Korean J healthc assoc Infect Control Prev.
2021 Dec;26(2):70-82. 10.14192/kjicp.2021.26.2.70.
Current Strategy and Perspective View for Preventing Clostridioides Difficile Infection in Acute Care Facilities
- Affiliations
-
- 1Division of Infectious Diseases, Samsung Changwon Hospital, Sungkyunkwan University, Changwon, Korea
- KMID: 2523604
- DOI: http://doi.org/10.14192/kjicp.2021.26.2.70
Abstract
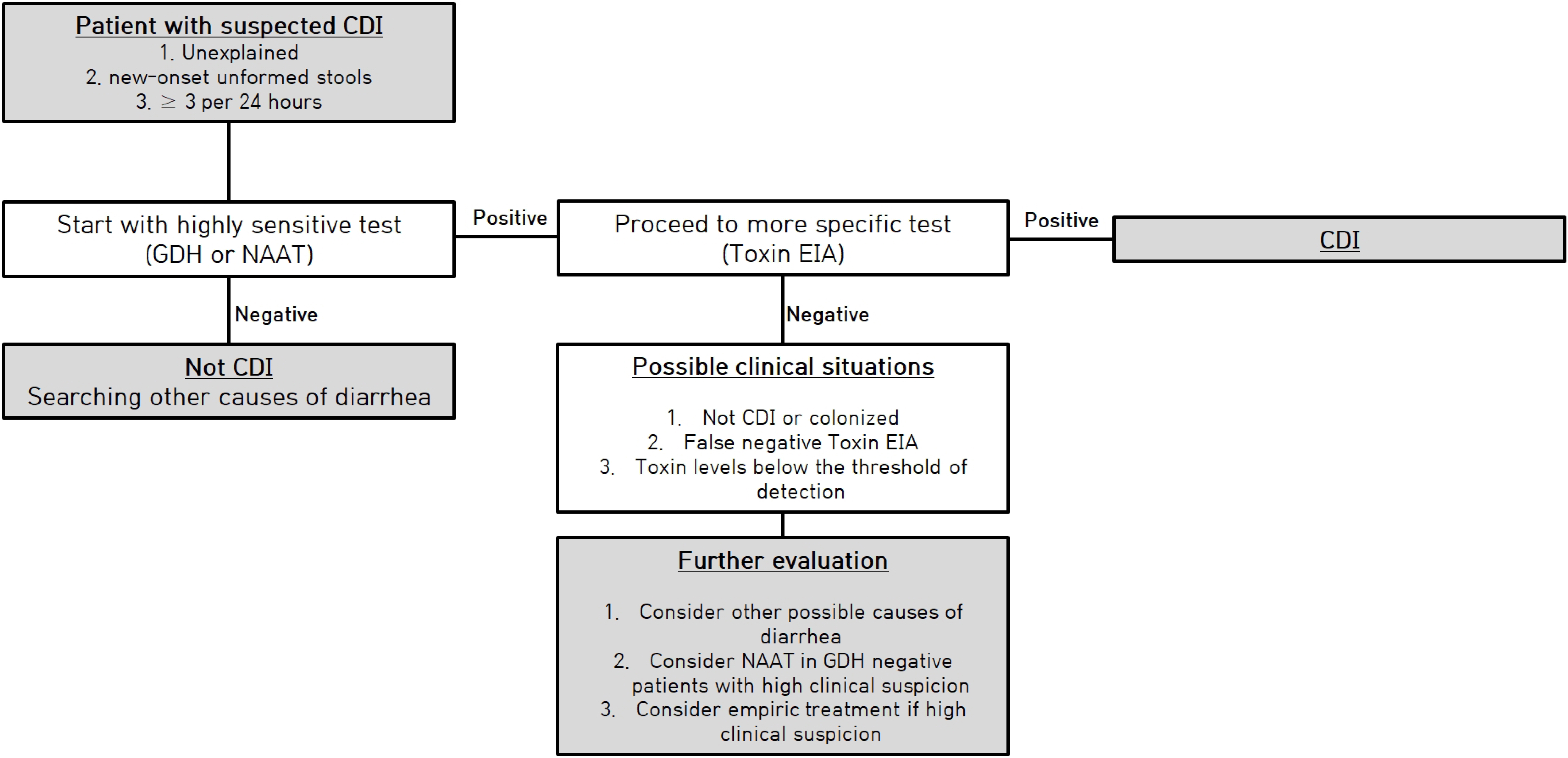
- Clostridium difficile is a spore-forming anaerobic gram-positive bacillus. With increasing antibiotic use, changing patient population, and microbiological characteristics of C. difficile, this pathogen has emerged as one of the most challenging pathogens of nosocomial infections. The current important strategies for preventing C. difficile infection (CDI) are patient monitoring, early recognition (prompt and accurate diagnosis accompanied by an appropriate diagnostic algorithm and a CDI surveillance system), blocking transmission (contact isolation, hand washing, environmental disinfection, and cleaning), and controlling risk factors (increasing the appropriateness of antibiotic use through antibiotic stewardship program). In this review, we will reappraise the clinical efficacy and efficiency of each strategy for preventing CDI and introduce promising interventions for CDI prevention.
