 31:1270–7. DOI: 10.1016/j.biomaterials.2009.10.023. PMID: 19880175.
Article25. He Q, Gong K, Ao Q, et al. 2013; Positive charge of chitosan retards blood coagulation on chitosan films. J Biomater Appl. 27:1032–45. DOI: 10.1177/0885328211432487. PMID: 22207609.
Article26. Lord MS, Cheng B, McCarthy SJ, Jung M, Whitelock JM. 2011; The modulation of platelet adhesion and activation by chitosan through plasma and extracellular matrix proteins. Biomaterials. 32:6655–62. DOI: 10.1016/j.biomaterials.2011.05.062. PMID: 21676458.
Article27. Chung TW, Lin PY, Wang SS, Chen YF. 2014; Adenosine diphosphate-decorated chitosan nanoparticles shorten blood clotting times, influencing the structures and varying the mechanical properties of the clots. Int J Nanomedicine. 9:1655–64. DOI: 10.2147/IJN.S57855. PMID: 24729701. PMCID: PMC3976209.
Article28. Periayah MH, Halim AS, Hussein AR, Saad AZ, Rashid AH, Noorsal K. 2013; In vitro capacity of different grades of chitosan derivatives to induce platelet adhesion and aggregation. Int J Biol Macromol. 52:244–9. DOI: 10.1016/j.ijbiomac.2012.10.001. PMID: 23063426.
Article29. Jesus S, Marques AP, Duarte A, et al. 2020; Chitosan nanoparticles: shedding light on immunotoxicity and hemocompatibility. Front Bioeng Biotechnol. 8:100. DOI: 10.3389/fbioe.2020.00100. PMID: 32154232. PMCID: PMC7047933.
Article30. Gopalakrishnan L, Ramana LN, Sethuraman S, Krishnan UM. 2014; Ellagic acid encapsulated chitosan nanoparticles as anti-hemorrhagic agent. Carbohydr Polym. 111:215–21. DOI: 10.1016/j.carbpol.2014.03.093. PMID: 25037345.
Article31. Ramtoola Z, Lyons P, Keohane K, Kerrigan SW, Kirby BP, Kelly JG. 2011; Investigation of the interaction of biodegradable micro- and nanoparticulate drug delivery systems with platelets. J Pharm Pharmacol. 63:26–32. DOI: 10.1111/j.2042-7158.2010.01174.x. PMID: 21155812.
Article32. Shelma R, Sharma CP. 2011; Development of lauroyl sulfated chitosan for enhancing hemocompatibility of chitosan. Colloids Surf B Biointerfaces. 84:561–70. DOI: 10.1016/j.colsurfb.2011.02.018. PMID: 21367586.
Article33. Xiong WY, Yi Y, Liu HZ, Wang H, Liu JH, Ying GQ. 2011; Selective carboxypropionylation of chitosan: synthesis, characterization, blood compatibility, and degradation. Carbohydr Res. 346:1217–23. DOI: 10.1016/j.carres.2011.03.037. PMID: 21549358.
Article34. Jiang G, Lin Z, Xu X, Zhang H, Song K. 2012; Stable nanomicelles based on chitosan derivative: in vitro antiplatelet aggregation and adhesion properties. Carbohydrate Polymers. 88:232–8. DOI: 10.1016/j.carbpol.2011.11.089.
Article35. Kim ES, Lee JS, Lee HG. 2016; Nanoencapsulation of red ginseng extracts using chitosan with polyglutamic acid or fucoidan for improving antithrombotic activities. J Agric Food Chem. 64:4765–71. DOI: 10.1021/acs.jafc.6b00911. PMID: 27181678.
Article36. Abbasi E, Aval SF, Akbarzadeh A, et al. 2014; Dendrimers: synthesis, applications, and properties. Nanoscale Res Lett. 9:247. DOI: 10.1186/1556-276X-9-247. PMID: 24994950. PMCID: PMC4074873.
Article37. Roeven E, Scheres L, Smulders MMJ, Zuilhof H. 2019; Design, synthesis, and characterization of fully zwitterionic, functionalized dendrimers. ACS Omega. 4:3000–11. DOI: 10.1021/acsomega.8b03521. PMID: 30847431. PMCID: PMC6398351.
