J Korean Neurosurg Soc.
2022 Jan;65(1):130-137. 10.3340/jkns.2021.0056.
Comparative Analysis of COVID-19 Outbreak and Changes in Neurosurgical Emergency Patients
- Affiliations
-
- 1Department of Neurosurgery, Uijeongbu St. Mary's Hospital, School of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2523921
- DOI: http://doi.org/10.3340/jkns.2021.0056
Abstract
Objective
: COVID-19 has spread worldwide since the first case was reported in Wuhan, China, in December 2019. Our institution is a regional trauma and emergency center in the northern Gyeonggi Province. The changing trend of patient care in the emergency room of this hospital likely reflects the overall trend of patients in the area. In the present study, whether changes in the surrounding social environment following the outbreak of COVID-19 changed the incidence of neurosurgical emergency patients and whether differences in practice existed were investigated.
Methods
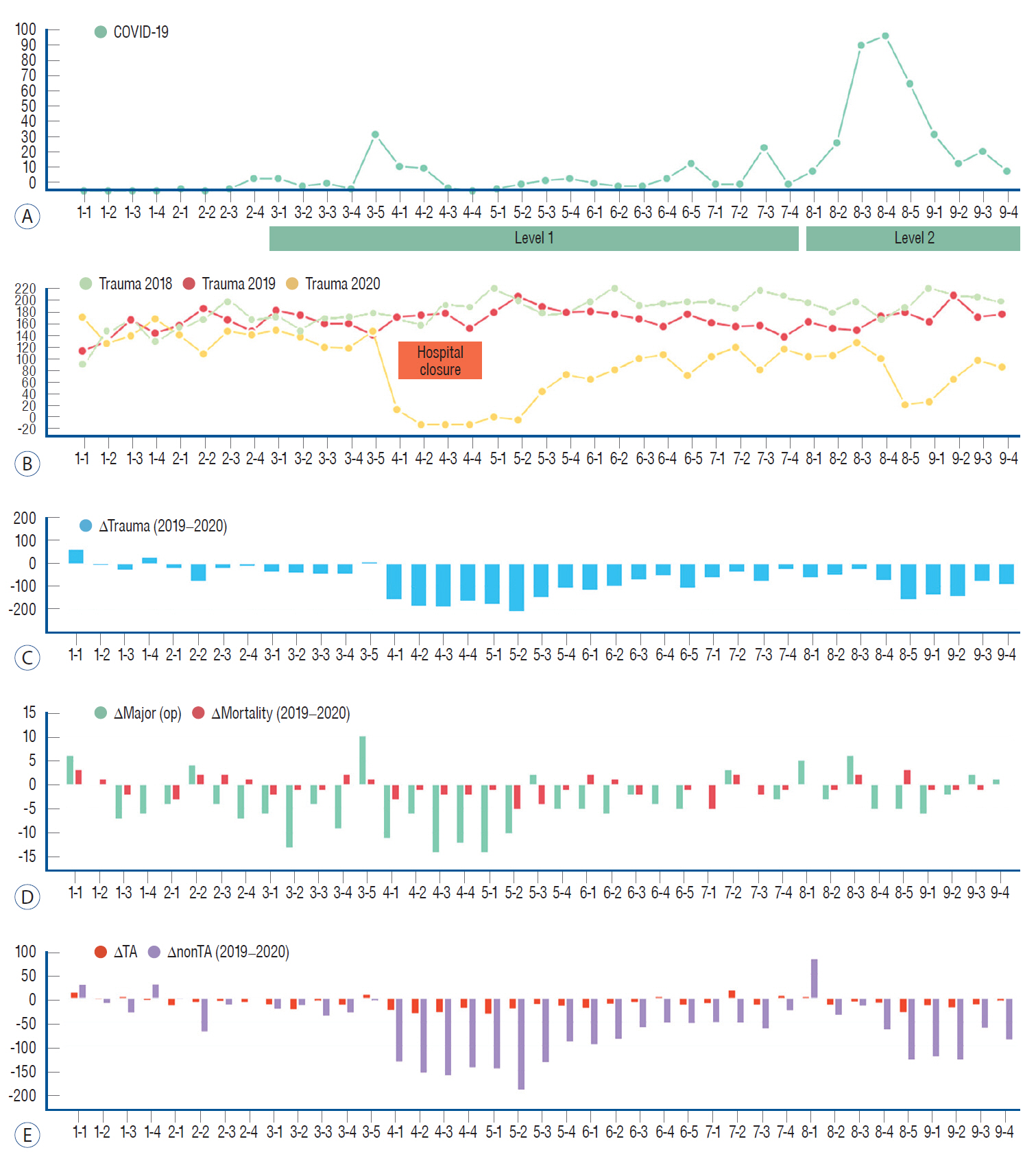
: The overall trend was analyzed from January 2020 which is before the outbreak of COVID-19 to September 2020. To remove bias due to seasonal variation, the previous 2 year's records during the same period were reviewed and compared. Confirmed COVID-19 patients in the northern Gyeonggi Province were identified using data released by the government. And patients who came to the emergency department with head trauma and stroke were identified.