Keyword
Figure
Reference
-
1. Hall IC, O’Toole E. 1935; Intestinal flora in new-born infants: with a description of a new pathogenic anaerobe, Bacillus difficilis. Am J Dis Child. 49:390–402.2. Zhu D, Sorg JA, Sun X. 2018; Clostridioides difficile biology: sporulation, germination, and corresponding therapies for C. difficile infection. Front Cell Infect Microbiol. 8:29. DOI: 10.3389/fcimb.2018.00029. PMID: 29473021. PMCID: PMC5809512.
Article3. Leffler DA, Lamont JT. 2015; Clostridium difficile infection. N Engl J Med. 372:1539–48. DOI: 10.1056/NEJMra1403772. PMID: 25875259.
Article4. Kyne L, Warny M, Qamar A, Kelly CP. 2000; Asymptomatic carriage of Clostridium difficile and serum levels of IgG antibody against toxin A. N Engl J Med. 342:390–7. DOI: 10.1056/NEJM200002103420604. PMID: 10666429.5. Seekatz AM, Rao K, Santhosh K, Young VB. 2016; Dynamics of the fecal microbiome in patients with recurrent and nonrecurrent Clostridium difficile infection. Genome Med. 8:47. DOI: 10.1186/s13073-016-0298-8. PMID: 27121861. PMCID: PMC4847246.
Article6. McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. 2018; Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 66:e1–48. DOI: 10.1093/cid/ciy149. PMID: 29562266.
Article7. Marra AR, Perencevich EN, Nelson RE, Samore M, Khader K, Chiang HY, et al. 2020; Incidence and outcomes associated with Clostridium difficile infections: a systematic review and meta-analysis. JAMA Netw Open. 3:e1917597. DOI: 10.1001/jamanetworkopen.2019.17597. PMID: 31913488. PMCID: PMC6991241.8. Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al. 2020; ; Emerging Infections Program Clostridioides difficile Infection Working Group. Trends in U.S. burden of Clostridioides difficile infection and outcomes. N Engl J Med. 382:1320–30.9. Han SH, Kim H, Lee K, Jeong SJ, Park KH, Song JY, et al. 2014; Epidemiology and clinical features of toxigenic culture-confirmed hospital-onset Clostridium difficile infection: a multicentre prospective study in tertiary hospitals of South Korea. J Med Microbiol. 63(Pt 11):1542–51. DOI: 10.1099/jmm.0.070672-0. PMID: 25187603.
Article10. Pai H, Kim YJ, Kim JE, Bae IK, Choi WS, Lee DG. 2014. Dec. Epidemiology of Clostridium infection in Korean hospitals and development of guideline for CDI control in hospital. Korea Centers for Disease Control and Prevention;Cheongju: Report No.: 11-1352159-000270-01.11. Kim J, Kim B, Lee CS, Kim ES, Lee SH, Kim YS, et al. 2021; Active surveillance of Clostridioides difficile infections in 10 tertiary hospitals. Infect Chemother. 53(Suppl 2):264–6.12. Tschudin-Sutter S, Kuijper EJ, Durovic A, Vehreschild MJGT, Barbut F, Eckert C, et al. 2018; Guidance document for prevention of Clostridium difficile infection in acute healthcare settings. Clin Microbiol Infect. 24:1051–4. DOI: 10.1016/j.cmi.2018.02.020. PMID: 29505879.