Article38. Zadeh Mehrizi T, Khamesipour A, Shafiee Ardestani M, et al. 2019; Comparative analysis between four model nanoformulations of amphotericin B-chitosan, amphotericin B-dendrimer, betulinic acid-chitosan and betulinic acid-dendrimer for treatment of Leishmania major: real-time PCR assay plus. Int J Nanomedicine. 14:7593–607. DOI: 10.2147/IJN.S220410. PMID: 31802863. PMCID: PMC6831986.39. Dobrovolskaia MA, Patri AK, Potter TM, Rodriguez JC, Hall JB, McNeil SE. 2012; Dendrimer-induced leukocyte procoagulant activity depends on particle size and surface charge. Nanomedicine (Lond). 7:245–56. DOI: 10.2217/nnm.11.105. PMID: 21957862.
Article40. Dobrovolskaia MA, Patri AK, Simak J, et al. 2012; Nanoparticle size and surface charge determine effects of PAMAM dendrimers on human platelets in vitro. Mol Pharm. 9:382–93. DOI: 10.1021/mp200463e. PMID: 22026635. PMCID: PMC3624701.
Article41. Greish K, Thiagarajan G, Herd H, et al. 2012; Size and surface charge significantly influence the toxicity of silica and dendritic nanoparticles. Nanotoxicology. 6:713–23. DOI: 10.3109/17435390.2011.604442. PMID: 21793770.
Article42. Jones CF, Campbell RA, Brooks AE, et al. 2012; Cationic PAMAM dendrimers aggressively initiate blood clot formation. ACS Nano. 6:9900–10. DOI: 10.1021/nn303472r. PMID: 23062017. PMCID: PMC3532938.
Article43. Jones CF, Campbell RA, Franks Z, et al. 2012; Cationic PAMAM dendrimers disrupt key platelet functions. Mol Pharm. 9:1599–611. DOI: 10.1021/mp2006054. PMID: 22497592. PMCID: PMC3367133.
Article44. Chitlur M, Ware E, Kannan S, et al. 2006; Influence of nanopolymers with different end-functionalities on platelet function and the coagulation cascade - an ex-vivo study. Blood (ASH Annual Meeting Abstracts). 108(Suppl):4038. DOI: 10.1182/blood.V108.11.4038.4038.
Article45. Šemberová J. 2012. Nanotechnology in the intensive care: intravascular biocompatibility of carbon nanomaterials-effect of carbon nanotubes on blood platelets [PhD dissertation]. Charles University;Prague, Czech Republic:46. Aisina R, Mukhametova L, Ivanova E. 2020; Influence cationic and anionic PAMAM dendrimers of low generation on selected hemostatic parameters in vitro. Mater Sci Eng C Mater Biol Appl. 109:110605. DOI: 10.1016/j.msec.2019.110605. PMID: 32228918.
Article47. Enciso AE, Neun B, Rodriguez J, Ranjan AP, Dobrovolskaia MA, Simanek EE. 2016; Nanoparticle effects on human platelets in vitro: a comparison between PAMAM and triazine dendrimers. Molecules. 21:428. DOI: 10.3390/molecules21040428. PMID: 27043508. PMCID: PMC6273833.
Article48. Watala C, Karolczak K, Kassassir H, et al. 2016; How do the full-generation poly(amido)amine (PAMAM) dendrimers activate blood platelets? Activation of circulating platelets and formation of "fibrinogen aggregates" in the presence of polycations. Int J Pharm. 503:247–61. DOI: 10.1016/j.ijpharm.2015.08.073. PMID: 26319628.
Article49. Fu Y, Hu R, Li C, Wang Q, Liu Z, Xue W. 2014; Effects of poly (amidoamine) dendrimers on the structure and function of key blood components. J Bioact Compat Polym. 29:165–79. DOI: 10.1177/0883911514521921.50. Liu Y, Pang Y, Toh MR, Chiu GN. 2015; Dual-functionalized poly (amidoamine) dendrimers with poly(ethylene glycol) conjugation and thiolation improved blood compatibility. J Pharm Pharmacol. 67:1492–502. DOI: 10.1111/jphp.12457. PMID: 26303576.51. Alavi SE, Muflih Al Harthi S, Ebrahimi Shahmabadi H, Akbarzadeh A. 2019; Cisplatin-loaded polybutylcyanoacrylate nano-particles with improved properties as an anticancer agent. Int J Mol Sci. 20:1531. DOI: 10.3390/ijms20071531. PMID: 30934689. PMCID: PMC6480951.
Article52. Li P, Zheng W, Ma W, et al. 2018; In-situ preparation of amino-terminated dendrimers on TiO2 films by generational growth for potential and efficient surface functionalization. Appl Surf Sci. 459:438–45. DOI: 10.1016/j.apsusc.2018.08.044.
