Ann Surg Treat Res.
2022 Jan;102(1):20-28. 10.4174/astr.2022.102.1.20.
Risk factors deteriorating severe exocrine pancreatic insufficiency measured by stool elastase after pancreatoduodenectomy and the risk factors for weight loss
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2523766
- DOI: http://doi.org/10.4174/astr.2022.102.1.20
Abstract
- Purpose
The measurement of stool elastase (SE) level is useful for evaluating pancreatic exocrine function. This study aimed to determine the risk factors for severe exocrine pancreatic insufficiency (EPI) after pancreatoduodenectomy (PD), and analyze serial changes in nutritional markers and weight based on the SE level.
Methods
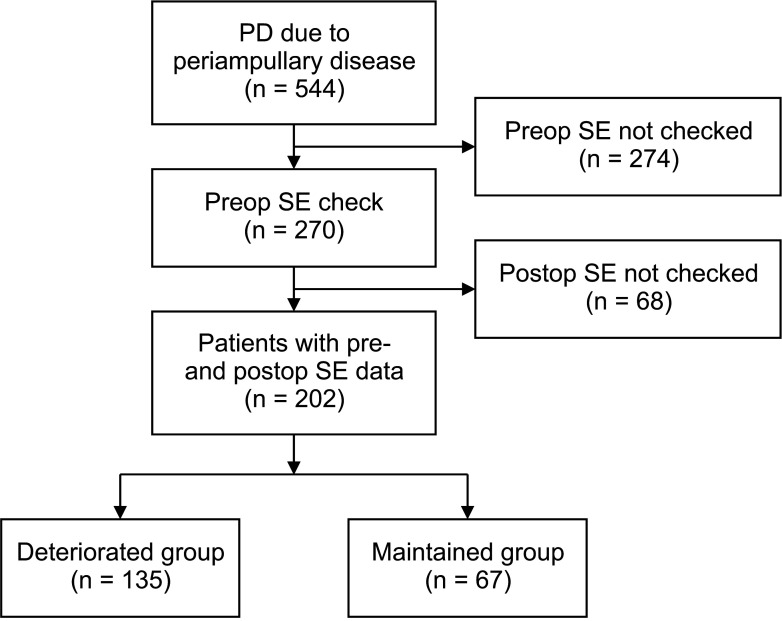
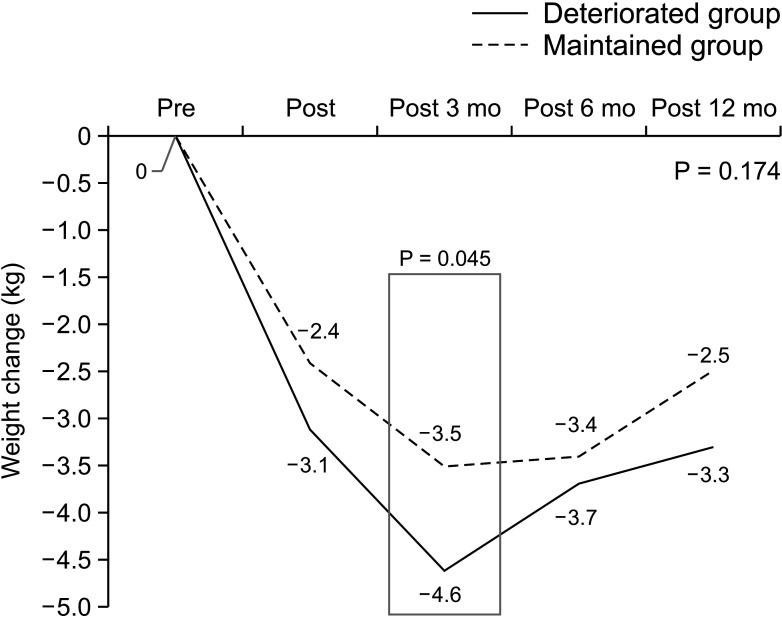
Among patients who underwent PD for periampullary disease, patients whose preoperative and postoperative SE levels were measured were included in the study. The deteriorated (exocrine function) group comprised patients whose SE levels decreased from ≥100 µg/g preoperatively to <100 µg/g postoperatively. Patients whose weight 12 months postoperatively was greater than that 3 months postoperatively were classified into the weight-recovery group.