Article13. Kim KH, Fekety R, Batts DH, Brown D, Cudmore M, Silva J Jr, et al. 1981; Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis. 143:42–50. DOI: 10.1093/infdis/143.1.42. PMID: 7217711.
Article14. Dubberke ER, Reske KA, Noble-Wang J, Thompson A, Killgore G, Mayfield J, et al. 2007; Prevalence of Clostridium difficile environmental contamination and strain variability in multiple health care facilities. Am J Infect Control. 35:315–8. DOI: 10.1016/j.ajic.2006.12.006. PMID: 17577478.
Article15. Lewis SJ, Heaton KW. 1997; Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 32:920–4. DOI: 10.3109/00365529709011203. PMID: 9299672.
Article16. Public Health England. Updated guidance on the management and treatment of Clostridium difficile infection. https://www.gov.uk/government/publications/clostridium-difficile-infection-guidance-on-management-and-treatment . Updated on May 2013.17. Crobach MJ, Planche T, Eckert C, Barbut F, Terveer EM, Dekkers OM, et al. 2016; European Society of Clinical Microbiology and Infectious Diseases: update of the diagnostic guidance document for Clostridium difficile infection. Clin Microbiol Infect. 22 Suppl 4:S63–81. DOI: 10.1016/j.cmi.2016.03.010. PMID: 27460910.
Article18. Kelly CR, Fischer M, Allegretti JR, LaPlante K, Stewart DB, Limketkai BN, et al. 2021; ACG clinical guidelines: prevention, diagnosis, and treatment of Clostridioides difficile infections. Am J Gastroenterol. 116:1124–47. DOI: 10.14309/ajg.0000000000001278. PMID: 34003176.
Article19. Centers for Disease Control. National Healthcare Safety Network (NHSN). https://www.cdc.gov/nhsn/index.html . Updated on 15 October 2021.20. Doll M, Marra AR, Apisarnthanarak A, Al-Maani AS, Abbas S, Rosenthal VD. 2021; Prevention of Clostridioides difficile in hospitals: a position paper of the International Society for Infectious Diseases. Int J Infect Dis. 102:188–95. DOI: 10.1016/j.ijid.2020.10.039. PMID: 33122100.
Article21. National Healthcare Safety Network (NHSN). Patient safety component manual. https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf . Updated on January 2021.22. Muto CA, Blank MK, Marsh JW, Vergis EN, O’Leary MM, Shutt KA, et al. 2007; Control of an outbreak of infection with the hypervirulent Clostridium difficile BI strain in a university hospital using a comprehensive “bundle” approach. Clin Infect Dis. 45:1266–73.
Article23. Grigoras CA, Zervou FN, Zacharioudakis IM, Siettos CI, Mylonakis E. 2016; Isolation of C. difficile carriers alone and as part of a bundle approach for the prevention of Clostridium difficile infection (CDI): a mathematical model based on clinical study data. PLoS One. 11:e0156577. DOI: 10.1371/journal.pone.0156577. PMID: 27258068. PMCID: PMC4892551.
Article24. Louh IK, Greendyke WG, Hermann EA, Davidson KW, Falzon L, Vawdrey DK, et al. 2017; Clostridium difficile infection in acute care hospitals: systematic review and best practices for prevention. Infect Control Hosp Epidemiol. 38:476–82. DOI: 10.1017/ice.2016.324. PMID: 28300019. PMCID: PMC5560033.25. Barker AK, Scaria E, Safdar N, Alagoz O. 2020; Evaluation of the cost-effectiveness of infection control strategies to reduce hospital-onset Clostridioides difficile infection. JAMA Netw Open. 3:e2012522. DOI: 10.1001/jamanetworkopen.2020.12522. PMID: 32789514. PMCID: PMC7426752.