Article53. Ilinskaya AN, Dobrovolskaia MA. 2013; Nanoparticles and the blood coagulation system. Part I: benefits of nanotechnology. Nanomedicine (Lond). 8:773–84. DOI: 10.2217/nnm.13.48. PMID: 23656264.
Article54. Kim Y, Hechler B, Klutz AM, Gachet C, Jacobson KA. 2008; Toward multivalent signaling across G protein-coupled receptors from poly(amidoamine) dendrimers. Bioconjug Chem. 19:406–11. DOI: 10.1021/bc700327u. PMID: 18176997.
Article55. de Castro S, Maruoka H, Hong K, et al. 2010; Functionalized congeners of P2Y1 receptor antagonists: 2-alkynyl (N)-methanocarba 2'-deoxyadenosine 3',5'-bisphosphate analogues and conjugation to a polyamidoamine (PAMAM) dendrimer carrier. Bioconjug Chem. 21:1190–205. DOI: 10.1021/bc900569u. PMID: 20565071. PMCID: PMC2912410.56. Ziemba B, Halets I, Shcharbin D, et al. 2012; Influence of fourth generation poly(propyleneimine) dendrimers on blood cells. J Biomed Mater Res A. 100:2870–80. DOI: 10.1002/jbm.a.34222. PMID: 22623362.
Article57. Ziemba B, Janaszewska A, Ciepluch K, et al. 2011; In vivo toxicity of poly (propyleneimine) dendrimers. J Biomed Mater Res A. 99:261–8. DOI: 10.1002/jbm.a.33196. PMID: 21976451.58. Franiak-Pietryga I, Ziolkowska E, Ziemba B, et al. 2012; Nanoparticles-a novel approach to chronic lymphocytic leukemia treatment? Blood (ASH Annual Meeting Abstracts). 120(Suppl):4601. DOI: 10.1182/blood.V120.21.4601.4601.59. Franiak-Pietryga I, Ziółkowska E, Ziemba B, et al. 2013; The influence of maltotriose-modified poly(propylene imine) dendrimers on the chronic lymphocytic leukemia cells in vitro: dense shell G4 PPI. Mol Pharm. 10:2490–501. DOI: 10.1021/mp400142p. PMID: 23641871.
Article60. Peña-González CE, Pedziwiatr-Werbicka E, Shcharbin D, et al. 2017; Gold nanoparticles stabilized by cationic carbosilane dendrons: synthesis and biological properties. Dalton Trans. 46:8736–45. DOI: 10.1039/C6DT03791G. PMID: 28091639.
Article61. Pedziwiatr-Werbicka E, Peña-González CE, Stasiak K, et al. 2016. Toxicity of gold nanoparticles stabilized by cationic carbosilane dendrons. Belarusian State University;Minsk, Belarus:62. Dzmitruk V, Pedziwiatr-Werbicka E, Shcharbin D, et al. 2015; Platelets aggregation induced by dendrimers and their complexes with siRNA and ODN, albumins impact on the process. News Biomed Sci. 12:139–43.63. Barrios-Gumiel A, Sánchez-Nieves J, Pedziwiatr-Werbicka E, et al. 2020; Effect of PEGylation on the biological properties of cationic carbosilane dendronized gold nanoparticles. Int J Pharm. 573:118867. DOI: 10.1016/j.ijpharm.2019.118867. PMID: 31765788.
Article64. Hashempour Alamdari N, Alaei-Beirami M, Sadat Shandiz SA, et al. 2017; Gd3+-asparagine-anionic linear globular dendrimer second-generation G2 complexes: novel nanobiohybrid theranostics. Contrast Media Mol Imaging. 2017:3625729. DOI: 10.1155/2017/3625729. PMID: 29097918. PMCID: PMC5635473.65. Mirzaei M, Mohagheghi M, Shahbazi-Gahrouei D, Khatami A. 2012; Novel nanosized GD3+-ALGD-G2-C595: in vivo dual selective MUC-1 positive tumor molecular MR imaging and therapeutic agent. J Nanomed Nanotechnol. 3:1000147. DOI: 10.4172/2157-7439.1000147.66. Mehrizi TZ, Ardestani MS, Khamesipour A, et al. 2018; Reduction toxicity of Amphotericin B through loading into a novel nanoformulation of anionic linear globular dendrimer for improve treatment of leishmania major. J Mater Sci Mater Med. 29:125. DOI: 10.1007/s10856-018-6122-9. PMID: 30056571.
