Endocrinol Metab.
2021 Dec;36(6):1201-1210. 10.3803/EnM.2021.1206.
Computed Tomography-Derived Skeletal Muscle Radiodensity Is an Early, Sensitive Marker of Age-Related Musculoskeletal Changes in Healthy Adults
- Affiliations
-
- 1Yonsei University College of Medicine, Seoul, Korea
- 2Division of Endocrinology, Endocrine Research Institute, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Urology, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2523489
- DOI: http://doi.org/10.3803/EnM.2021.1206
Abstract
- Background
A decrease in computed tomography (CT)-derived skeletal muscle radiodensity (SMD) reflects age-related ectopic fat infiltration of muscle, compromising muscle function and metabolism. We investigated the age-related trajectory of SMD and its association with vertebral trabecular bone density in healthy adults.
Methods
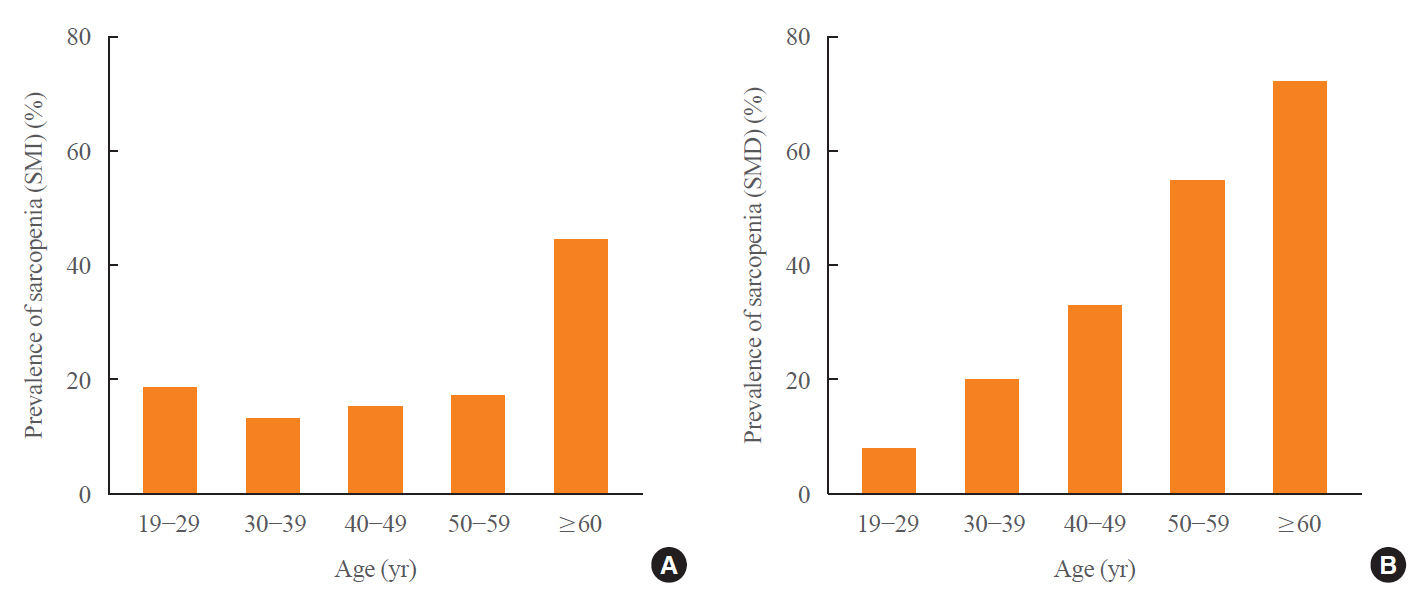
In a cohort of healthy adult kidney donors aged 19 to 69 years (n=583), skeletal muscle index (SMI, skeletal muscle area/height2), SMD, and visceral-to-subcutaneous fat (V/S) ratio were analyzed at the level of L3 from preoperative CT scans. Low bone mass was defined as an L1 trabecular Hounsfield unit (HU) <160 HU.
Results
L3SMD showed constant decline from the second decade (annual change –0.38% and –0.43% in men and women), whereas the decline of L3SMI became evident only after the fourth decade of life (–0.37% and –0.18% in men and women). One HU decline in L3SMD was associated with elevated odds of low bone mass (adjusted odds ratio, 1.07; 95% confidence interval, 1.02 to 1.13; P=0.003), independent of L3SMI, age, sex, and V/S ratio, with better discriminatory ability compared to L3SMI (area under the receiver-operating characteristics curve 0.68 vs. 0.53, P<0.001). L3SMD improved the identification of low bone mass when added to age, sex, V/S ratio, and L3SMI (category-free net reclassification improvement 0.349, P<0.001; integrated discrimination improvement 0.015, P=0.0165).