Article26. Barker AK, Scaria E, Alagoz O, Sethi AK, Safdar N. 2020; Reducing C. difficile in children: an agent-based modeling approach to evaluate intervention effectiveness. Infect Control Hosp Epidemiol. 41:522–30. DOI: 10.1017/ice.2020.14. PMID: 32052722. PMCID: PMC7461244.27. Teltsch DY, Hanley J, Loo V, Goldberg P, Gursahaney A, Buckeridge DL. 2011; Infection acquisition following intensive care unit room privatization. Arch Intern Med. 171:32–8. DOI: 10.1001/archinternmed.2010.469. PMID: 21220658.
Article28. Brouqui P. 2016; Should we provide acute care in single or double room occupancy? Clin Microbiol Infect. 22:402.
Article29. Vaisman A, Jula M, Wagner J, Winston LG. 2018; Examining the association between hospital-onset Clostridium difficile infection and multiple-bed room exposure: a case-control study. Infect Control Hosp Epidemiol. 39:1068–73. DOI: 10.1017/ice.2018.163. PMID: 30060776.
Article30. Dubberke ER, Carling P, Carrico R, Donskey CJ, Loo VG, McDonald LC, et al. 2014; Strategies to prevent Clostridium difficile infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 35(Suppl 2):S48–65. DOI: 10.1086/676023. PMID: 24799639.
Article31. Sethi AK, Al-Nassir WN, Nerandzic MM, Bobulsky GS, Donskey CJ. 2010; Persistence of skin contamination and environmental shedding of Clostridium difficile during and after treatment of C. difficile infection. Infect Control Hosp Epidemiol. 31:21–7. DOI: 10.1086/649016. PMID: 19929371.32. Johnson S, Gerding DN, Olson MM, Weiler MD, Hughes RA, Clabots CR, et al. 1990; Prospective, controlled study of vinyl glove use to interrupt Clostridium difficile nosocomial transmission. Am J Med. 88:137–40. DOI: 10.1016/0002-9343(90)90462-m. PMID: 2301439.
Article33. Perry C, Marshall R, Jones E. 2001; Bacterial contamination of uniforms. J Hosp Infect. 48:238–41. DOI: 10.1053/jhin.2001.0962. PMID: 11439013.
Article34. Jabbar U, Leischner J, Kasper D, Gerber R, Sambol SP, Parada JP, et al. 2010; Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol. 31:565–70. DOI: 10.1086/652772. PMID: 20429659.35. Isaacson D, Haller B, Leslie H, Roemer M, Winston L. 2015; Novel handwashes are superior to soap and water in removal of Clostridium difficile spores from the hands. Am J Infect Control. 43:530–2. DOI: 10.1016/j.ajic.2015.02.008. PMID: 25952050.
Article36. Hsu J, Abad C, Dinh M, Safdar N. 2010; Prevention of endemic healthcare-associated Clostridium difficile infection: reviewing the evidence. Am J Gastroenterol. 105:2327–39. quiz 2340. DOI: 10.1038/ajg.2010.254. PMID: 20606676.
Article37. Knight N, Strait T, Anthony N, Lovell R, Norton HJ, Sautter R, et al. 2010; Clostridium difficile colitis: a retrospective study of incidence and severity before and after institution of an alcohol-based hand rub policy. Am J Infect Control. 38:523–8. DOI: 10.1016/j.ajic.2009.12.008. PMID: 20392538.38. Rupp ME, Cavalieri RJ, Lyden E, Kucera J, Martin M, Fitzgerald T, et al. 2012; Effect of hospital-wide chlorhexidine patient bathing on healthcare-associated infections. Infect Control Hosp Epidemiol. 33:1094–100. DOI: 10.1086/668024. PMID: 23041806.
Article39. Kengen R, Thoonen E, Daveson K, Loong B, Rodgers H, Beckingham W, et al. 2018; Chlorhexidine washing in intensive care does not reduce bloodstream infections, blood culture contamination and drug-resistant microorganism acquisition: an interrupted time series analysis. Crit Care Resusc. 20:231–40.40. Noto MJ, Domenico HJ, Byrne DW, Talbot T, Rice TW, Bernard GR, et al. 2015; Chlorhexidine bathing and health care-associated infections: a randomized clinical trial. JAMA. 313:369–78. DOI: 10.1001/jama.2014.18400. PMID: 25602496. PMCID: PMC4383133.41. Jury LA, Guerrero DM, Burant CJ, Cadnum JL, Donskey CJ. 2011; Effectiveness of routine patient bathing to decrease the burden of spores on the skin of patients with Clostridium difficile infection. Infect Control Hosp Epidemiol. 32:181–4. DOI: 10.1086/657911. PMID: 21460475.
