J Korean Med Sci.
2020 Dec;35(47):e407. 10.3346/jkms.2020.35.e407.
Association between Antibiotic Consumption and Incidence of Clostridioides difficile Infection in a Hospital
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2509446
- DOI: http://doi.org/10.3346/jkms.2020.35.e407
Abstract
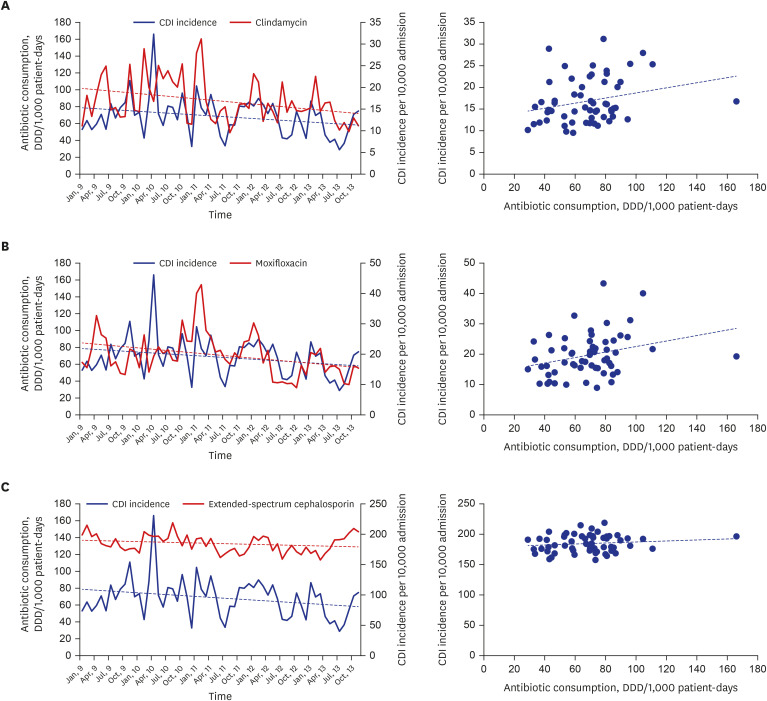
- Previous exposure to antimicrobials is a major risk factor for Clostridioides difficile infection (CDI). Antibiotic prescription and C. difficile toxin assay records of patients admitted to a tertiary hospital in Korea from 2009 to 2013 were collected to investigate the association between antibiotic consumption and CDI incidence. A Spearman's correlation analysis between CDI incidence (positive result of toxin assay/10,000 admissions) and antibiotic consumption (defined daily dose/1,000 patient-days) was performed on a monthly basis. Using the matched month approach, we found a significant correlation between CDI rate and moxifloxacin consumption (Spearman's r = 0.351, P < 0.001). Furthermore, using the onemonth delay approach, we found that the consumption of clindamycin (Spearman's r = 0.272, P = 0.037) and moxifloxacin (Spearman's r = 0.297, P = 0.022) was significantly correlated with CDI incidence. Extended-spectrum cephalosporins did not have any effect on CDI incidence.
Keyword
Figure
Reference
-
1. Freeman J, Bauer MP, Baines SD, Corver J, Fawley WN, Goorhuis B, et al. The changing epidemiology of Clostridium difficile infections. Clin Microbiol Rev. 2010; 23(3):529–549. PMID: 20610822.
Article2. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States. Updated 2020. Accessed May 23, 2020. https://www.multivu.com/players/English/8627551-cdc-antibiotic-resistance-threat-report-2019.3. Brown K, Valenta K, Fisman D, Simor A, Daneman N. Hospital ward antibiotic prescribing and the risks of Clostridium difficile infection. JAMA Intern Med. 2015; 175(4):626–633. PMID: 25705994.4. Leffler DA, Lamont JT, Lamont JT. Clostridium difficile infection. N Engl J Med. 2015; 372(16):1539–1548. PMID: 25875259.
Article5. McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis. 2018; 66(7):e1–e48. PMID: 29462280.
