Ann Clin Microbiol.
2020 Dec;23(4):241-249. 10.5145/ACM.2020.23.4.3.
The Trend of Clostridioides difficile Infection in Korean Hospitals with the Analysis of Nationwide Sample Cohort
- Affiliations
-
- 1Department of Research and Analysis, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 2Department of Biostatistics and Computing, Yonsei University Graduate School, Seoul, Korea
- 3Department of Laboratory Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2509647
- DOI: http://doi.org/10.5145/ACM.2020.23.4.3
Abstract
- Background
Clostridioides (Clostridium) difficile is an important pathogen that causes diarrhea in people who take antibiotics. The recent status of C. difficile infection is not wellknown in Korea.
Methods
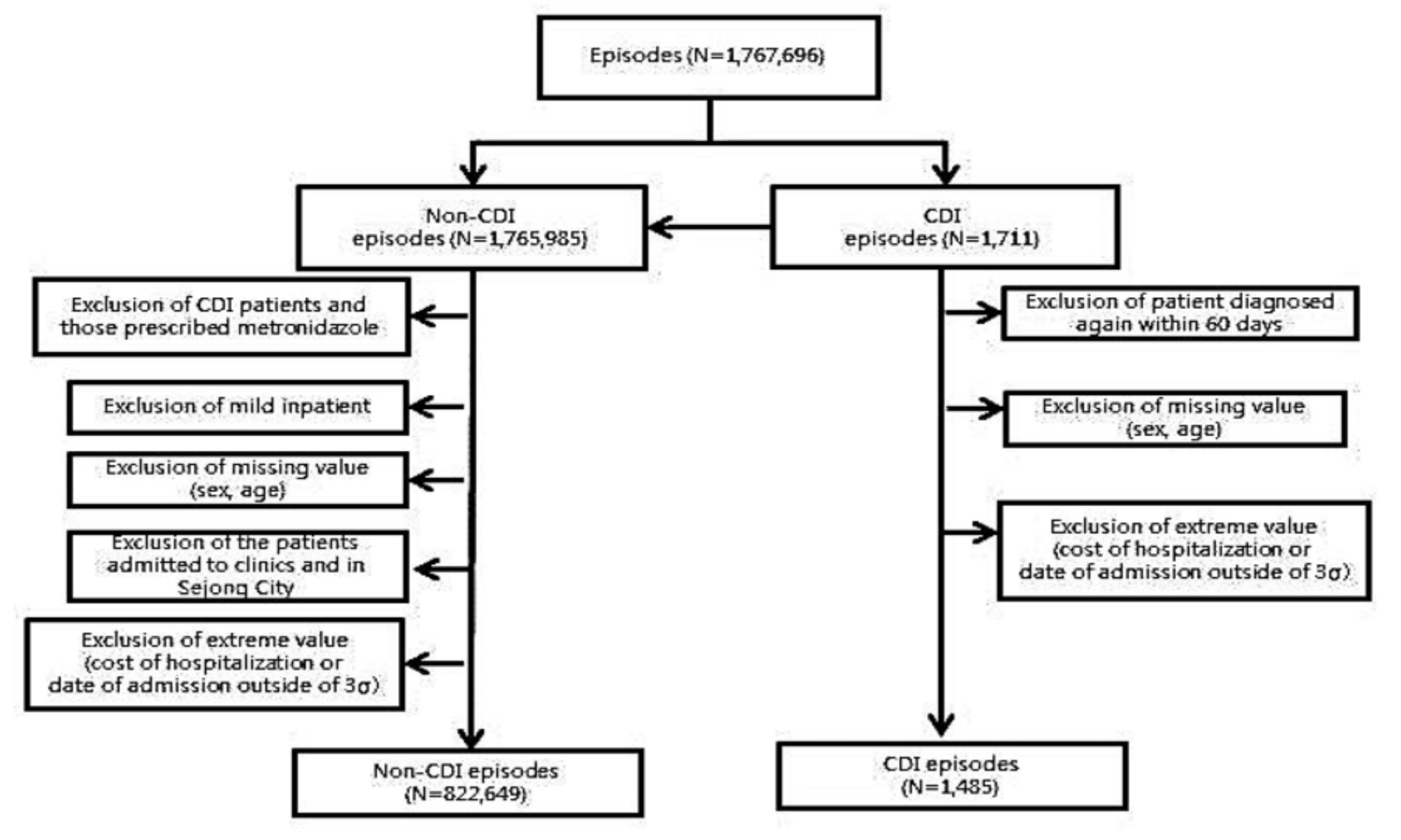
The long-term trend of C. difficile infection in Korean hospitals was analyzed using a nationwide sample cohort. The data also included sociodemographic characteristics, disease severity, and healthcare facilities. C. difficile infection was defined by the prescription of oral vancomycin or all metronidazole prescriptions under C. difficile infectious disease code (A047).