Article42. Shaughnessy MK, Micielli RL, DePestel DD, Arndt J, Strachan CL, Welch KB, et al. 2011; Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Infect Control Hosp Epidemiol. 32:201–6. DOI: 10.1086/658669. PMID: 21460503.
Article43. Manian FA, Meyer L, Jenne J. 1996; Clostridium difficile contamination of blood pressure cuffs: a call for a closer look at gloving practices in the era of universal precautions. Infect Control Hosp Epidemiol. 17:180–2. PMID: 8708361.
Article44. Brooks S, Khan A, Stoica D, Griffith J, Friedeman L, Mukherji R, et al. 1998; Reduction in vancomycin-resistant Enterococcus and Clostridium difficile infections following change to tympanic thermometers. Infect Control Hosp Epidemiol. 19:333–6. DOI: 10.1086/647824. PMID: 9613694.
Article45. Ofstead CL, Hopkins KM, Buro BL, Eiland JE, Wetzler HP. 2020; Challenges in achieving effective high-level disinfection in endoscope reprocessing. Am J Infect Control. 48:309–15. DOI: 10.1016/j.ajic.2019.09.013. PMID: 31677925.
Article46. McMullen KM, Zack J, Coopersmith CM, Kollef M, Dubberke E, Warren DK. 2007; Use of hypochlorite solution to decrease rates of Clostridium difficile-associated diarrhea. Infect Control Hosp Epidemiol. 28:205–7. DOI: 10.1086/511791. PMID: 17265404.
Article47. Ray AJ, Deshpande A, Fertelli D, Sitzlar BM, Thota P, et al. Sankar C T. 2017; A multicenter randomized trial to determine the effect of an environmental disinfection intervention on the incidence of healthcare-associated Clostridium difficile infection. Infect Control Hosp Epidemiol. 38:777–83. DOI: 10.1017/ice.2017.76. PMID: 28462761.
Article48. Vianna PG, Dale CR Jr, Simmons S, Stibich M, Licitra CM. 2016; Impact of pulsed xenon ultraviolet light on hospital-acquired infection rates in a community hospital. Am J Infect Control. 44:299–303. DOI: 10.1016/j.ajic.2015.10.009. PMID: 26684369.
Article49. Pegues DA, Han J, Gilmar C, McDonnell B, Gaynes S. 2017; Impact of ultraviolet germicidal irradiation for no-touch terminal room disinfection on Clostridium difficile infection incidence among hematology-oncology patients. Infect Control Hosp Epidemiol. 38:39–44. DOI: 10.1017/ice.2016.222. PMID: 27707423.
Article50. Marra AR, Schweizer ML, Edmond MB. 2018; No-touch disinfection methods to decrease multidrug-resistant organism infections: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 39:20–31. DOI: 10.1017/ice.2017.226. PMID: 29144223.
Article51. Barbut F. 2015; How to eradicate Clostridium difficile from the environment. J Hosp Infect. 89:287–95. DOI: 10.1016/j.jhin.2014.12.007. PMID: 25638358.
Article52. Lindsay PJ, Rohailla S, Taggart LR, Lightfoot D, Havey T, Daneman N, et al. 2019; Antimicrobial stewardship and intensive care unit mortality: a systematic review. Clin Infect Dis. 68:748–56. DOI: 10.1093/cid/ciy550. PMID: 29982376.
Article53. Kaki R, Elligsen M, Walker S, Simor A, Palmay L, Daneman N. 2011; Impact of antimicrobial stewardship in critical care: a systematic review. J Antimicrob Chemother. 66:1223–30. DOI: 10.1093/jac/dkr137. PMID: 21460369.
Article54. Feazel LM, Malhotra A, Perencevich EN, Kaboli P, Diekema DJ, Schweizer ML. 2014; Effect of antibiotic stewardship programmes on Clostridium difficile incidence: a systematic review and meta-analysis. J Antimicrob Chemother. 69:1748–54. DOI: 10.1093/jac/dku046. PMID: 24633207.