Results
: Based on the present study results, the total number of neurosurgery emergency patients decreased over the study period. In the trauma patient group, the number of patients not involved in traffic accidents significantly decreased compared with patients involved in traffic accidents. Among the stroke cases, the rate of ischemic stroke was lower than hemorrhagic stroke, although a statistically significant difference was not observed. Meanwhile, an increase in the risk of mortality associated with trauma or stroke cases was not observed during the COVID-19 outbreak compared with the same time period in the previous year.
Conclusion
: Due to the occurrence of COVID-19, non-essential activities have decreased and trauma cases not associated with traffic accidents appeared to decrease. Due to the decrease in overall activity, the number of stroke patients has also decreased. This trend is expected to continue even in the post-COVID-19 era, and accordingly, the results from the present study are relevant especially if the current situation continues.
Keyword
Figure
Reference
-
References
1. Capizzi A, Woo J, Verduzco-Gutierrez M. Traumatic brain injury: an overview of epidemiology, pathophysiology, and medical management. Med Clin North Am. 104:213–238. 2020.2. Cui Q, Naikoo NA. Modifiable and non-modifiable risk factors in ischemic stroke: a meta-analysis. Afr Health Sci. 19:2121–2129. 2019.
Article3. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during COVID-19 outbreak in northern Italy. N Engl J Med. 383:88–89. 2020.
Article4. Diegoli H, Magalhães PSC, Martins SCO, Moro CHC, França PHC, Safanelli J, et al. Decrease in hospital admissions for transient ischemic attack, mild, and moderate stroke during the COVID-19 era. Stroke. 51:2315–2321. 2020.
Article5. Ham CH, Moon HJ, Kim JH, Park YK, Lee TH, Kwon WK. Coronavirus disease (COVID-19) outbreak and its impact on spinal daily practice : preliminary report from a single (regional) university hospital in republic of Korea. J Korean Neurosurg Soc. 63:407–414. 2020.
Article6. Hoyer C, Ebert A, Huttner HB, Puetz V, Kallmünzer B, Barlinn K, et al. Acute stroke in times of the COVID-19 pandemic: a multicenter study. Stroke. 51:2224–2227. 2020.7. Kamine TH, Rembisz A, Barron RJ, Baldwin C, Kromer M. Decrease in trauma admissions with COVID-19 pandemic. West J Emerg Med. 21:819–822. 2020.8. Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 35:e112. 2020.9. Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the global burden of disease study 2013. BMJ. 354:i3857. 2016.
Article10. Li Y, Zhou Z, Chen N, He L, Zhou M. Seasonal variation in the occurrence of ischemic stroke: a meta-analysis. Environ Geochem Health. 41:2113–2130. 2019.
Article11. Luostarinen T, Virta J, Satopää J, Bäcklund M, Kivisaari R, Korja M, et al. Intensive care of traumatic brain injury and aneurysmal subarachnoid hemorrhage in Helsinki during the COVID-19 pandemic. Acta Neurochir (Wien). 162:2715–2724. 2020.
Article12. Mathiesen T, Arraez M, Asser T, Balak N, Barazi S, Bernucci C, et al. A snapshot of European neurosurgery December 2019 vs. March 2020: just before and during the COVID-19 pandemic. Acta Neurochir (Wien). 162:2221–2233. 2020.
Article13. Park IN, Yum HK. Stepwise strategy of social distancing in Korea. J Korean Med Sci. 35:e264. 2020.
Article14. Sutherland M, McKenney M, Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 38:1710–1714. 2020.
Article15. Taylor MS, Zelinkova V, Plancikova D, Melichova J, Sivco P, Rusnak M, et al. Seasonal patterns of traumatic brain injury deaths due to trafficrelated incidents in the Slovak Republic. Traffic Inj Prev. 21:55–59. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pre-Hospital Delay in Patients With Acute Stroke During the Initial Phase of the Coronavirus Disease 2019 Outbreak
- Changes in Clinical Characteristics among Febrile Patients Visiting the Emergency Department before and after the COVID-19 Outbreak
- Effect of regional COVID-19 outbreak to emergency department response on acute myocardial infarction: a multicenter retrospective study
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- The impact of COVID-19 through epidemiological changes in out-of-hospital cardiac arrest patients: a study in a single emergency medical center