Results
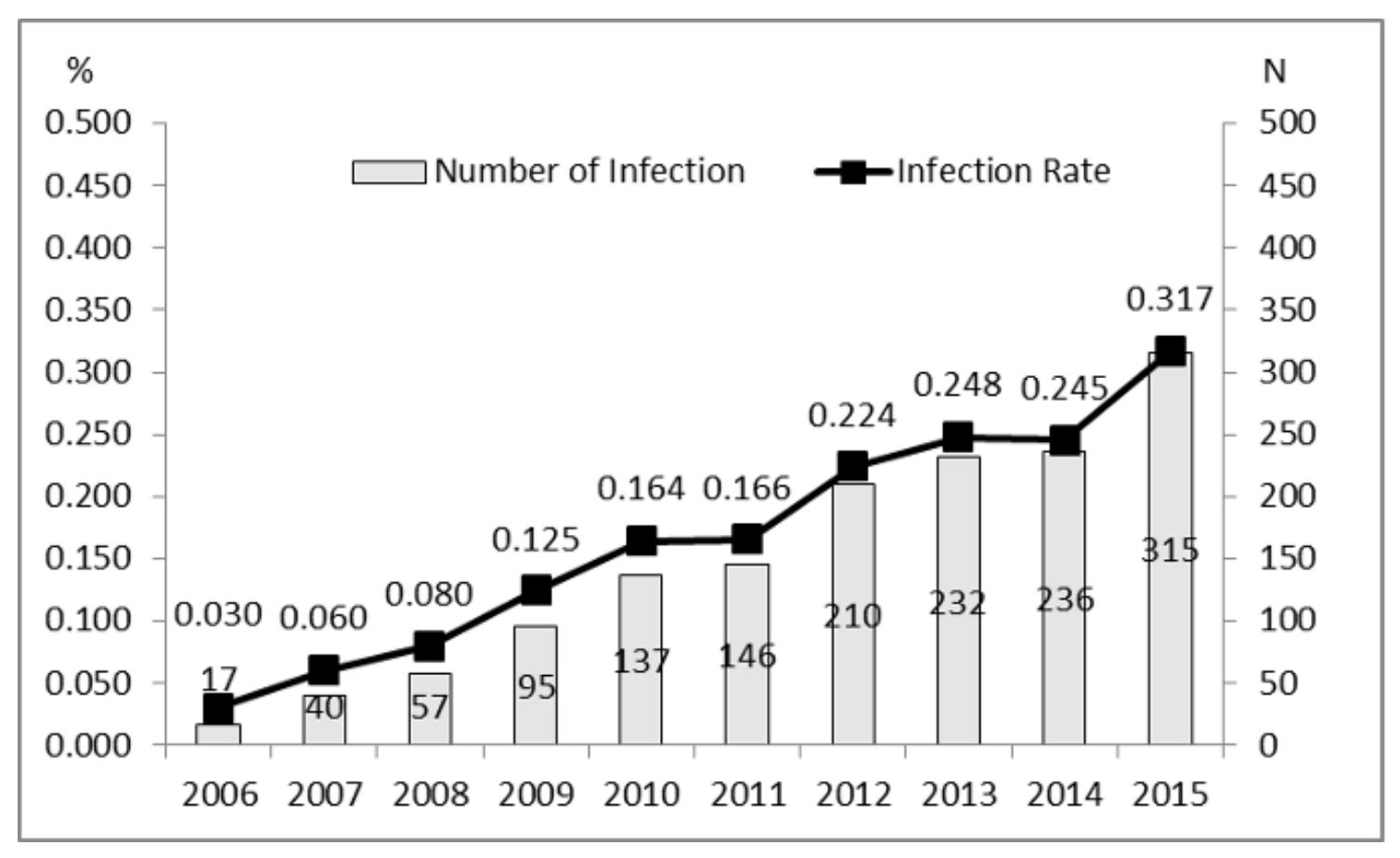
The rate of C. difficile infection has steadily increased from 0.030% in 2006 to 0.317% in 2015. The increased rate correlated to age (0.033% for <50 years, 0.421% for 70-79 years, and 0.758% for >80 years of age) and the Charlson comorbidity index score (0.048% for zero versus 0.378% for three or more points). It differed by the type of medical institution (0.270 % at referral hospitals versus 0.056 % at general hospitals and mental hospitals).