Article55. Kim SH, Yoon JG, Park HJ, Won H, Ryoo SS, Choi E, et al. 2021; Effects of a comprehensive antimicrobial stewardship program in a surgical intensive care unit. Int J Infect Dis. 108:237–43. DOI: 10.1016/j.ijid.2021.02.082. PMID: 33639294.
Article56. Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E. 2011; Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis. 53:42–8. DOI: 10.1093/cid/cir301. PMID: 21653301.
Article57. Brown KA, Fisman DN, Moineddin R, Daneman N. 2014; The magnitude and duration of Clostridium difficile infection risk associated with antibiotic therapy: a hospital cohort study. PLoS One. 9:e105454. DOI: 10.1371/journal.pone.0105454. PMID: 25157757. PMCID: PMC4144891.
Article58. Lawes T, Lopez-Lozano JM, Nebot CA, Macartney G, Subbarao-Sharma R, Wares KD, et al. 2017; Effect of a national 4C antibiotic stewardship intervention on the clinical and molecular epidemiology of Clostridium difficile infections in a region of Scotland: a non-linear time-series analysis. Lancet Infect Dis. 17:194–206. DOI: 10.1016/S1473-3099(16)30397-8. PMID: 27825595.59. Yun JH, Park GE, Ki HK. 2021; Correlation between antibiotic consumption and the incidence of healthcare facility-onset Clostridioides difficile infection: a retrospective chart review and analysis. Antimicrob Resist Infect Control. 10:117. DOI: 10.1186/s13756-021-00986-9. PMID: 34362442. PMCID: PMC8348999.
Article60. Riggs MM, Sethi AK, Zabarsky TF, Eckstein EC, Jump RL, Donskey CJ. 2007; Asymptomatic carriers are a potential source for transmission of epidemic and nonepidemic Clostridium difficile strains among long-term care facility residents. Clin Infect Dis. 45:992–8. DOI: 10.1086/521854. PMID: 17879913.
Article61. Guerrero DM, Becker JC, Eckstein EC, Kundrapu S, Deshpande A, Sethi AK, et al. 2013; Asymptomatic carriage of toxigenic Clostridium difficile by hospitalized patients. J Hosp Infect. 85:155–8. DOI: 10.1016/j.jhin.2013.07.002. PMID: 23954113.
Article62. Blixt T, Gradel KO, Homann C, Seidelin JB, Schønning K, Lester A, et al. 2017; Asymptomatic carriers contribute to nosocomial Clostridium difficile infection: a cohort study of 4508 patients. Gastroenterology. 152:1031–41.e2. DOI: 10.1053/j.gastro.2016.12.035. PMID: 28063955.
Article63. Lanzas C, Dubberke ER. 2014; Effectiveness of screening hospital admissions to detect asymptomatic carriers of Clostridium difficile: a modeling evaluation. Infect Control Hosp Epidemiol. 35:1043–50. DOI: 10.1086/677162. PMID: 25026622.
Article64. Longtin Y, Paquet-Bolduc B, Gilca R, Garenc C, Fortin E, Longtin J, et al. 2016; Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C difficile infections: a quasi-experimental controlled study. JAMA Intern Med. 176:796–804. DOI: 10.1001/jamainternmed.2016.0177. PMID: 27111806.65. Kwok CS, Arthur AK, Anibueze CI, Singh S, Cavallazzi R, Loke YK. 2012; Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol. 107:1011–9. DOI: 10.1038/ajg.2012.108. PMID: 22525304.
Article66. Gao XW, Mubasher M, Fang CY, Reifer C, Miller LE. 2010; Dose-response efficacy of a proprietary probiotic formula of Lactobacillus acidophilus CL1285 and Lactobacillus casei LBC80R for antibiotic-associated diarrhea and Clostridium difficile-associated diarrhea prophylaxis in adult patients. Am J Gastroenterol. 105:1636–41. DOI: 10.1038/ajg.2010.11. PMID: 20145608.67. Kotowska M, Albrecht P, Szajewska H. 2005; Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea in children: a randomized double-blind placebo-controlled trial. Aliment Pharmacol Ther. 21:583–90. DOI: 10.1111/j.1365-2036.2005.02356.x. PMID: 15740542.