Article67. Mirzaei H, Kazemi B, Bandehpour M, et al. 2016; Computational and nonglycosylated systems: a simpler approach for development of nanosized PEGylated proteins. Drug Des Devel Ther. 10:1193–200. DOI: 10.2147/DDDT.S98323. PMID: 27042012. PMCID: PMC4801162.68. Alavidjeh MS, Haririan I, Khorramizadeh MR, Ghane ZZ, Ardestani MS, Namazi H. 2010; Anionic linear-globular dendrimers: biocompatible hybrid materials with potential uses in nanomedicine. J Mater Sci Mater Med. 21:1121–33. DOI: 10.1007/s10856-009-3978-8. PMID: 20082119.
Article69. Fernandes EG, de Queiroz AA, Abraham GA, San Román J. 2006; Antithrombogenic properties of bioconjugate streptokinase-polyglycerol dendrimers. J Mater Sci Mater Med. 17:105–11. DOI: 10.1007/s10856-006-6813-5. PMID: 16502242.
Article70. D'souza AA, Shegokar R. 2016; Polyethylene glycol (PEG): a versatile polymer for pharmaceutical applications. Expert Opin Drug Deliv. 13:1257–75. DOI: 10.1080/17425247.2016.1182485. PMID: 27116988.71. Knop K, Hoogenboom R, Fischer D, Schubert US. 2010; Poly(ethylene glycol) in drug delivery: pros and cons as well as potential alternatives. Angew Chem Int Ed Engl. 49:6288–308. DOI: 10.1002/anie.200902672. PMID: 20648499.
Article72. Scott MD, Nakane N, Maurer-Spurej E. Quain M, editor. 2019. Cryoprotection of platelets by grafted polymers. Cryopreservation-current advances and evaluations. IntechOpen;London, UK: DOI: 10.5772/intechopen.89272.
Article73. Tarrand J, Andersson B. 2018. Compositions and methods for prolonged cell storage. The University of Texas System;Austin, TX:74. Maurer E, Scott MD, Kitamura N. 2011. Cold storage of pegylated platelets at about or below 0° C. Canadian Blood Services;Ottawa, CA:75. Kerrigan SW, Cox D. 2010; Platelet-bacterial interactions. Cell Mol Life Sci. 67:513–23. DOI: 10.1007/s00018-009-0207-z. PMID: 20091082.
Article76. Greco CA, Maurer-Spurej E, Scott MD, Kalab M, Nakane N, Ramírez-Arcos SM. 2011; PEGylation prevents bacteria-induced platelet activation and biofilm formation in platelet concentrates. Vox Sang. 100:336–9. DOI: 10.1111/j.1423-0410.2010.01419.x. PMID: 21392023.
Article77. Kim Y, Hechler B, Gao ZG, Gachet C, Jacobson KA. 2009; PEGylated dendritic unimolecular micelles as versatile carriers for ligands of G protein-coupled receptors. Bioconjug Chem. 20:1888–98. DOI: 10.1021/bc9001689. PMID: 19785401. PMCID: PMC2891302.
Article78. Fuentes E, Yameen B, Bong SJ, Salvador-Morales C, Palomo I, Vilos C. 2017; Antiplatelet effect of differentially charged PEGylated lipid-polymer nanoparticles. Nanomedicine. 13:1089–94. DOI: 10.1016/j.nano.2016.10.010. PMID: 27789259.
Article79. Srinivasan M, Sudheer AR, Pillai KR, Kumar PR, Sudhakaran PR, Menon VP. 2007; Modulatory effects of curcumin on γ-radiation-induced cellular damage in primary culture of isolated rat hepatocytes. Environ Toxicol Pharmacol. 24:98–105. DOI: 10.1016/j.etap.2007.03.001. PMID: 21783796.
Article80. Wakamoto S, Fujihara M, Abe H, et al. 2001; Effects of poly (ethyleneglycol)-modified hemoglobin vesicles on agonist-induced platelet aggregation and RANTES release in vitro. Artif Cells Blood Substit Immobil Biotechnol. 29:191–201. DOI: 10.1081/BIO-100103043. PMID: 11358035.81. Bakhaidar R, Green J, Alfahad K, et al. 2019; Effect of size and concentration of PLGA-PEG nanoparticles on activation and aggregation of washed human platelets. Pharmaceutics. 11:514. DOI: 10.3390/pharmaceutics11100514. PMID: 31590303. PMCID: PMC6835715.
Article82. Bakhaidar R, O'Neill S, Ramtoola Z. 2020; PLGA-PEG nanoparticles show minimal risks of interference with platelet function of human platelet-rich plasma. Int J Mol Sci. 21:9716. DOI: 10.3390/ijms21249716. PMID: 33352749. PMCID: PMC7767100.