Article6. Owens RC Jr, Donskey CJ, Gaynes RP, Loo VG, Muto CA. Antimicrobial-associated risk factors for Clostridium difficile infection. Clin Infect Dis. 2008; 46(s1):Suppl 1. S19–S31. PMID: 18177218.7. Hensgens MP, Goorhuis A, Dekkers OM, Kuijper EJ. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012; 67(3):742–748. PMID: 22146873.
Article8. Kim J, Kang JO, Kim H, Seo MR, Choi TY, Pai H, et al. Epidemiology of Clostridium difficile infections in a tertiary-care hospital in Korea. Clin Microbiol Infect. 2013; 19(6):521–527. PMID: 22712697.
Article9. McDonald LC, Coignard B, Dubberke E, Song X, Horan T, Kutty PK, et al. Recommendations for surveillance of Clostridium difficile-associated disease. Infect Control Hosp Epidemiol. 2007; 28(2):140–145. PMID: 17265394.
Article10. World Health Organization. Definition and general considerations of defined daily dose (DDD). Updated 2020. Accessed April 7, 2020. http://www.whocc.no/ddd/definition_and_general_considera/.11. Kazakova SV, Baggs J, McDonald LC, Yi SH, Hatfield KM, Guh A, et al. Association between antibiotic use and hospital-onset Clostridioides difficile infection in US acute care hospitals, 2006–2012: an ecologic analysis. Clin Infect Dis. 2020; 70(1):11–18. PMID: 30820545.
Article12. Pereira JB, Farragher TM, Tully MP, Jonathan Cooke J. Association between Clostridium difficile infection and antimicrobial usage in a large group of English hospitals. Br J Clin Pharmacol. 2014; 77(5):896–903. PMID: 24868578.13. Johnson S, Samore MH, Farrow KA, Killgore GE, Tenover FC, Lyras D, et al. Epidemics of diarrhea caused by a clindamycin-resistant strain of Clostridium difficile in four hospitals. N Engl J Med. 1999; 341(22):1645–1651. PMID: 10572152.14. Pépin J, Saheb N, Coulombe MA, Alary ME, Corriveau MP, Authier S, et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis. 2005; 41(9):1254–1260. PMID: 16206099.15. Pear SM, Williamson TH, Bettin KM, Gerding DN, Galgiani JN. Decrease in nosocomial Clostridium difficile-associated diarrhea by restricting clindamycin use. Ann Intern Med. 1994; 120(4):272–277. PMID: 8080497.
Article16. Dingle KE, Didelot X, Quan TP, Eyre DW, Stoesser N, Golubchik T, et al. Effects of control interventions on Clostridium difficile infection in England: an observational study. Lancet Infect Dis. 2017; 17(4):411–421. PMID: 28130063.17. Aldeyab MA, Devine MJ, Flanagan P, Mannion M, Craig A, Scott MG, et al. Multihospital outbreak of Clostridium difficile ribotype 027 infection: epidemiology and analysis of control measures. Infect Control Hosp Epidemiol. 2011; 32(3):210–219. PMID: 21460505.18. Kim B, Lee MJ, Moon SM, Park SY, Song KH, Lee H, et al. Current status of antimicrobial stewardship programmes in Korean hospitals: results of a 2018 nationwide survey. J Hosp Infect. 2020; 104(2):172–180. PMID: 31513880.
Article19. Sinnott SJ, Polinski JM, Byrne S, Gagne JJ. Measuring drug exposure: concordance between defined daily dose and days' supply depended on drug class. J Clin Epidemiol. 2016; 69:107–113. PMID: 26146090.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Which is the Preferred Regimen for Non-Severe Clostridioides difficile Infection in Korea, Vancomycin or Metronidazole?
- Current Strategy and Perspective View for Preventing Clostridioides Difficile Infection in Acute Care Facilities
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- Incidence and Characteristics of Clostridioides difficile Infection in Children
- Diagnostic Stewardship on the Extra-Analytical Phase to Secure Quality Assurance of Diagnostic Tests for Clostridioides difficile Infection