Article68. Su GL, Ko CW, Bercik P, Falck-Ytter Y, Sultan S, Weizman AV, et al. 2020; AGA clinical practice guidelines on the role of probiotics in the management of gastrointestinal disorders. Gastroenterology. 159:697–705. DOI: 10.1053/j.gastro.2020.05.059. PMID: 32531291.
Article69. Popovich KJ, Snitkin ES. 2017; Whole genome sequencing-implications for infection prevention and outbreak investigations. Curr Infect Dis Rep. 19:15. DOI: 10.1007/s11908-017-0570-0. PMID: 28281083.
Article70. Janezic S, Rupnik M. 2019; Development and implementation of whole genome sequencing-based typing schemes for Clostridioides difficile . Front Public Health. 7:309. DOI: 10.3389/fpubh.2019.00309. PMID: 31709221. PMCID: PMC6821651.
Article71. Kuenzli AB, Burri S, Casanova C, Sommerstein R, Buetti N, Seth-Smith HMB, et al. 2020; Successful management of a Clostridioides difficile ribotype 027 outbreak with a lean intervention bundle. J Hosp Infect. 106:240–5. DOI: 10.1016/j.jhin.2020.07.034. PMID: 32745592.
Article72. Luz CF, Vollmer M, Decruyenaere J, Nijsten MW, Glasner C, Sinha B. 2020; Machine learning in infection management using routine electronic health records: tools, techniques, and reporting of future technologies. Clin Microbiol Infect. 26:1291–9. DOI: 10.1016/j.cmi.2020.02.003. PMID: 32061798.
Article73. Oh J, Makar M, Fusco C, McCaffrey R, Rao K, Ryan EE, et al. 2018; A generalizable, data-driven approach to predict daily risk of Clostridium difficile infection at two large academic health centers. Infect Control Hosp Epidemiol. 39:425–33. DOI: 10.1017/ice.2018.16. PMID: 29576042. PMCID: PMC6421072.74. Johnson S, Lavergne V, Skinner AM, Gonzales-Luna AJ, Garey KW, Kelly CP, et al. 2021; Clinical practice guideline by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA): 2021 focused update guidelines on management of Clostridioides difficile infection in adults. Clin Infect Dis. 73:e1029–44. DOI: 10.1093/cid/ciab549. PMID: 34164674.
Article75. Louie TJ, Cannon K, Byrne B, Emery J, Ward L, Eyben M, et al. 2012; Fidaxomicin preserves the intestinal microbiome during and after treatment of Clostridium difficile infection (CDI) and reduces both toxin reexpression and recurrence of CDI. Clin Infect Dis. 55(Suppl 2):S132–42. DOI: 10.1093/cid/cis338. PMID: 22752862. PMCID: PMC3388020.
Article76. Hengel RL, Ritter TE, Nathan RV, Van Anglen LJ, Schroeder CP, Dillon RJ, et al. 2020; Real-world experience of bezlotoxumab for prevention of Clostridioides difficile infection: a retrospective multicenter cohort study. Open Forum Infect Dis. 7:ofaa097. DOI: 10.1093/ofid/ofaa097. PMID: 32363211. PMCID: PMC7186524.
Article77. Korea Centers for Disease Control. 2017. Guidelines for prevention and control of healthcare associated infections. Korea Centers for Disease Control and Prevention;Cheongju: p. 183–210.78. Korea Disease Control. https://kdca.go.kr/contents.es?mid=a20301080100 . Updated on 2 June 2021.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Which is the Preferred Regimen for Non-Severe Clostridioides difficile Infection in Korea, Vancomycin or Metronidazole?
- The Trend of Clostridioides difficile Infection in Korean Hospitals with the Analysis of Nationwide Sample Cohort
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- Case of Pseudomembranous Colitis Caused by a Clostridioides difficile Infection Concomitant with Cytomegalovirus colitis Mimicking Ischemic Colitis
- Association between Antibiotic Consumption and Incidence of Clostridioides difficile Infection in a Hospital