Article83. Akbarzadeh A, Rezaei-Sadabady R, Davaran S, et al. 2013; Liposome: classification, preparation, and applications. Nanoscale Res Lett. 8:102. DOI: 10.1186/1556-276X-8-102. PMID: 23432972. PMCID: PMC3599573.
Article84. Beltrán-Gracia E, López-Camacho A, Higuera-Ciapara I, Velázquez-Fernández JB, Vallejo-Cardona AA. 2019; Nanomedicine review: clinical developments in liposomal applications. Cancer Nano. 10:11. DOI: 10.1186/s12645-019-0055-y.
Article85. Shahabi J, Shahmabadi HE, Alavi SE, et al. 2014; Effect of gold nanoparticles on properties of nanoliposomal hydroxyurea: an in vitro study. Indian J Clin Biochem. 29:315–20. DOI: 10.1007/s12291-013-0355-7. PMID: 24966479. PMCID: PMC4062658.
Article86. Zhang Y, Wei J, Liu S, et al. 2017; Inhibition of platelet function using liposomal nanoparticles blocks tumor metastasis. Theranostics. 7:1062–71. DOI: 10.7150/thno.17908. PMID: 28435448. PMCID: PMC5399576.
Article87. Okamura Y, Katsuno S, Suzuki H, et al. 2010; Release abilities of adenosine diphosphate from phospholipid vesicles with different membrane properties and their hemostatic effects as a platelet substitute. J Control Release. 148:373–9. DOI: 10.1016/j.jconrel.2010.09.013. PMID: 20875473.
Article88. Srinivasan R, Marchant RE, Gupta AS. 2010; In vitro and in vivo platelet targeting by cyclic RGD-modified liposomes. J Biomed Mater Res A. 93:1004–15. DOI: 10.1002/jbm.a.32549. PMID: 19743511. PMCID: PMC2854838.89. Vaidya B, Nayak MK, Dash D, Agrawal GP, Vyas SP. 2011; Development and characterization of site specific target sensitive liposomes for the delivery of thrombolytic agents. Int J Pharm. 403:254–61. DOI: 10.1016/j.ijpharm.2010.10.028. PMID: 20971175.
Article90. Kuznetsova NR, Sevrin C, Lespineux D, et al. 2012; Hemocompatibility of liposomes loaded with lipophilic prodrugs of methotrexate and melphalan in the lipid bilayer. J Control Release. 160:394–400. DOI: 10.1016/j.jconrel.2011.12.010. PMID: 22210161.
Article91. Chan VWT. 2018. Liposomal-encapsulated enzymes can be delivered to and modify platelet function ex vivo [PhD dissertation]. University of British Columbia;Vancouver, Canada:92. Chen KY, Lin TH, Yang CY, Kuo YW, Lei U. 2018; Mechanics for the adhesion and aggregation of red blood cells on chitosan. J Mech. 34:725–32. DOI: 10.1017/jmech.2018.27.
Article93. Stoll C, Holovati JL, Acker JP, Wolkers WF. 2011; Liposomes composed of unsaturated lipids for membrane modification of human erythrocytes. Mol Membr Biol. 28:454–61. DOI: 10.3109/09687688.2011.622304. PMID: 21954868.
Article94. Da Silveira Cavalcante L. 2017. The effects of liposome treatment on red blood cells during hypothermic storage [PhD dissertation]. University of Alberta;Edmonton, Canada:95. da Silveira Cavalcante L, Feng Q, Chin-Yee I, Acker JP, Holovati JL. 2017; Effect of liposome-treated red blood cells in an anemic rat model. J Liposome Res. 27:56–63. DOI: 10.3109/08982104.2016.1149867. PMID: 27055898.96. Stadnick H, Stoll C, Wolkers WF, Acker JP, Holovati JL. 2011; The effect of liposome treatment on the quality of hypothermically stored red blood cells. Biopreserv Biobank. 9:335–42. DOI: 10.1089/bio.2011.0023. PMID: 24836629.
Article97. Stadnick HPA. 2011. The deformability of hypothermically stored red blood cells. University of Alberta;Edmonton, CA:
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- New Frontiers in Molecular Imaging with Superparamagnetic IronOxide Nanoparticles (SPIONs): Efficacy, Toxicity, and FutureApplications
- Multimodal Composite Iron Oxide Nanoparticles for Biomedical Applications
- Immunostimulatory Effects of Silica Nanoparticles in Human Monocytes
- Photo-triggered Theranostic Nanoparticles in Cancer Therapy
- Clinical Application of Gold Nanoparticles for Diagnosis and Treatment