Results
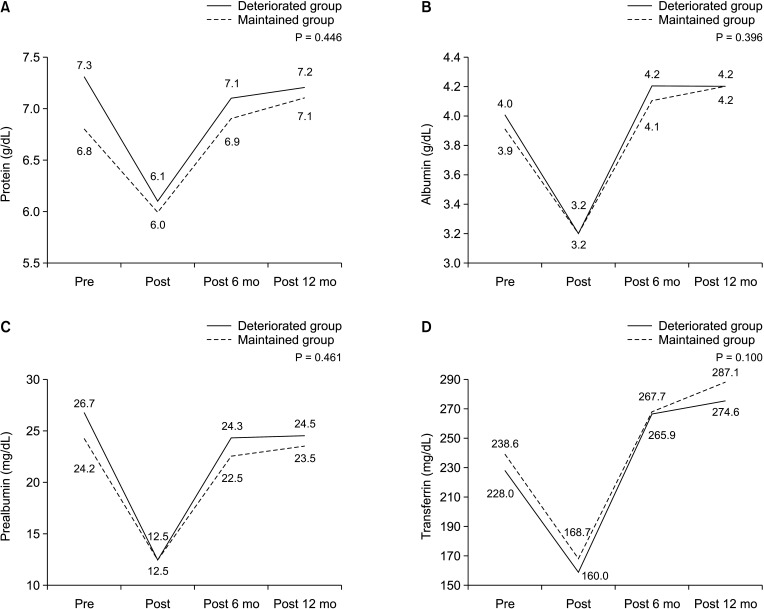
Of the 202 included patients, the deteriorated group had a higher incidence of preoperative SE level above 200 μg/ g, benign pathology, and the presence of a clinically relevant postoperative pancreatic fistula than the maintained group. Patients who did not undergo weight recovery had a higher rate of history of adjuvant radiotherapy compared to the norecovery group.
Conclusion
The evaluation of EPI by measuring SE alone is not sufficient because it does not reflect the nutritional status of patients, and a comprehensive approach that considers other parameters is required for EPI management.
Keyword
Figure
Reference
-
1. Capurso G, Traini M, Piciucchi M, Signoretti M, Arcidiacono PG. Exocrine pancreatic insufficiency: prevalence, diagnosis, and management. Clin Exp Gastroenterol. 2019; 12:129–139. PMID: 30962702.2. Tran TC, van Lanschot JJ, Bruno MJ, van Eijck CH. Functional changes after pancreatoduodenectomy: diagnosis and treatment. Pancreatology. 2009; 9:729–737. PMID: 20090394.
Article3. Hollemans RA, Hallensleben ND, Mager DJ, Kelder JC, Besselink MG, Bruno MJ, et al. Pancreatic exocrine insufficiency following acute pancreatitis: systematic review and study level meta-analysis. Pancreatology. 2018; 18:253–262. PMID: 29482892.
Article4. de la Iglesia-Garcia D, Vallejo-Senra N, Iglesias-Garcia J, López-López A, Nieto L, Domínguez-Muñoz JE. Increased risk of mortality associated with pancreatic exocrine insufficiency in patients with chronic pancreatitis. J Clin Gastroenterol. 2018; 52:e63–e72. PMID: 28858943.
Article5. Löser C, Möllgaard A, Fölsch UR. Faecal elastase 1: a novel, highly sensitive, and specific tubeless pancreatic function test. Gut. 1996; 39:580–586. PMID: 8944569.
Article6. Beharry S, Ellis L, Corey M, Marcon M, Durie P. How useful is fecal pancreatic elastase 1 as a marker of exocrine pancreatic disease? J Pediatr. 2002; 141:84–90. PMID: 12091856.
Article7. Erickson JA, Aldeen WE, Grenache DG, Ashwood ER. Evaluation of a fecal pancreatic elastase-1 enzyme-linked immunosorbent assay: assessment versus an established assay and implication in classifying pancreatic function. Clin Chim Acta. 2008; 397:87–91. PMID: 18706899.
Article8. Goess R, Ceyhan GO, Friess H. Pancreatic exocrine insufficiency after pancreatic surgery. Panminerva Med. 2016; 58:151–159. PMID: 27058237.9. Okano K, Murakami Y, Nakagawa N, Uemura K, Sudo T, Hashimoto Y, et al. Remnant pancreatic parenchymal volume predicts postoperative pancreatic exocrine insufficiency after pancreatectomy. Surgery. 2016; 159:885–892. PMID: 26603844.