Conclusion
L3SMD can be an early marker for age-related musculoskeletal changes showing linear decline throughout life from the second decade in healthy adults, with potential diagnostic value for individuals with low bone mass.
Figure
Reference
-
1. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31.
Article2. World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992] [Internet]. Geneva: WHO;1994. [cited 2021 Nov 18]. Available from: https://apps.who.int/iris/handle/10665/39142.3. Goodpaster BH, Park SW, Harris TB, Kritchevsky SB, Nevitt M, Schwartz AV, et al. The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2006; 61:1059–64.
Article4. Yoo JI, Ha YC. Review of epidemiology, diagnosis, and treatment of osteosarcopenia in Korea. J Bone Metab. 2018; 25:1–7.
Article5. Dao T, Green AE, Kim YA, Bae SJ, Ha KT, Gariani K, et al. Sarcopenia and muscle aging: a brief overview. Endocrinol Metab (Seoul). 2020; 35:716–32.
Article6. Drey M, Sieber CC, Bertsch T, Bauer JM, Schmidmaier R; FiAT intervention group. Osteosarcopenia is more than sarcopenia and osteopenia alone. Aging Clin Exp Res. 2016; 28:895–9.
Article7. Huo YR, Suriyaarachchi P, Gomez F, Curcio CL, Boersma D, Gunawardene P, et al. Comprehensive nutritional status in sarco-osteoporotic older fallers. J Nutr Health Aging. 2015; 19:474–80.
Article8. Kawao N, Kaji H. Interactions between muscle tissues and bone metabolism. J Cell Biochem. 2015; 116:687–95.
Article9. Di Monaco M, Vallero F, Di Monaco R, Tappero R. Prevalence of sarcopenia and its association with osteoporosis in 313 older women following a hip fracture. Arch Gerontol Geriatr. 2011; 52:71–4.
Article10. Guerri S, Mercatelli D, Aparisi Gomez MP, Napoli A, Battista G, Guglielmi G, et al. Quantitative imaging techniques for the assessment of osteoporosis and sarcopenia. Quant Imaging Med Surg. 2018; 8:60–85.
Article11. Shen W, Punyanitya M, Wang Z, Gallagher D, St-Onge MP, Albu J, et al. Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (1985). 2004; 97:2333–8.
Article12. Hopkins JJ, Reif RL, Bigam DL, Baracos VE, Eurich DT, Sawyer MB. The impact of muscle and adipose tissue on long-term survival in patients with stage I to III colorectal cancer. Dis Colon Rectum. 2019; 62:549–60.
Article13. Caan BJ, Cespedes Feliciano EM, Prado CM, Alexeeff S, Kroenke CH, Bradshaw P, et al. Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol. 2018; 4:798–804.
Article14. Goodpaster BH, Kelley DE, Thaete FL, He J, Ross R. Skeletal muscle attenuation determined by computed tomography is associated with skeletal muscle lipid content. J Appl Physiol (1985). 2000; 89:104–10.
Article15. Miljkovic I, Zmuda JM. Epidemiology of myosteatosis. Curr Opin Clin Nutr Metab Care. 2010; 13:260–4.
Article16. Goodpaster BH, Krishnaswami S, Harris TB, Katsiaras A, Kritchevsky SB, Simonsick EM, et al. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005; 165:777–83.
Article17. Lentine KL, Kasiske BL, Levey AS, Adams PL, Alberu J, Bakr MA, et al. KDIGO clinical practice guideline on the evaluation and care of living kidney donors. Transplantation. 2017; 101(8S Suppl 1):S1–109.
Article18. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009; 150:604–12.
Article19. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 2008; 33:997–1006.
Article20. Lenchik L, Lenoir KM, Tan J, Boutin RD, Callahan KE, Kritchevsky SB, et al. Opportunistic measurement of skeletal muscle size and muscle attenuation on computed tomography predicts 1-year mortality in medicare patients. J Gerontol A Biol Sci Med Sci. 2019; 74:1063–9.
Article21. Heymsfield SB, Heo M, Thomas D, Pietrobelli A. Scaling of body composition to height: relevance to height-normalized indexes. Am J Clin Nutr. 2011; 93:736–40.
Article22. Schuck P. Assessing reproducibility for interval data in health-related quality of life questionnaires: which coefficient should be used? Qual Life Res. 2004; 13:571–86.
Article23. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016; 15:155–63.
