J Korean Neurosurg Soc.
2022 Jan;65(1):96-106. 10.3340/jkns.2021.0131.
The Effect of Hounsfield Unit Value with Conventional Computed Tomography and Intraoperative Distraction on Postoperative Intervertebral Height Reduction in Patients Following Stand-Alone Anterior Cervical Discectomy and Fusion
- Affiliations
-
- 1Department of Neurosurgery, Pusan National University Yangsan Hospital, Yangsan, Korea
- 2Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 3Department of Neurosurgery, School of Medicine, Pusan National University, Yangsan, Korea
- KMID: 2523917
- DOI: http://doi.org/10.3340/jkns.2021.0131
Abstract
Objective
: The most common complication of anterior cervical discectomy and fusion (ACDF) is cage subsidence and maintenance of disc height affects postoperative clinical outcomes. We considered cage subsidence as an inappropriate indicator for evaluating preservation of disc height. Thus, this study aimed to consider patients with complications such as reduced total disc height compared to that before surgery and evaluate the relevance of several factors before ACDF.
Methods
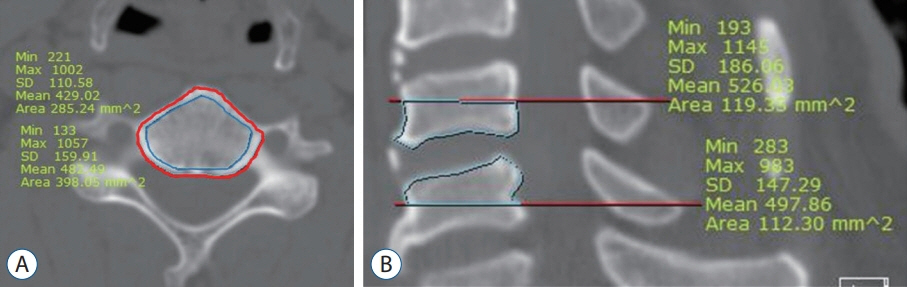
: We retrospectively reviewed the medical records of 40 patients who underwent stand-alone single-level ACDF using a polyetheretherketone (PEEK) cage at our institution between January 2012 and December 2018. Our study population comprised 19 male and 21 female patients aged 24–70 years. The minimum follow-up period was 1 year. Twenty-seven patients had preoperative bone mineral density (BMD) data on dual-energy X-ray absorptiometry. Clinical parameters included sex, age, body mass index, smoking history, and prior medical history. Radiologic parameters included the C2-7 cobb angle, segmental angle, sagittal vertical axis, disc height, and total intervertebral height (TIH) at the preoperative and postoperative periods. Cage decrement was defined as the reduction in TIH at the 6-month follow-up compared to preoperative TIH. To evaluate the bone quality, Hounsfield unit (HU) value was calculated in the axial and sagittal images of conventional computed tomography.
Results
: Lumbar BMD values and cervical HU values were significantly correlated (r=0.733, p<0.001). We divided the patients into two groups based on cage decrement, and 47.5% of the total patients were regarded as cage decrement. There were statistically significant differences in the parameters of measuring the HU value of the vertebra and intraoperative distraction between the two groups. Using these identified factors, we performed a receiver operating characteristic (ROC) curve analysis. Based on the ROC curve, the cut-off point was 530 at the HU value of the upper cortical and cancellous vertebrae (p=0.014; area under the curve [AUC], 0.727; sensitivity, 94.7%; specificity, 42.9%) and 22.41 at intraoperative distraction (p=0.017; AUC, 0.722; sensitivity, 85.7%; specificity, 57.9%). Using this value, we converted these parameters into a bifurcated variable and assessed the multinomial regression analysis to evaluate the risk factors for cage decrement in ACDF. Intraoperative distraction and HU value of the upper vertebral body were independent factors of postoperative subsidence.
Conclusion
: Insufficient intraoperative distraction and low HU value showed a strong relationship with postoperative intervertebral height reduction following single stand-alone PEEK cage ACDF.
Figure
Reference
-
References
1. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 16:1395–1400. 2007.
Article2. Brenke C, Dostal M, Scharf J, Weiß C, Schmieder K, Barth M. Influence of cervical bone mineral density on cage subsidence in patients following stand-alone anterior cervical discectomy and fusion. Eur Spine J. 24:2832–2840. 2015.
Article3. Choi MK, Kim SB, Lee JH. Rare intractable cervicalgia related to exaggerated disc height distraction : report of two cases and literature review. J Korean Neurosurg Soc. 61:530–536. 2018.
Article4. Coe JD, Warden KE, Herzig MA, McAfee PC. Influence of bone mineral density on the fixation of thoracolumbar implants. A comparative study of transpedicular screws, laminar hooks, and spinous process wires. Spine (Phila Pa 1976). 15:902–907. 1990.