Article10. Kim E, Kang JS, Han Y, Kim H, Kwon W, Kim JR, et al. Influence of preoperative nutritional status on clinical outcomes after pancreatoduodenectomy. HPB (Oxford). 2018; 20:1051–1061. PMID: 29887259.
Article11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.12. Lévy P, Barthet M, Mollard BR, Amouretti M, Marion-Audibert AM, Dyard F. Est imat ion of the prevalence and incidence of chronic pancreatitis and its complications. Gastroenterol Clin Biol. 2006; 30:838–844. PMID: 16885867.13. Van de Vijver E, Desager K, Mulberg AE, Staelens S, Verkade HJ, Bodewes FA, et al. Treatment of infants and toddlers with cystic fibrosis-related pancreatic insufficiency and fat malabsorption with pancrelipase MT. J Pediatr Gastroenterol Nutr. 2011; 53:61–64. PMID: 21694537.
Article14. Sziegoleit A, Linder D. Studies on the sterol-binding capacity of human pancreatic elastase 1. Gastroenterology. 1991; 100:768–774. PMID: 1993499.
Article15. Seiler CM, Izbicki J, Varga-Szabó L, Czakó L, Fiók J, Sperti C, et al. Randomised clinical trial: a 1-week, double-blind, placebo-controlled study of pancreatin 25 000 Ph. Eur. minimicrospheres (Creon 25000 MMS) for pancreatic exocrine insufficiency after pancreatic surgery, with a 1-year open-label extension. Aliment Pharmacol Ther. 2013; 37:691–702. PMID: 23383603.16. Park JW, Jang JY, Kim EJ, Kang MJ, Kwon W, Chang YR, et al. Effects of pancreatectomy on nutritional state, pancreatic function and quality of life. Br J Surg. 2013; 100:1064–1070. PMID: 23616030.
Article17. Tran TC, van 't Hof G, Kazemier G, Hop WC, Pek C, van Toorenenbergen AW, et al. Pancreatic fibrosis correlates with exocrine pancreatic insufficiency after pancreatoduodenectomy. Dig Surg. 2008; 25:311–318. PMID: 18818498.
Article18. Tanaka T, Ichiba Y, Fujii Y, Kodama O, Dohi K. Clinical and experimental study of pancreatic exocrine function after pancreaticoduodenectomy for periampullary carcinoma. Surg Gynecol Obstet. 1988; 166:200–205. PMID: 3257831.19. Bruno MJ, Haverkort EB, Tytgat GN, van Leeuwen DJ. Maldigestion associated with exocrine pancreatic insufficiency: implications of gastrointestinal physiology and properties of enzyme preparations for a cause-related and patient-tailored treatment. Am J Gastroenterol. 1995; 90:1383–1393. PMID: 7661155.20. Ito K. Duodenum preservat ion in pancreatic head resection to maintain pancreatic exocrine function (determined by pancreatic function diagnostant test and cholecystokinin secretion). J Hepatobiliary Pancreat Surg. 2005; 12:123–128. PMID: 15868075.21. Bruno MJ. Maldigestion and exocrine pancreatic insufficiency after pancreatic resection for malignant disease: pathophysiology and treatment. Pancreatology. 2001; 1:55–61.22. Nordback I, Parviainen M, Piironen A, Räty S, Sand J. Obstructed pancreaticojejunostomy partly explains exocrine insufficiency after pancreatic head resection. Scand J Gastroenterol. 2007; 42:263–270. PMID: 17327947.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Pancreatic Function after Pylorus Preserving Pancreatoduodenectomy according to the Pancreatoenterostomy
- Clinical Evaluation of the Fecal and Serum Elastase 1 test in the Diagnosis of Chronic Pancreatitis
- Clinical Utility of Fecal Elastase 1 Test in Chronic Pancreatitis
- The Clinical Usefulness of Fecal Elastase-1 Test as an Exocrine Pancreatic Function Test for the Diagnosis of Chronic Pancreatitis
- The diagnostic value of serum and fecal pancreatic elastase-1 in patients with pancreatic disease