Article24. Pickhardt PJ, Lee LJ, del Rio AM, Lauder T, Bruce RJ, Summers RM, et al. Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res. 2011; 26:2194–203.
Article25. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–96.
Article26. Derstine BA, Holcombe SA, Ross BE, Wang NC, Su GL, Wang SC. Skeletal muscle cutoff values for sarcopenia diagnosis using T10 to L5 measurements in a healthy US population. Sci Rep. 2018; 8:11369.
Article27. Kim HK, Kim KW, Kim EH, Lee MJ, Bae SJ, Ko Y, et al. Age-related changes in muscle quality and development of diagnostic cutoff points for myosteatosis in lumbar skeletal muscles measured by CT scan. Clin Nutr. 2021; 40:4022–8.
Article28. Nadaraya EA. On estimating regression. Theory Probab Appl. 1964; 9:141–2.
Article29. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–45.
Article30. Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008; 27:157–72.
Article31. Boutin RD, Yao L, Canter RJ, Lenchik L. Sarcopenia: current concepts and imaging implications. AJR Am J Roentgenol. 2015; 205:W255–66.
Article32. Hamrick MW, McGee-Lawrence ME, Frechette DM. Fatty infiltration of skeletal muscle: mechanisms and comparisons with bone marrow adiposity. Front Endocrinol (Lausanne). 2016; 7:69.
Article33. Hong N, Lee J, Ku CR, Han K, Lee CR, Kang SW, et al. Changes of computed tomography-based body composition after adrenalectomy in patients with endogenous hypercortisolism. Clin Endocrinol (Oxf). 2019; 90:267–76.
Article34. Goodpaster BH, Carlson CL, Visser M, Kelley DE, Scherzinger A, Harris TB, et al. Attenuation of skeletal muscle and strength in the elderly: the Health ABC Study. J Appl Physiol (1985). 2001; 90:2157–65.
Article35. Choi H, Hong N, Park N, Kim CO, Kim HC, Choi JY, et al. Computed tomography-derived skeletal muscle radiodensity predicts peak weight-corrected jump power in older adults: the Korean Urban Rural Elderly (KURE) Study. Calcif Tissue Int. 2021; 108:764–74.
Article36. Alajlouni D, Bliuc D, Tran T, Eisman JA, Nguyen TV, Center JR. Decline in muscle strength and performance predicts fracture risk in elderly women and men. J Clin Endocrinol Metab. 2020; 105:dgaa414.
Article37. Proctor DN, Melton LJ, Khosla S, Crowson CS, O’Connor MK, Riggs BL. Relative influence of physical activity, muscle mass and strength on bone density. Osteoporos Int. 2000; 11:944–52.
Article38. Blain H, Vuillemin A, Teissier A, Hanesse B, Guillemin F, Jeandel C. Influence of muscle strength and body weight and composition on regional bone mineral density in healthy women aged 60 years and over. Gerontology. 2001; 47:207–12.
Article39. Cawthon PM, Fullman RL, Marshall L, Mackey DC, Fink HA, Cauley JA, et al. Physical performance and risk of hip fractures in older men. J Bone Miner Res. 2008; 23:1037–44.
Article40. Figueiredo P, Marques EA, Gudnason V, Lang T, Sigurdsson S, Jonsson PV, et al. Computed tomography-based skeletal muscle and adipose tissue attenuation: variations by age, sex, and muscle. Exp Gerontol. 2021; 149:111306.
Article41. Yoon JK, Lee S, Kim KW, Lee JE, Hwang JA, Park T, et al. Reference values for skeletal muscle mass at the third lumbar vertebral level measured by computed tomography in a healthy Korean population. Endocrinol Metab (Seoul). 2021; 36:672–7.
Article42. Boutin RD, Lenchik L. Value-added opportunistic CT: insights into osteoporosis and sarcopenia. AJR Am J Roentgenol. 2020; 215:582–94.
Article43. Lee YS, Hong N, Witanto JN, Choi YR, Park J, Decazes P, et al. Deep neural network for automatic volumetric segmentation of whole-body CT images for body composition assessment. Clin Nutr. 2021; 40:5038–46.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Amount of Daily Protein Intake Is Not Associated with Skeletal Muscle Strength in Older Adults
- Effects of Muscles on Bone Metabolism—with a Focus on Myokines
- Association between energy intake and skeletal muscle mass according to dietary patterns derived by cluster analysis: data from the 2008 ~ 2010 Korea National Health and Nutrition Examination Survey
- The ability of panoramic radiography in assessing maxillary sinus inflammatory diseases
- Impact of Skeletal Muscle Mass on Metabolic Health