Article5. Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. Spine J. 9:537–544. 2009.
Article6. Jergas M, Breitenseher M, Glüer CC, Black D, Lang P, Grampp S, et al. Which vertebrae should be assessed using lateral dual-energy X-ray absorptiometry of the lumbar spine. Osteoporos Int. 5:196–204. 1995.
Article7. Kao TH, Wu CH, Chou YC, Chen HT, Chen WH, Tsou HK. Risk factors for subsidence in anterior cervical fusion with stand-alone polyetheretherketone (PEEK) cages: a review of 82 cases and 182 levels. Arch Orthop Trauma Surg. 134:1343–1351. 2014.
Article8. Kast E, Derakhshani S, Bothmann M, Oberle J. Subsidence after anterior cervical inter-body fusion. A randomized prospective clinical trial. Neurosurg Rev. 32:207–214. discussion 214. 2009.
Article9. Kettler A, Wilke HJ, Claes L. Effects of neck movements on stability and subsidence in cervical interbody fusion: an in vitro study. J Neurosurg. 94(1 Suppl):97–107. 2001.
Article10. Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 7:205–209. 2007.
Article11. Lee SJ, Binkley N, Lubner MG, Bruce RJ, Ziemlewicz TJ, Pickhardt PJ. Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int. 27:1131–1136. 2016.
Article12. Lochmüller EM, Bürklein D, Kuhn V, Glaser C, Müller R, Glüer CC, et al. Mechanical strength of the thoracolumbar spine in the elderly: prediction from in situ dual-energy X-ray absorptiometry, quantitative computed tomography (QCT), upper and lower limb peripheral QCT, and quantitative ultrasound. Bone. 31:77–84. 2002.
Article13. Mi J, Li K, Zhao X, Zhao CQ, Li H, Zhao J. Vertebral body Hounsfield units are associated with cage subsidence after transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Clin Spine Surg. 30:E1130–E1136. 2017.
Article14. Sakai Y, Takenaka S, Matsuo Y, Fujiwara H, Honda H, Makino T, et al. Hounsfield unit of screw trajectory as a predictor of pedicle screw loosening after single level lumbar interbody fusion. J Orthop Sci. 23:734–738. 2018.
Article15. Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. J Bone Joint Surg Am. 93:1057–1063. 2011.
Article16. Singh K, Vaccaro AR, Kim J, Lorenz EP, Lim TH, An HS. Biomechanical comparison of cervical spine reconstructive techniques after a multilevel corpectomy of the cervical spine. Spine (Phila Pa 1976). 28:2352–2358. discussion 2358. 2003.
Article17. Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN. Effects of disc height and distractive forces on graft compression in an anterior cervical discectomy model. Spine (Phila Pa 1976). 27:2441–2445. 2002.
Article18. Wang M, Mummaneni PV, Xi Z, Chang CC, Rivera J, Guinn J, et al. Lower Hounsfield units on CT are associated with cage subsidence after anterior cervical discectomy and fusion. J Neurosurg Spine. 33:425–432. 2020.
Article19. Wu SH, Li Y, Zhang YQ, Li XK, Yuan CF, Hao YL, et al. Porous titanium-6 aluminum-4 vanadium cage has better osseointegration and less micromotion than a poly-ether-ether-ketone cage in sheep vertebral fusion. Artif Organs. 37:E191–E201. 2013.
Article20. Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. 21:1374–1382. 2012.
Article21. Yang JJ, Yu CH, Chang BS, Yeom JS, Lee JH, Lee CK. Subsidence and nonunion after anterior cervical interbody fusion using a stand-alone polyetheretherketone (PEEK) cage. Clin Orthop Surg. 3:16–23. 2011.
Article22. Yoganandan N, Pintar FA, Stemper BD, Baisden JL, Aktay R, Shender BS, et al. Trabecular bone density of male human cervical and lumbar vertebrae. Bone. 39:336–344. 2006.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiological Assessment of the Effects of Anterior Cervical Discectomy and Fusion on Distraction of the Posterior Ligamentum Flavum in Patients with Degenerative Cervical Spines
- Subsidence and Nonunion after Anterior Cervical Interbody Fusion Using a Stand-Alone Polyetheretherketone (PEEK) Cage
- Anterior Cervical Discectomy and Fusion Using a Stand-Alone Polyetheretherketone Cage Packed with Local Autobone : Assessment of Bone Fusion and Subsidence
- Subsidence of Polyetheretherketone Cage after Anterior Cervical Fusion
- Late Results of Anterior Cervical Discectomy and Fusion with Interbody Cages