Conclusion
The rate of C. difficile infection in Korea is significant in patients with advanced age and disease severity. The results show that C. difficile infection trend has been increasing steadily in Korea.
Keyword
Figure
Reference
-
1. Bartlett JG. Clostridium difficile: history of its role as an enteric pathogen and the current state of knowledge about the organism. Clin Infect Dis 1994;18:S265-72.2. Pepin J. Valiquette L, Alary ME, Villemure P, Pelletier A, Forget K, et al. Clostridium difficileassociated diarrhea in a region of Quebec from 1991 to 2003: a changing pattern of disease severity. Can Med Assoc J 2004;171:466–72.3. Loo VG, Poirier L, Miller MA, Oughton M, Libman MD, Michaud S, et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile associated diarrhea with high morbidity and mortality. N Engl J Med 2005;353:2442-9.4. Kim YS, Han DS, Kim YH, Kim WH, Kim JS, Kim HS, et al. Incidence and clinical features of Clostridium difficile infection in Korea: a nationwide study. Epidemiol Infect 2013;141:189-94.5. Choi HY, Park S, Kim Y, Yoon T, Choi J, Choe B, et al. The epidemiology and economic burden of Clostridium difficile infection in Korea. Biomed Res Int 2015;2015:510386.6. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance servicenational sample cohort (NHIS-NSC), South Korea. Int J Epidemiol 2017;46:e15.7. Kim KH. Comparative study on three algorithms of the ICD-10 Charlson comorbidity index with myocardial infarction patients. J Prev Med Public Health 2010;43:42-9.8. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 2011;173:676-82.9. Martín-Loeches I, Diaz E, Vallés J. Risks for multidrug-resistant pathogens in the ICU. Curr Opin Crit Care 2014;20:516-24.10. Yoon YK, Park GC, An H, Chun BC, Sohn JW, Kim MJ. Trends of antibiotic consumption in Korea according to national reimbursement data (2008–2012): a population-based epidemiologic study. Medicine 2015;94:e2100.11. Kim D, Ahn JY, Lee CH, Jang SJ, Lee H, Yong D, et al. Increasing resistance to extendedspectrum cephalosporins, fluoroquinolone, and carbapenem in gram-negative bacilli and the emergence of carbapenem non-susceptibility in Klebsiella pneumoniae: analysis of Korean antimicrobial resistance monitoring system (KARMS) data from 2013 to 2015. Ann Lab Med 2017;37:231-9.12. Lee H, Yoon EJ, Kim D, Jeong SH, Won EJ, Shin JH, et al. Antimicrobial resistance of major clinical pathogens in South Korea, May 2016 to April 2017: first one-year report from KorGLASS. Euro Surveill 2018;23:1800047.13. Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2019. www.cdc.gov › threats-report › 2019-ar-threats-report-508 [Online] (last visited on 4 December 2020).14. Byun JH, Kim H, Kim JL, Kim D, Jeong SH, Shin JH, et al. A nationwide study of molecular epidemiology and antimicrobial susceptibility of Clostridioides difficile in South Korea. Anaerobe 2019;60:102106.15. Nicholas A, Kim YK, Lee WK, Selasi GN, Na SH, Kwon HI, et al. Molecular epidemiology and antimicrobial susceptibility of Clostridium difficile isolates from two Korean hospitals. PLoS One 2017;12:e0174716.16. Friedman ND, Kaye KS, Stout JE, McGarry SA, Trivette SL, Briggs JP, et al. Healthcareassociated bloodstream infections in adults: a reason to change the accepted definition of community-acquired infections. Ann Intern Med 2002;137:791–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Which is the Preferred Regimen for Non-Severe Clostridioides difficile Infection in Korea, Vancomycin or Metronidazole?
- Clostridioides Infection in Patients with Inflammatory Bowel Disease
- Association between Antibiotic Consumption and Incidence of Clostridioides difficile Infection in a Hospital
- Case of Pseudomembranous Colitis Caused by a Clostridioides difficile Infection Concomitant with Cytomegalovirus colitis Mimicking Ischemic Colitis
- Laboratory diagnosis of Clostridioides difficile infection: guidelines and status of practice in Korea